Erysipelas
definition
Erysipelas is a common, acute infection (inflammation) in the lymphatic spaces of the skin. This inflammation spreads through the lymph vessels. It is caused by bacteria (see below). The entry point for these bacteria is injuries to the skin. The pathogens can let in deep cracks (rhagades) or other injuries.

Causes of Erysipelas
An erysipelas is caused by bacteria. These bacteria are called streptococci.
Strepptococcus pyogenes is the most common pathogen. Staphylococci (Staphylococcus aureus = Staph. Aureus) can also rarely be the trigger. Staph. aureus is a germ that occurs physiologically on the skin. It occurs naturally and in every person, for example, in the armpit, the forehead-hair line or in the nasal vestibule.
The erysipelas occurs more frequently in immunocompromised patients, i.e. especially elderly and sick people as well as people with an immunodeficiency (e.g. HIV infection).
Symptoms of the erysipelas
There is a swelling at the entrance gate that is red and burning. Usually this area is also overheated.
These changes in the skin are always sharply delimited and can also be accompanied by the formation of blisters. The Skin is tense and shines. In addition to the localized pain, itching (Skin itches) consist.
Within hours, the inflammation spreads along the lymph vessels (flame-like and irregular). Healing begins from the center.
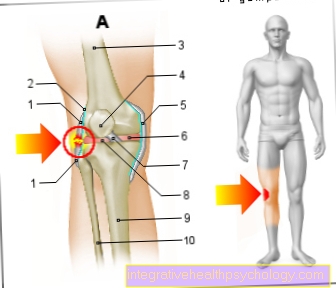
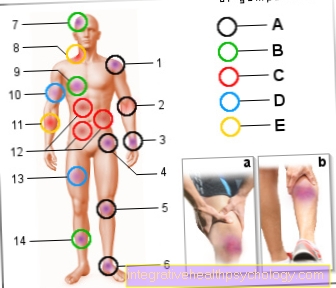
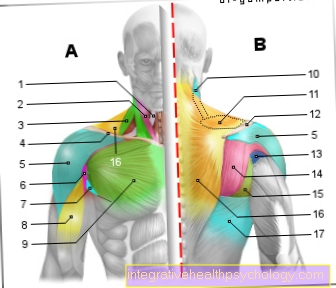
Usually this disease occurs on Lower leg on. In the case of facial involvement, where the connective tissue is looser, a rather diffuse reddening and swelling can be identified. The sharp border like on the lower leg is missing.
With the onset of the erysipelas (wound rose) or sometimes before it comes to general symptoms such as Fever, chills, and nausea.
Small injuries, which could have served as a gateway, may still be visible.
Localization of an erysipelago
Erysipelas on the face
In addition to the most common localization of erysipelas on the legs, this bacterial skin infection often also occurs on the face and is then referred to as a facial rose (ATTENTION: risk of confusion with a herpes zoster infection on the face, which is also often referred to as a facial rose).
The cause and mechanism of erysipelas on the face are the same as those on the legs. The entry portal often includes minor injuries in the area of the nose or mouth (e.g. small cracks in the area of the nostrils or corners of the mouth), small cuts in the facial skin (e.g. due to shaving) or opened pimples.
The symptoms (crimson, limited, scaly skin area, signs of inflammation, fever, pain, possibly blistering, etc.) are the same as with all other erysipelas, the lymph nodes, which can be affected and swollen in an erysipelas on the face, are usually found here in the area of the neck, lower jaw or ear.
An immediate start of antibiotic therapy is even more important in the case of erysipelas on the face than in other affected parts of the body, as life-threatening complications are feared. These include, for example, the involvement of the eye socket and the resulting risk to eye function, a blood clot in the cerebral veins (sinus vein thrombosis) or an inflammation of the meninges and thus an infection in the brain.
Erysipelas on the ear
In the case of erysipelas on the ear, the skin and subcutaneous tissue of the auricle are primarily affected, and the inflammation can also spread to the earlobe and the skin of the face immediately adjacent to the ear.
The cause of the erysipelas is also here the penetration of bacteria (group A streptococci) through small skin defects of the ear, the main symptoms being strong reddening, warming, painfulness and swelling of the auricle with accompanying fever, possibly swelling of the lymph nodes in the ear region and a general one Are feeling sick.
It is important to examine the external auditory canal and the middle ear as part of the diagnosis in order to determine whether the inflammation has spread in good time.
In addition to co-infection of the middle and / or inner ear, erysipelas of the ear have the same life-threatening complications as facial serysipelas (meningitis, cerebral vein thrombosis, inflammation of the eye socket). It is therefore also true here that the immediate initiation of an adequate antibiotic therapy is essential.
Complications of an erysipelas
If the disease is particularly severe, blisters may form within the affected area.
This is called medically bullous erysipelas (bulla = bladder).
If there is bleeding, the disease is called hemorrhagic erysipelas (heme = red blood pigment).
The most severe form is the gangrenous erysipelas (gangrene = disease caused by bacteria that causes individual parts of the body to “rot”).
Another complication is the tendency to relapse, i.e. erysipelas always occur.
The recurrences often occur in the same place. The recurrences can cause the lymphatic tract to stick together, causing lymphedema.
Lymphedema is the swelling that is caused by the transfer of lymph fluid into the surrounding tissue.
You might also be interested in the topic: Gangrene
diagnosis
To diagnose the Erysipelas mainly the symptoms and the appearance of the disease are considered.
The typical combination of swelling, reddening, warming and sharp delimitation at the predilection sites described above (especially the lower legs) hardly allows any other diagnosis.
Also certain Laboratory values can be helpful.
Most of them are Leukocytes (white blood cells) increases that BSG (Sedimentation rate) and that CRP (C-reactive protein, CRP value) extended.
All three are signs of inflammation. However, the values are also very unspecific. They are also increased in other types of inflammation (e.g. Appendicitis or flu-like infections).
If you suspect an erysipelas, you shouldn't ignore the search for the entrance gate.
Therapy and antibiosis of erysipelas

When the first signs of erysipelas appear, adequate therapy should be initiated as quickly as possible in order to avoid serious complications (such as lymphatic congestion, phlebitis, blood poisoning, kidney inflammation, etc.) in the course.
The therapy that every attending physician usually resorts to first - the so-called drug of choice - is the administration of high doses of antibiotics. This is an antibiotic from the group of penicillins or cephalosporins that, depending on the severity of the disease, is given either via the vein (iv; then usually in the hospital) or as a tablet (orally; as an outpatient therapy at the family doctor) . Since in most cases these are group A streptococci (Streptococcus pyogenes) and these are normally sensitive to penicillin, should this antibiotic contain and combat the erysipelas. If the patient is allergic to penicillins or if, in exceptional cases, there is resistance to penicillin in the bacteria causing the problem, then erythromycin or clindamycin is used. If there is a suspicion that other pathogens are involved in the infection in addition to the classic erysipelas bacterium (mixed infection, e.g. with Staphylococcus aureus), a cephalosporin is more likely to be used. The antibiotic should be taken for about 10-14 days or given via the vein, even if the symptoms improve significantly after just a few days.
In addition to antibiotic therapy, pain relievers and antipyretic agents (such as ibuprofen, paracetamol) can be given to relieve accompanying symptoms of the erysipelas. In addition, the part of the body affected by the erysipelas should be moved as little as possible, so that in most cases bed rest is even prescribed. Applying a splint and elevating it can also be useful if the erysipelas occurs on an arm or leg. In addition, cooling the diseased area has an additional pain-relieving effect and reduces the swelling.
Since immobilization or bed rest increases the risk of a blood clot (thrombosis) developing in the veins, thrombosis prophylaxis may be necessary from the outset (administration of a blood-thinning, anticoagulant agent). Putting on compression stockings or a compression bandage after the affected area of the body has declined for the first time can also prevent fluid from accumulating in the tissue and promote the return of blood in the veins. In addition to acute treatment, it is also important to find the entry point for the erysipelas pathogens (skin injuries), which should be made to heal as quickly as possible.
course
In people with a strengthened immune system and the appropriate antibiotic treatment, the erysipelas usually heals well.
Nevertheless, the erysipelas / wound rose must always be taken seriously, as complications can quickly arise. There is then the risk of Phlebitis, or even the Blood poisoning (sepsis).
If the bacteria spread in depth, life-threatening phlegmon can occur. Phlegmon is inflammation of the deep layers of the skin that can spread to muscles and tendons.
Is Erysipelas Contagious?

In general, an existing erysipelas infection is not contagious to other people with intact skin and a well-functioning immune system. The causative bacteria can be found on the skin or mucous membranes of most people without causing any problems.
It only becomes dangerous when the bacteria can penetrate the body through a skin or mucous membrane defect and challenge the immune system with an infection. This can happen in particular when the physiological skin barrier (e.g. due to cracks in the skin, cuts in the skin, skin diseases, etc.) is destroyed and an entry portal is formed. If this is the case, however, the immune system in healthy people is usually still able to fight the spread of the pathogen and thus the infection. However, if the body has a weakened immune system for various reasons, the development of erysipelas can no longer be prevented.
Erysipelas can only be contagious if there is a transfer of bacteria from the patient's wound area to existing skin defects in another immunocompromised person.
Guideline in an erysipelago
According to the guideline of the German Dermatological Society (DDG) with regard to streptococcal infections of the skin and mucous membranes, erysipelas is an invasive pathogen infection that affects 100 out of 100,000 inhabitants and occurs primarily on the legs or face.
The diagnosis of erysipelas is usually made clinically, a port of entry (skin defects) and risk factors (venous weakness, diabetes mellitus, etc.) should always be looked for, and the pathogen should be determined by means of a smear from the affected area in order to begin the appropriate antibiotic therapy can.
The first choice for a pure streptococcal infection is the administration of penicillin G or V, but if there is a suspicion of an additional infection with another bacterium (usually Staphylococcus aureus), it must either be a 1st generation cephalosporin or a beta-lactam antibiotic with beta-lactamase inhibitors (amoxicillin + clavulanic acid) may be used. In the case of penicillin allergy, erythromycin or clindamycin should be used. If there is a severe initial infection, antibiotic therapy is usually started first with administering the antibiotic via the vein, but if symptoms improve, it can usually be switched to tablets after 2-3 days.
Overall, the guideline for the treatment of erysipelas provides for a total of 10-14 days of antibiotic administration, which can be supported with further symptomatic therapy (bed rest, elevated position, cooling, anticoagulation, etc.).
prophylaxis
It is important that people who are at risk of contracting erysipelas protect themselves well against it.
People with weakened immune systems are particularly at risk. These include old people, diabetics, but also patients who suffer from circulatory disorders. The skin should be carefully cared for. This protects it from injuries such as small cracks in the skin.













.jpg)