Post-zoster neuralgia
What is post-zoster neuralgia?
Post-zoster neuralgia is a condition in which there is very severe pain in a nerve after previously experienced shingles.
So it is ultimately caused by the herpes viruses, which linger in the body for years after a chickenpox disease and damage nerves.
When reactivating, the clinical picture of shingles occurs, with typical rashes. These heal in about 90% of the cases.
If this does not happen, post-zoster neuralgia occurs, which is ultimately based on permanent damage to the nerves by the viruses. If the pain is adequately treated, the symptoms occasionally disappear completely.

Causes of Post-Herpetic Neuralgia
Post-zoster neuralgia is a late possible secondary disease caused by the herpes viruses, also known as varicella-zoster viruses. These often cause the chickenpox disease in childhood, which heals on its own.
Afterwards, however, the viruses can linger in the body and migrate via nerve fibers into the cell bodies of nerves, for example in the face or chest area. The viruses linger in these cell bodies for decades and can, for example, be reactivated if the body becomes immune to weakness.
Then they can "break out" again, so to speak, and cause shingles. This results in painful blisters in the nerve supply area where they linger. Shingles heals up in around 90% of all those affected.
However, permanent damage to the nerves can also occur. These occur mainly in older people, whose immune system is usually somewhat weaker. This permanent nerve damage then manifests itself as post-zoster neuralgia. The risk factors therefore include:
- weakened immune system
- high age
- Virus therapy started too late
diagnosis
The diagnosis of post-zoster neuralgia always includes a physical examination and a detailed doctor-patient discussion in order to record the relevant history of the herpes virus.
An examination of the brain water can also provide information about the viruses that are still in the body.
Depending on the severity, an MRI of the back can also be useful. Inflammations can be searched for in the area of the spinal canal, which can provide information about the localization of the virus.
You can recognize post-herpetic neuralgia by these symptoms
Post-herpes zoster neuralgia is very painful in a specific area of the body. This area is initially still delimited and the localization depends on the nerves in which the herpes viruses have lingered after the chickenpox disease.
However, over time, the symptoms can spread to other areas and the pain may also appear in surrounding areas of the skin.
The focus of post-herpes zoster neuralgia is very severe pain, which often severely restricts the quality of life for those affected. Often those affected can no longer work fully and the quality of sleep is also reduced.
Pain
The pain in post-herpetic neuralgia is very severe because it is based on damage to the nerves.
They can express themselves in different forms. Either they are present as permanent pain, which is usually described as burning or piercing, or they come in repeated, very strong attacks. Alternatively, it can also appear as pain to touch, which is also known as allodynia.
The pain often represents a high level of suffering for those affected because it is very intense and therefore a great burden.
itching
The itching is not a typical symptom of post-herpetic neuralgia. On the other hand, it occurs more frequently with shingles, as a rash with fluid-filled blisters forms. These can occasionally cause itching, but are often more painful.
In post-zoster neuralgia, the focus is on pain. The clinical picture often only breaks out after the rash has subsided, which is why there is usually no itching. Occasionally the severe, burning pain can also be felt as a kind of itch. However, they are usually more of a stinging or piercing character.
Post-herpetic neuralgia without a rash
Post-herpes zoster neuralgia can occur at different times. The severe pain often does not set in until one month after the shingles has subsided, so after a month of freedom from pain, very severe pain occurs again. Then there is usually no more rash in post-zoster neuralgia, since the shingles has already healed.
Post-zoster neuralgia can also occur during shingles if it lasts for more than 4 weeks. In this case, a rash with the typical fluid-filled vesicles may exist at the same time as the disease.
Localization - where is the post-herpetic neuralgia particularly common?
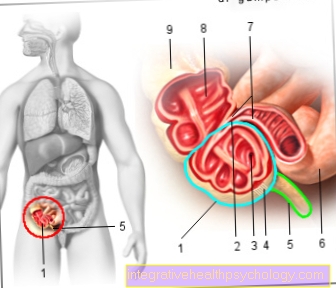
Post-zoster neuralgia usually initially has a specific localization, which depends on the nerves in which or in which cell bodies of the nerves the herpes viruses have lingered after the chickenpox infection. Depending on this, the pain then occurs in a certain area that is supplied by the nerves and in which the shingles disease was previously located.
Post-herpes zoster neuralgia can occur anywhere, but is often in the chest area or face, for example in the ears or eyes. In the latter, one also speaks of zoster oticus (in the ear area) or zoster ophthalmicus (in the eye area) during shingles.
In the course of post-zoster neuralgia, the pain often spreads to neighboring areas of the skin.
Therapy of post-zoster neuralgia
Since post-zoster neuralgia is associated with the greatest pain, which means a strong reduction in quality of life for those affected, the treatment focuses on the one hand on pain relief and on the other hand on maintaining everyday life, as well as the ability to work and improving sleep .
Depending on the intensity of the pain, the treatment is usually initially carried out with so-called anticonvulsants, which actually relieve cramps, but can also have an effective effect on certain points on the nerves. Typically, gabapentin or pregabalin can help. But also antidepressants, such as Amitryptyline can help against post-zoster neuralgia. Anesthetics, for example a plaster containing lidocaine, can also be used locally in the area of pain. If the pain is very severe, people may occasionally need to take opioid medication for a period of time. These include, for example, tramadol, oxycodone or morphine.
Please also read: Lidocaine patch
In addition to drug therapy, occupational therapy and nerve stimulation are available to down-regulate nerve activity. Psychotherapy should also be considered in the event of severe psychological stress.
A nerve block can also be used to treat post-zoster neuralgia. The stellate ganglion nerve plexus is blocked. The sometimes severe pain can be alleviated in this way. Read our article on this: Stellate ganglion blockage
Naturopathy
In naturopathy there are some remedies that can help with post-zoster neuralgia. How effective these work, however, depends on the individual affected. These include above all vitamins that strengthen the body as a whole and, depending on the type of vitamin, are also very important for the nerves and their function.
This includes vitamin B, especially vitamin B12, which can be taken as a support in post-zoster neuralgia. In addition, the so-called alpha-lipoic acid, which is important as a supplementary factor in many metabolic processes in the body, can be helpful.
acupuncture
Acupuncture can be used to support post-herpes zoster neuralgia. For some of those affected, this resulted in an improvement in pain. However, there are no studies on its effectiveness, so this should be tried individually. Small needles are inserted at specific points, so-called trigger points, and remain there for about half an hour. This can relieve tension caused by the pain.
Pain therapy
Pain therapy is highly recommended for severe or long-lasting post-zoster neuralgia. This offers the possibility of an individual setting and adaptation of the medication depending on the severity and localization of the pain. In addition, the potential dependence on strong pain medication is also taken into account. Since post-zoster neuralgia in many cases requires a recurring switch to another medication when the effect wears off, pain therapy can be very helpful for those affected.
Get more information about the Pain therapy
Duration of post-herpetic neuralgia
The duration of post-herpetic neuralgia can vary greatly and depends primarily on the age of the person affected and the immune system.
If the affected person is younger, they are often more likely to recover from the disease. The pain usually lasts about a month.
With increasing age it happens again and again that the post-zoster neuralgia lasts for more than a year. A lifelong existence of the disease is also possible, but rarely.
In addition, there is the effectiveness of pain therapy, on which the duration of the pain also depends.
Prognosis - can post-zoster neuralgia be cured?
In principle, post-zoster neuralgia can be cured or the pain caused by the disease can disappear. The prognosis for post-herpetic neuralgia, however, depends on many different factors.
First of all, it is essential that the shingles that existed before the post-zoster neuralgia is recognized quickly and treated accordingly with acyclovir, a drug against the herpes viruses. Starting therapy later has a negative effect on the prognosis, as the viruses have more time to further damage the nerves.
The immune system and the age of the affected person are also important for the prognosis. For many sufferers, the pain subsides after about a month. However, with age, the risk that post-herpetic neuralgia will last for more than a year increases.
In addition, therapy with pain medication does not work sufficiently for about 30% of all those affected, which leads to a severe reduction in quality of life.