Fundus
Basics

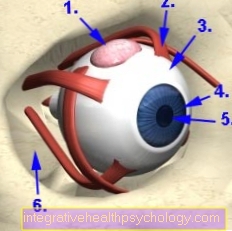
The back of the eye is the back part of the eyeball, which can be made visible when the pupil dilates medically. The Latin name for the fundus is Fundus oculi.
In order to be able to observe it more closely, one looks through the transparent glass body and can illuminate various structures, such as the retina (also known as retina), the optic nerve outlet (blind spot), arterial and venous vessels and the so-called yellow spot (macula lutea).
The retina develops from part of the forebrain and is central to actual vision. There are various light-sensitive photoreceptors on it. These are cells in which an electrochemical reaction takes place when light arrives, which is converted into an electrical signal and then passed on to the brain. There the visual impressions are then finally processed into visual information.
Cross-links between the photoreceptors also serve to enhance contrast in the retina.
The retina turns into a photosensitive and one light-insensitive Part divided. In the middle is the yellow spot (Macula lutea), which Point of sharpest vision, since this is where the density of photoreceptors is highest. Here are exclusively so-called cones, which are responsible for both daytime vision and color perception. A distinction is made between blue, red and green cones. In total, humans have around 6-7 million Coneswhich are predominantly located in the macular region.
Around the yellow spot are the 110-125 million rodresponsible for seeing at dusk or at night. This is because the messenger substance in the rods is about 500 times more sensitive to light than that in the cones. Vitamin A is of outstanding importance for the production of this messenger substance. A deficiency in this vitamin comes with it Impairments in twilight vision hand in hand.
The place where the extensions of all photoreceptors bundle and enter the brain is the optic nerve exit. There are no more light-sensitive cells there either, which is why you should take the Blind spot speaks.
The retina is supplied via arterial and venous vessels. However, pain-sensitive nerves are missing, which is why diseases of the retina are usually not perceived as painful.
Diagnosis

The examination of the fundus is an ophthalmoscope or ophthalmoscopy. There are two different procedures for this, one speaks of direct and indirect ophthalmoscopy.
In direct ophthalmoscopy, the ophthalmologist uses an ophthalmoscope (ophthalmoscope) that throws light onto the fundus and displays it at a 14 to 16-fold magnification. The doctor looks into the patient's right eye with his right eye and sees the fundus as an upright image, which is why this type of examination is also referred to as an “upright image”. The same applies to the left eye, but vice versa. This examination is easy to carry out and shows a relatively small portion of the fundus in high magnification. This allows the individual structures in it, such as the optic nerve outlet or individual vessels, to be assessed particularly well, but an overall view can only be obtained using indirect ophthalmoscopy.
In indirect ophthalmoscopy, the doctor holds a magnifying glass in front of the eye to be examined with an outstretched arm and a light source, such as a flashlight, with the other hand. With this type of examination, he sees the fundus as an upside-down image, which is why one speaks of the examination with the "inverted image". The magnification is significantly lower than with direct ophthalmoscopy, around 4.5 times. Therefore, this examination is better suited to get a complete view of the fundus and requires more practice on the part of the examiner.
With the help of the slit lamp examination, i.e. a binocular microscope, it is possible to examine both eyes at the same time.
If this is not possible, further examination options, such as an ultrasound examination, are available.
Diseases
The Diseases of the fundus can be very diverse and affect different structures. Diseases of the retina are called retinopathies.
A common disease of the retina is the dabetic retinopathy that can occur in the context of diabetes. It is the most common cause of premature blindness, as it can detach the retina or cause bleeding.It is therefore important for diabetics to go to regular ophthalmological examinations from the time the diagnosis is made and, if necessary, to undergo an operation.
In addition, the vessels supplying the retina can become too Vascular occlusions come. This often happens in patients with high blood pressure, diabetes, diseases of the cardiovascular system and in the context of glaucoma. The therapy of choice is to restore or improve blood flow.
Another clinical picture is that of retinal detachment (ablatio retinae). This can lead to visual impairments or even blindness if this is not treated adequately. The causes are very variable, for example injuries to the eye such as splinters in the eye or bruises can lead to it. The treatment can be carried out with a laser or, if the damage is larger, surgically.
The Retinal detachment is a less dramatic clinical picture, but can also lead to retinal detachment in the course of the disease.
With advancing age, age-related macular degeneration can finally occur, which is the most common cause of blindness in old age. The patients report a gradual deterioration in vision with a decrease in visual acuity. On the one hand, there is the possibility of laser treatment, as well as visual aids or supportive drug therapy.
Another group of diseases affecting the fundus is inflammation. It is important to recognize infections at an early stage and, if necessary, treat them with medication in order to avoid further consequential damage.
One condition that often affects young men is the Chorioretinopathia centralis serosa. This leads to visual loss of different sizes Accumulation of serous fluid between the photoreceptors. This clinical picture is associated with stressful situations and often heals spontaneously the first time it occurs.
There are also tumors in the back of the eye that can occur in all age groups. These can be both benign and malignant and should be removed and / or irradiated if possible.
Finally, there are also hereditary and congenital diseases of the retina, but these are usually associated with a very early onset of symptoms. Unfortunately, causal treatment is only possible in very few cases.