Pericardial effusion
introduction
A pericardial effusion is an enlarged one Fluid build-up (from about 50 ml) in the pericardium. In order to be able to understand this well, one should first consider the anatomical relationships in the mediastinum (space in the middle of the membrane).
The heart lies in the mediastinum inside the pericardium (= Pericardium). The pericardium consists of two parts: On the one hand, the outer one Pericardium fibrosumwhich at the bottom with the diaphragm is connected and on the other hand from the inside Pericardium serosum. The pericardium serosum itself consists of two leaves, the so-called "Laminae". The outer of these two leaves is called the lamina parietalis pericardii and is firmly fused with the pericardium fibrosum. The inner leaf is called Lamina visceralis pericardii and, by definition, is also the outermost layer of the heart (= Epicardium).

Between these two sheets of the pericardium there is a gap in which there is usually a small amount of fluid, so that the two sheets can easily slide past each other when the heart moves and the heart beats. A healthy amount of fluid is around two to ten milliliters. If the water in the pericardium begins to press on the heart and compress it and thus hinder the heart's actions, this is called pericardial tamponade or pericardial tamponade.
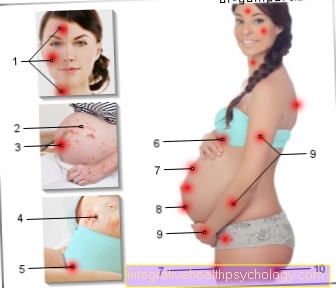
Symptoms
At a small effusion become common no complaints perceived. If the effusion slowly increases over time ("chronic effusion“), Symptoms are usually noticeable from an amount of 300 ml.
These can be made from shortness of breath (Dyspnea), high blood pressure (hypertension) or Racing heart (Tachycardia) consist. In addition, those affected usually feel physically weak and occasionally feel pain behind the sternum.
The big ones Neck veins (Jugular veins) can also jammed be. Other symptoms that the doctor can detect include soft heartbeats and possibly a pericardial rubbing when listening with the stethoscope, as well as a Enlargement of the liver (Hepatomegaly). Water in the stomach (Ascites) can also occur.
If pericardial effusion occurs within a short time (acute effusion) even small amounts (around 150 to 200 ml) can cause severe symptoms that can lead to Heart attack strongly resemble. An acute occurrence with rapid development can end in cardiogenic shock (pump failure of the heart), which is why an acute effusion is always one emergency and must be treated accordingly.
therapy
In therapy generally persist three types of treatment optionsthat can be combined depending on the cause.
First of all, can conservative are proceeded. Depending on the cause, this will be Antibiotics (for infections), Glucocorticoids or Anti-inflammatory drugs (anti-inflammatory drugs). When there is pain also come Painkiller like acetylsalicylic acid (corresponds to Aspirin®) for use.
The second option consists of the Puncture of the pericardium. Here is under ultrasound control Drained fluid from the pericardium with a hollow needle.This is usually done in the case of large effusions or if there is any suspicion that the heart is starting to compress.
Operational measures are mainly carried out for "contaminated" effusions, for example when caused by a trauma There is blood in the pool of fluid or bacteria have infected the effusion. Here is an operational one drainage introduced. The drainage insert is also a treatment option for effusions that keep recurring (so-called chronically recurrent effusions).
Puncture of the pericardium
The pericardial puncture is used to tap into the pericardium Aspirate liquid. In the case of acute pericardial effusions, this is carried out immediately as an emergency.
On the one hand, the heart should be relieved, on the other hand, the pericardial water (Pericardial fluid) for possible pathogens, inflammatory or tumor cells and possibly for the root cause to close the pericardial effusion.
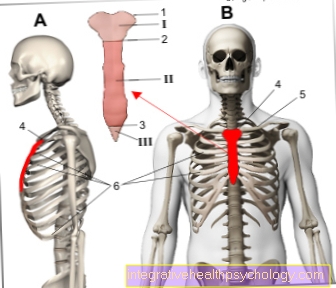
The pericardial puncture is performed by the doctor while monitoring the heart function, circulation and breathing. A general anesthetic is mostly not necessary, however will Sedatives or sleeping pills administered and the puncture site locally anesthetized. The needle is usually inserted below the breastbone (sternum) and is carried out under ultrasound control. In the case of larger effusions, a drain can be placed within the same procedure, which leads the pericardial water permanently to the outside.
As a rule, the procedure is well tolerated, but complications can be inflammation in the area of the puncture site, Cardiac arrhythmias or injuries to the surrounding tissue occur.
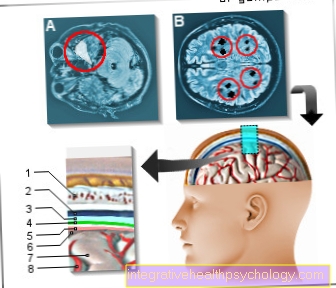
Echo and EKG
At a Echocardiography (informally often as "Heart echo“Denotes the heart and the bloodstream sonographically (= by means of Ultrasonic) shown. The echocardiography belongs together with the EKG to the most important examinations of the heart. A great advantage of this examination is that it can be carried out without surgery, ie "non-invasively".
With the Echocardiography of the heart, a pericardial effusion can be detected quickly and usually reliably. In addition, echocardiography can Extent of effusion be assessed so that further measures can be better assessed. Furthermore, an echocardiography can show how much blood the heart pumps into the body and whether the heart walls are moving properly. Narrowed atria indicate cardiac tamponade.
The EKG records the sum of the electrical voltages of all Heart muscle fibers and thus serves to assess the heart muscle function. If this is restricted by a pericardial effusion, this can be recognized using an EKG.
Non-invasive methods also include making one X-ray image. With pericardial effusion there is the Heart silhouette enlarged and the heart has a so-called buckbag shape.