Palliative therapy
definition
Palliative therapy is a special therapy concept that can be used for terminally ill patients when no further measures can be taken that could lead to the patient being cured. Accordingly, it is a concept that accompanies patients at the end of their life and is intended to alleviate their suffering without being able to bring about a cure. The palliative therapy can also be used at the request of the patient if he does not want any further treatment measures, although theoretically there is still a chance of healing. Palliative therapy is made up of several areas, each of which aims to reduce the suffering of the sick to a minimum. Depending on the type of illness, pain therapies, psychotherapy, drug therapies and operations are used.

Who gets palliative therapy?
A palliative therapy is used in very sick people, whose suffering no longer through curative - That means leading to healing - measures can be treated. Accordingly, these are usually patients who are in the end-stage of a serious illness. Often these are cancer patients whose tumor has spread over a large area in the body. Other diseases, such as severe cardiovascular diseases or lung diseases, can worsen so much that palliative therapy is the last option. However, patients can also request palliative therapy if they no longer want any further potentially curative treatment measures - even if a cure has not yet been ruled out. The legal guardian of a patient who is no longer able to give consent himself can also decide on a palliative therapy concept in consultation with the doctors.
What is the goal of palliative therapy?
The aim of palliative therapy is to alleviate the symptoms of a patient who is terminally ill, or who no longer want any curative treatment measures, as much as possible and thus relieve him of the suffering. The focus is therefore on increasing the quality of life. Important components of palliative therapy are painkillers that are supposed to relieve the patient of his pain, an improvement or adjustment of the diet, psychological care if desired by the patient and other drugs, for example against shortness of breath or nausea. Since the patient should live with his illness as well as possible, operations, radiation and chemotherapy can also be part of palliative therapy if they can improve the patient's quality of life and prolong their survival. The disease is not cured, but the progression is slowed down and the course has a positive effect. Palliative irradiation of bone metastases can, for example, reduce pain caused by it and prevent bone fractures.
You can find more information about metastases on our website Metastases.
Palliative therapy for lung cancer
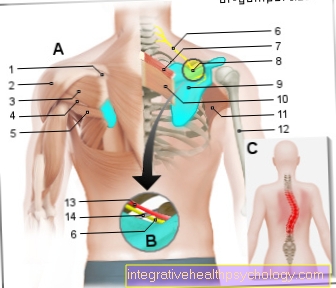
In many patients, lung cancer is only recognized at a very late stage, when no further therapy promises a cure. However, palliative therapy can restore a large part of their quality of life to these patients and often give them more life. It was shown that the earlier a palliative therapy concept was integrated into the treatment of the patient, the higher the overall survival and quality of life of the patient. For lung tumors that are localized in such a way that they interfere with the patient's breathing, various measures can be taken to improve the situation. For example, stents can be inserted into the airways. These are tubular wire or plastic meshes that are designed to keep the airways open at the point where they are compressed by the tumor. Radioactive substances can also be introduced locally in the immediate vicinity of the tumor, which curb further growth there. Of course, adequate pain therapy is also part of the palliative treatment concept for lung cancer. Painkillers can be administered directly to the spinal cord in tablet form, as a plaster or as a catheter. Since lung cancer often forms settlements in the bones, this can also cause unpleasant pain that should be treated. Not only conventional painkillers are used for this, but also Bisphosphonates. These are drugs that prevent bone loss and thus contribute to the stability of the damaged bones. In addition, bone metastases can be specifically irradiated, which also improves stability and pain.
For more information on lung cancer therapy, see our article Lung cancer therapy.
Palliative therapy for pancreatic cancer
Pancreatic cancer is one of the most aggressive and most difficult to treat tumor diseases. This is largely due to the fact that this disease is usually only diagnosed at a very advanced stage, when therapeutic concepts leading to a cure no longer work. In this situation, patients usually receive palliative chemotherapy with the active ingredient Gemcitabine, as this restricts tumor growth locally and can significantly improve the patient's quality of life. Pancreatic cancer often leads to pain, which should be countered with well-adjusted pain therapy. Tablets, drops, plasters and pain catheters can be used for this. In addition, pancreatic cancer can become problematic if it has grown to the point where it compresses the duct of the gallbladder, the gastric outlet or the duodenum. This can lead to a dangerous intestinal obstruction (Ileus) and bile build-up with jaundice (Jaundice) come. Palliative intervention can then help. To do this, stents - tubular wire or plastic meshes - are inserted into the constriction in order to keep the opening of the duct or the intestine open. In this way, the typical complications of pancreatic cancer can be prevented. The destruction of the pancreatic tissue also affects the patient's metabolism. Palliative therapy therefore also includes nutritional therapy with replacement of the important enzymes and vitamins, as well as - if necessary - diabetes treatment. If the gastric outlet has become more narrow, a feeding tube can be placed in the patient's intestine, through which he can continue to be fed. In addition, psychosocial care and drug treatment for accompanying symptoms such as nausea and anxiety are part of the palliative treatment concept for pancreatic cancer.
Causes, signs and much more information about pancreatic cancer can be found in our article Pancreatic cancer.
Palliative therapy for breast cancer
Breast cancer is curable in many cases today if the disease is detected early enough. Unfortunately, however, there are still patients in whom the disease is so advanced when the diagnosis is made that a cure can no longer be expected with conventional therapies. These patients should be referred to a palliative therapy concept at an early stage, as this can significantly improve their quality of life and lifespan. Palliative therapy for breast cancer often includes chemotherapy, which, although it no longer heals, can limit the local growth of the tumor and thus slow down the progression of the disease. Advanced breast cancer can develop into bone metastases. These often lead to severe pain in the relevant areas. Local irradiation of these metastases can help maintain the stability of the bone and reduce pain. In addition, drugs can be administered that inhibit bone loss - so-called Bisphosphonates. As a result, the patients regain a large part of their quality of life. In addition, adequate drug therapy and psychosocial care should be provided - if desired.
Read our article about this Breast cancer therapy.
Palliative therapy for prostate cancer
Palliative therapy for prostate cancer aims to alleviate the symptoms caused by the incurable disease as much as possible and to increase the patient's quality of life and lifespan as much as possible. If prostate cancer is very large, sooner or later it leads to an obstruction of the urinary tract. The patient then has problems urinating, which can lead to a build-up of urine as far as the kidneys and promote secondary infections and even life-threatening complications. These situations can be avoided through palliative interventions. For example, the removal of pathologically altered prostate areas can create more space for the urethra and prevent the urine outflow from being obstructed. Tubes can also be inserted into the urethra to prevent the urethra from being compressed by the tumor. Another alternative is urinary diversion using a urinary catheter, which can be placed both through the urethra and directly through the abdominal wall (so-called suprapubic catheter). Prostate cancer can form deposits in the bone, which in turn can cause pain and fractures. In the palliative therapy concept, these bone metastases can therefore be treated in the form of radiation, hormone treatment and / or chemotherapy. Bone stabilizing drugs such as Bisphosphonates can be used. Adequate pain therapy is also one of the most important pillars in the palliative treatment of prostate cancer. In addition, the patient should be offered psychosocial care.
Palliative therapy for liver cancer
Palliative therapy for liver cancer is used when the disease has progressed so far that a cure can no longer be brought about. It is important to treat or prevent the typical complications of the disease as well as possible. For example, advanced liver cancer can lead to obstruction of the bile duct depending on the location of the tumor. In order to prevent a build-up of bile and subsequent jaundice, a tube (Stent) into the bile duct to keep it open and to prevent compression by the tumor. Also stands with for several years Sorafenib an active ingredient available that can reduce the overall progression of the disease and improve the quality of life for patients.
Read more about the treatment of liver cancer in our article Liver cancer therapy.
Otherwise, adequate pain therapy, psycho-oncological and psychosocial care of the patient are also in the foreground in end-stage liver cancer.
Read more on the topic: End-stage liver cancer
Palliative therapy for colon cancer
In the case of colon cancer that can no longer be cured, a palliative therapy concept comes into question, which is intended to alleviate the patient's suffering and prevent complications from occurring. With colon cancer there is a risk that the colon will be obstructed by the local tumor growth and a life-threatening bowel obstruction will develop. It can therefore make sense to remove the tumor locally to prevent this. An artificial anus can also be used for palliative purposes (stoma) must be created to ensure that the chair is discharged. In addition, palliative chemotherapy can be used for end-stage colon cancer, which can slow the progression of the disease. In addition, individual pain therapy, psychosocial care, pastoral care and nutritional therapy are part of the palliative treatment concept for colon cancer.
For more information about colon cancer, see our article about Colon cancer.
Palliative medicine
Palliative medicine is a separate medical specialty that deals with the care of seriously ill patients who can no longer receive curative treatment. The patients are often looked after by a so-called palliative team, which is made up of people from various professional groups who work in a multidisciplinary manner in order to be able to meet the individual needs of each patient as best as possible. A palliative care team includes, for example, doctors, nurses, psychologists, social workers, physiotherapists, nutritionists and pastors. The focus is on increasing the quality of life of patients with limited life expectancy without concentrating purely on extending their lives. The suffering of the patients should be alleviated as much as possible in order to allow them the most dignified remaining life possible. In Germany, palliative medicine was established in 2003 as a separate additional training for doctors.
For more information on palliative care, read our article Palliative medicine.