The pseudoradicular syndrome
definition
Pseudoradicular syndrome is a condition in which muscles and joints do not work together properly. This often causes pain in the back, but also in the arms and legs.
For those affected, these feel like nerve pain, which can occur, for example, in a herniated disc. Hence the name pseudoradicular syndrome: it acts as if the complaints were leaving the nerve roots (lat.radix) out.
However, there is no damage to the nerves in the disease.

The reasons
The cause of the pseudoradicular syndrome is usually a malfunction of muscles and joints. The pain in the disease comes from the spine. This consists of many individual vertebral bones, each of which is connected to one another by a joint.
The spine is usually stabilized by the holding muscles of the back. The muscles are particularly active when moving.In most cases, however, these muscles are no longer sufficiently developed to fully protect the spine.
In this way, individual vertebral bodies can easily be tilted against each other and get stuck in position, especially after unusual movements. The body notices that something is wrong and tries to stabilize the affected part of the spine by tensing the muscles.
This muscle tension then usually triggers the pain and can spread reflexively.
Depending on where the problem is on the spine, neighboring parts of the back are affected, but the tension can also continue in the arms and legs. Anyone who has suffered brief irritation of the nerves due to a herniated disc, an accident or other causes, their brain has more or less "learned" the nerve pain.
Therefore, the pain associated with pseudoradicular syndrome is often perceived as real nerve pain in these individuals.
Read more about the topic here: Causes of back pain.
Appointment with a back specialist?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The spine is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
The treatment of the spine (e.g. herniated disc, facet syndrome, foramen stenosis, etc.) therefore requires a lot of experience.
I focus on a wide variety of diseases of the spine.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
The accompanying symptoms
Accompanying symptoms in pseudoradicular syndrome are the radiating pain and muscle tension.
On the one hand, the pain is located directly on the affected area of the spine, and the pain also radiates to other parts of the back. For example, if the lumbar spine is affected, the thoracic spine above it has to take on more work, whereupon the tension problem shifts to the thoracic spine. If the signal for tensioning the muscles is given in the spine, this information can also spread to the arms and legs.
With pseudoradicular syndrome in the lumbar vertebrae area, usually only the legs are affected. If the syndrome is higher up, in the cervical or thoracic spine, the tension is more likely to radiate to the arms.
Especially with problems in the thoracic spine, breathing can be difficult because the entire chest has to move against the tension.
Other accompanying symptoms are discomfort in the skin. The cutaneous nerves are also controlled by the spinal cord. Irritations on the spine can also briefly irritate the skin nerves.
The strength test in arms and legs provides a clear distinction between pseudoradicular syndrome and actual nerve damage. Loss of strength can only occur due to nerve damage and is not an accompanying symptom of pseudoradicular syndrome.
What is pseudoradicular pain?
Pseudoradicular pain is pain that feels like nerve pain. However, these do not actually assume nerve damage.
Instead, a dysregulation between the muscles and joints of the spine leads to severe tension. This can lead to pain that is very similar to that of nerve damage.
Just like nerve pain, pseudoradicular pain pulls along a muscle group into the arms or legs.
Read more on this topic at: Pseudoradicular pain
Why is it most common in the lumbar spine / lumbar region?
In addition to our cervical spine, the lumbar spine is the weakest point of the back. Here the weight of the entire upper body rests on the spine.
On the one hand, the lumbar spine has to support the upper body; on the other hand, there is a connection between the upper body, the pelvis and the legs, so that pronounced stabilization by the lumbar spine and the muscles located there is required, especially when walking.
Our current lifestyle means that we usually spend several hours at a time sitting. Often the posture of the back is crooked, which can lead to tension in the entire back muscles.
However, the lumbar spine is particularly affected. Here is the stabilizing contact between the fixed seat and the movable upper body, so that particularly good stabilization is required at this point. As a result of this inactive lifestyle, the back muscles are also no longer sufficiently trained to adequately stabilize and support the spine in all situations. This is why unfamiliar movements or new physical stress often lead to an imbalance in muscle work.
The resulting dysregulation of muscles and joints triggers the pseudoradicular syndrome. And since the lumbar region usually bears the greatest burden, these dysregulations occur particularly frequently there.
The diagnosis
The diagnosis of all types of back pain consists initially of an anamnesis, in which the doctor asks the person concerned about the exact symptoms. The most important thing here is whether there is an accident or an infection, as this can indicate an injury to the spine.
This is followed by the examination, in which the range of motion and nerve damage can be checked. For those who show no evidence of spinal or nerve damage, this diagnosis is sufficient.
Imaging (X-ray, MRI, CT) can be performed if serious damage is suspected. Pseudoradicular syndrome can be accompanied by abnormal sensations in the skin.
A detailed assessment by a neurologist is sometimes necessary for a more precise diagnosis of these symptoms.
Read more about the topic here: Diagnosis of spinal disease.
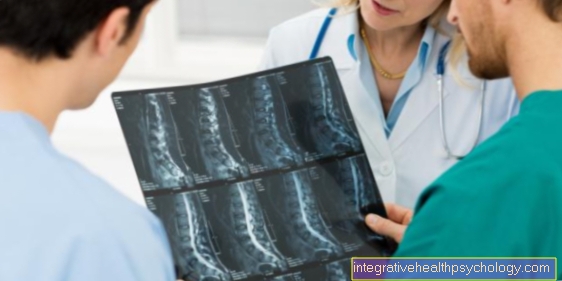
MRI for imaging
The MRI, also called nuclear spin, is the most suitable imaging method for assessing soft tissues, organs and muscles. Therefore, an MRI is used if damage to the spinal cord or nerve roots is suspected.
Slipped discs can also be assessed well in the MRI. In pseudoradicular syndrome, the MRI is used to diagnose exclusion. Structural damage that could explain the symptoms of the disease should be excluded.
Find out more about the topic here: MRI of the spine.
X-ray for imaging
The X-ray is a simple and quick procedure with which particularly bony structures can be assessed well. If pseudoradicular syndrome is suspected, bony defects in the spine should usually be excluded as the cause of the symptoms.
Usually you wait around two to four weeks to see whether the pain goes away with exercise and pain therapy. If this is not the case, causes other than pseudoradicular syndrome must be investigated.
An X-ray image serves as a good orientation for the bony structure.
CT as imaging
The CT is used in pseudoradicular syndrome as well as the X-ray image when bony defects are to be excluded. In contrast to the X-ray image, the CT images can be used to understand in three dimensions which structure is located in the body. Therefore, if the X-ray findings are unclear, CT is the next choice.
In addition, softer structures such as the spinal cord and nerves can also be assessed (although not as well as in an MRI). In the case of pseudoradicular syndrome, CT also serves to rule out serious structural diseases.
The treatment
Therapy for pseudoradicular syndrome is usually conservative at first. The most important component is physiotherapy, which is supposed to relieve the tension in the back muscles. In the course of this therapy can move from relaxation to targeted muscle building, which should prevent the symptoms from occurring again.
In order to improve mobility at the beginning of the therapy and to get the pain symptoms under control, pain medication such as ibuprofen or Novalgin are usually prescribed. This makes everyday life easier for those affected and at the same time leads to more coordinated mobility of the spine. In pain, reflex muscle tension leads to incorrect movement patterns, which can further aggravate the symptoms.
In the long term, affected people need to incorporate regular movements and strengthening exercises into their everyday lives to prevent relapse. Achieving this routine is also part of the therapy for pseudoradicular syndrome.
More invasive measures can be useful at the beginning of the symptoms. This includes chiropractic therapy, for example, in which doctors with additional training as chiropractic therapists can solve the small tilts in the vertebral joints. Without the resulting blockages in the spine, the symptoms usually improve within a few days.
Wheals, in which local anesthetics are injected under the skin, can also relieve tension. Afterwards, however, exercise therapy is necessary, which those affected then continue independently.
More information on the topic Therapy of back pain you'll find here.
The duration
The acute severe pain associated with pseudoradicular syndrome should be adequately ceased with adequate pain treatment within a few weeks. If the blockages in the vertebral joints can be resolved, the symptoms are usually significantly improved after a week.
Nevertheless, the back is very susceptible to further tension for a long time and, as a result, to new pseudoradicular pain.
The great danger with such back pain is chronification. If you do not consistently do training exercises for your back, the pain can stick or recur and cause problems for years.
Also read the topic: Back Pain - What Can I Do?
Prognosis
The prognosis for pseudoradicular syndrome is largely dependent on the initiative of those affected.
Scientific studies have shown that people who take responsibility for treating their disease themselves have significantly fewer problems with pseudoradicular pain. This includes conscious and regular exercise as well as targeted training for the back muscles. With consistent implementation, the pseudoradicular syndrome can be avoided in the long run.
On the other hand, those who tend to deal passively with the disease, relying on chiropractic, wheals and painkillers, may have to struggle with the symptoms for a lifetime. However, the disease is not dangerous, so that although it affects the quality of life, it does not affect the lifespan.