Diagnosis of osteoarthritis
How is osteoarthritis diagnosed?
The Diagnosis of osteoarthritis is mostly from the clinical picture provided by the doctor. If the patient comes to the doctor and complains of pain in the joints that are often affected:
- Finger joints (finger osteoarthritis)
- Toe joints (toe joint arthrosis)
- Hip joints (hip arthrosis)
- Shoulder joints (shoulder joint arthrosis)
- Knee joints (knee osteoarthritis)

the suspicion of osteoarthritis of the corresponding joint must be made. The doctor (usually a specialist in orthopedics) will usually have an X-ray taken after the patient interview and physical examination.
The physical diagnosis / examination of the patient consists of the inspection of the relevant joints.
This checks whether the joint is swollen or deformed and whether the skin is red.
This is followed by the physical examination which consists of touching the joint.
In addition, the doctor moves the patient's joint and pays attention to the pain indicated by the patient, as well as to blockages and movement restrictions.
The diagnosis “osteoarthritis” can be made on the basis of several factors.This includes a physical examination by the doctor, imaging tests (e.g. X-ray, CT and MRI) and the examination of the patient's blood. Arthroscopy is also used to diagnose osteoarthritis.
When making a diagnosis, it must always be asked whether the family is already familiar with the disease.
If this is the case, the likelihood that the affected patient will suffer from osteoarthritis increases.
One of the most important aspects is the specific questioning of the doctor about the type of pain. With osteoarthritis, the pain often occurs after a long period of rest, i.e. in the morning (morning stiffness).
In addition, the doctor should ask specific questions to rule out excessive stress as a cause of pain and swelling of the joints.
Typical changes can be seen in the x-rays of a joint with osteoarthritis.
These include a narrowing of the joint space and a thickening of the bone under the cartilage. In addition, the bone has formed runners (so-called "osteophytes")') and cysts can be seen in the bone itself. Often, bone misalignments can also be identified, which can either be a consequence or cause of the osteoarthritis.
As an alternative to the X-ray image, an ultrasound can also be performed to diagnose the joint.
In terms of its accuracy and differentiation, however, it is subject to x-rays, since apart from the narrowing of the joint space, none of the above-mentioned signs are usually seen on ultrasound.
Magnetic resonance tomography, which is also gaining in importance in the diagnosis of osteoarthritis, is far clearer. However, it is mostly not used for initial diagnosis.
Rather, this is used for a more detailed examination, provided that the X-rays carried out do not provide a clear indication of osteoarthritis.
The MRI can include also represent nerve and muscle involvement that can cause pain.
Read more about this under: Procedure of an MRI, Is an MRI harmful?
Appointment with a hand specialist?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
In order to be able to treat successfully in orthopedics, a thorough examination, diagnosis and a medical history are required.
In our very economic world in particular, there is too little time to thoroughly grasp the complex diseases of orthopedics and thus initiate targeted treatment.
I don't want to join the ranks of "quick knife pullers".
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me at:
- - orthopedics
14
Directly to the online appointment arrangement
Unfortunately, appointments can only be made with private health insurers. I ask for understanding!
Further information about myself can be found at -
X-ray signs of osteoarthritis
A more reliable indication of osteoarthritis is usually only an X-ray of the affected joint. So there are four classic signs that the X-ray should show:
1) Diagnosis of narrowing of the joint space: joints that are over or incorrectly stressed wear out unevenly due to the movements carried out. The joint space becomes narrower; this narrowing can be seen in the X-ray image through two closely spaced bone edges.
2) Diagnosis of subchondral sclerotherapy: if the worn joint continues to be improperly loaded, it tries to replace the worn joint space in some way. This should enable an alternative stability of the joint. Shortly below the articular cartilage, a bone-like material called subchondral sclerosis spreads. This process is accompanied by:
3) so-called rubble cysts, the third radiological diagnosis of osteoarthritis.
4) So-called osteophytes, some of which can also be seen in the X-ray image. These indicate an increased bone formation process. The four signs just mentioned are typical and usually occur in severe osteoarthritis. However, they can also be missing (e.g. in stage 1, see stages of osteoarthritis).
Only half of the patients with radiological signs of osteoarthritis complain of pain.
MRI

The articular cartilage, joint capsule and joint effusions cannot be shown directly in a conventional X-ray image. Therefore, in some cases, additional imaging tests may have to be used.
A magnetic resonance tomography examination (short: MRI) is also known as magnetic resonance imaging or magnetic resonance imaging.
It is often used for early detection or to rule out osteoarthritis.
The advantage of an MRI examination compared to X-rays or computed tomography is that no X-rays are used in MRI.
The detailed representation of the painful joint in the MRI is carried out by means of the electromagnetic measurement of the different water content in the various tissues. For this reason, joints with water-containing cartilage, synovial fluid and mucous membrane can be shown particularly well with an MRI examination. Magnetic resonance imaging is therefore superior to a CT image or an X-ray image in the event of a ligament injury (e.g. a cruciate ligament tear) or an injury or change in the articular cartilage.
An MRI scan should not be performed if the person has a pacemaker, cochlear implant, drug pump, or metal splinters. Even in the first three months of pregnancy (Read more about this: MRI during pregnancy - is that dangerous?), If you are intolerant to the contrast agent, if you have certain kidney diseases or allergies, an MRI cannot be performed.
Read more about this: MRI for claustrophobia - what options are there ?, MRI clothing - what should I wear?
CT
With the help of a computed tomography (abbreviated CT), the bony structures of a joint can be shown particularly well. Computed tomography is based on different X-ray absorption in the tissue.
The different absorption is recorded by a computer and then converted into very detailed sectional images.
A CT scan is mainly used when a broken bone is suspected (Fractures) used. In the context of osteoarthritis, a CT scan can provide important information about changes in the bones that are often difficult to see on X-rays. In addition, a CT examination can be used to make a statement about bone remodeling processes that result from the load distribution.
In principle, however, the CT examination plays a subordinate role in the diagnosis of osteoarthritis and is used more for specific questions about the bones (e.g. broken bones, bone tumors).
A CT scan is contraindicated in pregnancy. When using iodine-containing contrast media, it should also not be carried out in the case of thyroid cancer or allergies to iodine-containing contrast media.
Examination of the blood
In contrast to acute inflammation in a joint (arthritis), there are no special markers in the blood that can be used for diagnosis in osteoarthritis.
However, the arthritis can be excluded by the blood test. Other diseases of the joints, such as rheumatoid arthritis, must also be excluded.
Only the acute phase of osteoarthritis can be detected in the blood through increased inflammation values, such as the rate of sedimentation (BSG).
Diagnosis of osteoarthritis of the wrist and finger joints
When looking at (inspecting) the hand, swelling (due to an effusion in the joint), reddening or overheating of the affected joints may be noticed.
All finger joints as well as the wrist can be affected. However, it can also be the case that none of these aspects are noticeable despite existing illnesses.
Subsequent palpation of the hand can cause tenderness over the affected joints. However, this is also not a mandatory criterion.
The doctor also checks the mobility of the joints. This is often limited in osteoarthritis. In order to diagnose osteoarthritis, it is usually necessary to take x-rays of the hands in order to be able to precisely identify typical signs of changes in the bony structures.
Read more on the topic: Finger osteoarthritis
Diagnosis of knee osteoarthritis
When diagnosing knee osteoarthritis, too, the first step is to listen to the patient's medical history and to draw the right conclusions from it. In addition to the general symptoms such as morning stiffness and pain, these patients often report discomfort when climbing stairs.
Misalignments such as Knock-knees or bow-legs can lead to knee osteoarthritis and must be assessed by a doctor. Other diseases that can lead to these symptoms (e.g. hip osteoarthritis) must also be excluded. For further diagnosis, an x-ray of the knee is then made to assess the extent of the bony changes.
This is often done in conjunction with MRI images of the knee, as this allows the cartilage to be better visualized.
If the diagnostic options mentioned do not provide sufficient results, a jointoscopy can be considered. However, since this involves a comparatively high risk, it is often used not only for diagnosis, but also for therapy.
Read more on the subject at: Knee osteoarthritis
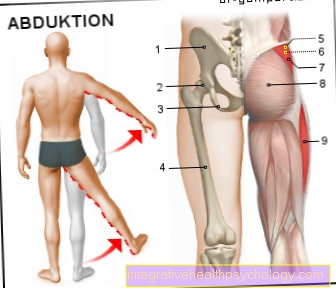
Diagnosis of hip arthrosis
A patient with a Hip osteoarthritis is often noticed by the fact that he thinks of it changed gait pattern shows. You can usually see to relieve the affected side a limp and an outwardly turned foot.
The palpation by the doctor is mostly on a particular one Pressure point above the groin painful. Other diseases, such as a Femoral head dysplasia should be excluded. Here, too, an X-ray should be taken to confirm the diagnosis. Other imaging methods are usually not necessary.