Diagnosis of testicular cancer
introduction
Diagnostics at Testicular cancer includes several individual steps and examinations. First of all, the clinical diagnosis takes place, during which the primary tumor in the testicle is usually discovered, followed by the exploration of its possible spread and spread to other organs and tissues.

The operative diagnostics are then carried out. The affected testicle is removed and examined histologically (tissue). Only by adding up these two partial steps can an adequate Therapy of testicular cancer to be started.
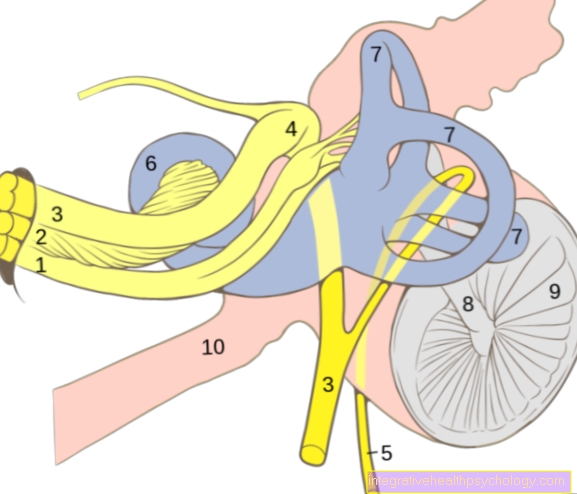
- Clinical diagnostics: Testicular cancer can 97% already through that Palpation (Scan) of the Testicles to be determined by the doctor. The specialist doctor responsible for this is the urologist. He carefully examines both testicles and first compares their size and texture. In the affected, mostly enlarged testicle, the tumor can usually be felt as a wood-hard lump. The urologist can do this Epididymis and also the Spermatic cord Separate it from the testicle and examine it for possible changes in size or tissue quality. In addition, the Lymph nodes in the strip and palpated around the inguinal canal for a possible Swelling of the lymph nodes in the groin region as a sign of spread of the testicular tumor.
The next step is a Ultrasound examination of both testicles displayed. With the so-called high-resolution scrotal sonography can over 98% of all tumors can be detected. If, for example, in rare cases a testicular tumor is not detected in the early stages during the palpation examination, preliminary stages can still be identified with the ultrasound examination. This method further determines the consistency of the palpable induration in the testicle. Here, between cystic (Cavities with water retention) and solid (solid) lesions. The early forms of germ cell tumors can be easily recognized by ultrasound, as so-called microcalcifications are found within the testicular tissue, which can be seen as "Snow"Or"starry sky“Represent. It is important that both testicles are included in the examination, since testicular cancer occurs on both sides in 1% of cases.
You can also find more information on this topic here: Ultrasound of the testicle
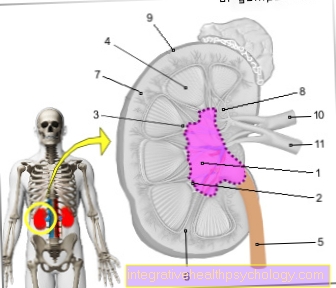
- Propagation diagnostics: In this diagnostic section, any metastases that may be present are recorded and the size and extent of the Primary tumor inside the testicle. This can be seen particularly well in a computed tomogram with contrast agent, which is why such an examination is mandatory in testicular cancer. The Computed Tomography is from thorax (Rib cage), Abdomen (upper and lower abdomen) and pelvis. With the help of this imaging, doctors can decide whether the affected lymph nodes also need to be removed during the operation. Furthermore, the liver and the lung, the organs that are primarily affected by spread in testicular cancer in addition to the lymph nodes. If metastases are found there, this is an important criterion for the staging (division into stages of aggressiveness) of the testicular cancer and the selection of therapeutic measures.
- Tumor marker: Determination more specific Hormones and proteins in the blood is another step in diagnosis Testicular cancer. Depending on the origin of the tissue, the cells of the tumor release various of these substances. As a general rule for Tumor markers holds that an increase in their concentration in the blood means that the tumor is active. If these values continue to rise in the course of the disease, it must be assumed that the testicular cancer has progressed. Thus, tumor markers in testicular cancer are important for process control and for assessing the success of the therapy. At the beginning of one chemotherapy or radiation therapy, the tumor markers can also increase, but this is more of a positive sign, as it indicates the death of tumor cells, which means that these substances are increasingly released into the blood. The most important markers in testicular cancer are these apha fetoprotein (AFP) and the human chorionic gonadotropin (HCG) for non-seminomas, as well as the placental alkaline phosphatase (PLAP) for the seminome. However, a tumor marker determination alone is never sufficient for a determination of a tissue type, since this examination is not specific enough. It is only indicative in combination with the rest of the diagnostics.
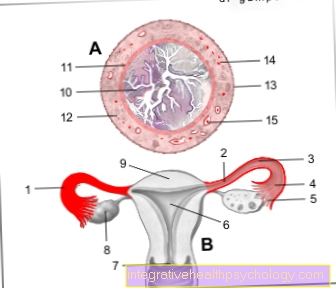
- Operative diagnostics: The operation of the Testicular cancer is both one therapeutic, as well as a diagnostic Measure. This is always the affected Testicles removed and a sample taken from the other testicle with a small incision as the likelihood of the cancer occurs in both testicles simultaneously (approx. 1%). Most often the testicle affected by the tumor is removed through a small incision in the groin.
The scrotum remains unharmed. In the case of an uncertain diagnosis, for example a lump visible in the ultrasound, the one in his malignancy (malignancy) cannot be reliably assessed, the testicle is first exposed and examined more closely. Furthermore, a histological examination of a sample of the node in question is carried out by the pathologist during the operation. A decision is then made as to whether the testicle can be preserved or whether removal is necessary. It depends on Lymph nodes are affected in the groin or in the area of the collarbone or in the abdomen, these are also removed as part of the operation. The removed testicle and, if applicable, the removed testicles Lymph nodes and tissue samples are placed in the pathology sent to be examined and assessed under the microscope. The pathologist's findings are made a few days later. Only then is it clear what type of testicular cancer it is, how malignant and advanced it is, and how it can be treated accordingly.
The absence of a testicle can be for men psychologically can be very problematic, even if this does not affect the potency or medically fertility means. There is therefore the possibility of at least cosmetically compensating for the loss by inserting an artificial testicle made of plastic into the scrotum after the surgical wound has healed. For example, medical laypeople can neither optically nor feel that a testicle has been removed.