Pus in the jaw
Definition - what is pus in the jaw?
Pus in the jaw can have numerous causes and forms, but it is much feared by the population as a complication of toothache as swelling in the jaw area. In technical jargon, medical professionals speak of an abscess. An abscess describes a collection of pus in a newly formed cavity. This cavity can appear anywhere on the body.
However, the soft tissues above the coccyx or the oral cavity are preferred.
In the oral cavity, the newly formed cavity produces a swelling with an uncomfortable pressure that can cause problems with opening the mouth and difficulty swallowing. But where does the abscess come from and why is it so dangerous?

What is osteomyelitis?
Osteomyelitis is inflammation of the bone marrow caused by a bacterial infection.
Osteomyelitis can occur acutely, for example directly after surgery. For example, it may happen that the bone does not heal after a wisdom tooth removal or another surgical procedure in the oral cavity, but instead signs of inflammation appear.
Chronic forms of osteomyelitis can also occur. Symptoms of this condition include pain, swelling, and loosening of the teeth in the affected area. The granulation tissue and inflammatory cells create an unpleasant odor in the mouth.
If the osteomyelitis is left untreated, bone parts can die and the infection can pass into the systemic circulation. The lymph nodes swell, a fever forms, and the inflammatory cells try to get to the heart, which is a sepsis, so can cause blood poisoning.
Therapeutically, a dose of antibiotics can be sufficient to heal the inflammation. Are however Bone necrosis, i.e. lost bone tissue is present, the dead bone parts have to be removed so that regeneration takes place. Also drugs that affect bone metabolism, such as the Bisphosphonates, are then used.
Read more about this at: Temporomandibular joint osteomyelitis
Causes of pus in the jaw
The classic disease with accumulations of pus is an abscess in the jaw. It occurs in bacterial inflammation that has a tendency to spread.
The abscess is always a possible complication of apical periodontitis, an inflammation below the tip of the root.
Read more on this topic at: Root inflammation
Dead nerves within teeth can also cause abscesses in the jaw. Even after the root canal treatment, any remaining bacteria below the root tip are potentially able to develop abscesses.
The most common cause, however, occurs with wisdom teeth, which, when shifted, grow out crooked and can form niches for bacteria. Furthermore, a loophole for bacteria can arise after the wisdom teeth have been removed, so that an abscess can develop.
Read more on this topic at: Abscess in the upper jaw
Abscess after a wisdom tooth removal
A wisdom tooth removal is a complex surgical procedure, which can restrict mouth opening and food intake in the follow-up treatment.
Oral hygiene and food intake are particularly difficult when removing all four wisdom teeth in one session.
This allows bacteria to lodge in the now empty tooth sockets and lead to inflammation. The bacteria can cause an inflammatory reaction to develop in the remaining cavity, which creates pus. This abscess has a tendency to spread and enter the systemic circulation.
An abscess formation in the area of the wisdom teeth is with
- Pain
- Swelling
- and difficulty swallowing.
This is not entirely without risk, as it can lead to blood poisoning. It is therefore important to visit a dentist as soon as possible in the event of swelling after a wisdom tooth removal or to go to a dental-surgical emergency service outside of the consultation hours.
Read more on this topic at: Inflammation after a wisdom tooth operation
Pus in the jaw after a root canal treatment
After the end of the root canal treatment with a root filling, a possible complication is that bacteria have remained below the root tip and these have an acute tendency to spread.
The bacteria can form a cavity in which pus is formed by the body's immune system, creating an abscess. This mainly happens because the pus cannot escape upwards and therefore produces a swelling. The swelling creates a lot of pressure, massive bite disturbances and unbearable pain.
If no treatment is given, swallowing difficulties arise, and depending on the situation, airway obstruction and sepsis (blood poisoning) can also occur.
Read more on this topic at: Inflammation after apicectomy
diagnosis
Diagnosing an abscess is a collection of pus in the oral cavity. The practitioner feels the swelling and tries to feel the edge of the lower jawbone underneath. A plump and hard swelling is critical, while a soft swelling may not require any treatment.
If the lower jaw is not palpable and is associated with swallowing or breathing difficulties, there is an urgent need for treatment.
Fever is also an acute sign of inflammation, which is checked.
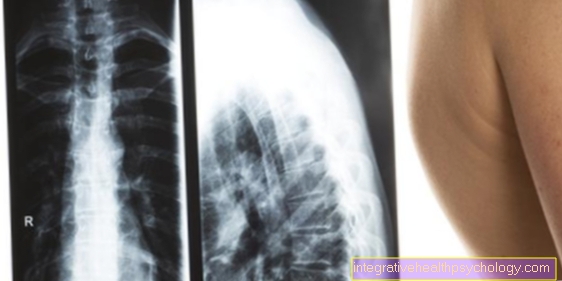
In addition to clinical examinations, X-ray diagnostics are used as a supporting medium to make a clarifying diagnosis.
Concomitant symptoms
Concomitant symptoms are the typical signs of inflammation:
- Redness
- swelling
- overheat
- Pain
In the case of the abscess, the swelling in particular is the most striking accompanying symptom. The swelling is visible from the outside and displaces the soft tissue. It feels soft, roughly comparable to a balloon filled with water.
Furthermore, the abscess is usually red and feels overheated. The accumulation of pus creates increased pressure.
Pain in the area of the abscess, which can also spread to other head regions, is also likely.
Immediate treatment is required if symptoms such as difficulty swallowing and airway obstruction.
Can you have pus in the jaw without any other symptoms?
As a rule, the abscess creates the displacement of existing tissue by filling a cavity, which is associated with tension.
The tissue is only able to expand to a certain extent. The larger the accumulation of pus, the greater the pressure pain and severe swelling, which is also visible from the outside. As a result, the symptoms are usually associated with massive pain.
Abscess formation without symptoms is usually not possible. Even soft swellings usually cause pain when touching. The pain can be so severe that a dentist is usually consulted as soon as possible.
Treatment of pus in the jaw
Therapeutically, attempts are made to drain the pus depending on the extent of the swelling.
In the event of an inflammation at the root tip, this can already be done by drilling open the tooth, in which the nerve tissue is then removed and a rinsing disinfection is carried out. The tooth is closed with a foam pellet to ensure that the pus can continue to escape. Only when the tooth is completely free of symptoms is the root canal treated and closed with a root filling.
However, if the abscess is severe, reaming will not be enough to drain. In this case, a relief incision, known as a Incision, carried out. The previously anesthetized gum above the abscess is cut open with a scalpel so that the pus can escape. As a rule, a flap or gauze (gauze compress) is inserted into the cavity and rinsed so that the pus can drain completely. Only when the patient is symptom-free is the strip removed from the wound and the wound heals on its own.
In the case of an abscess after a wisdom tooth removal, a Incision carried out. The abscess pus must be drained through a relief incision to relieve the pressure and, if necessary, to re-open the airways.
The massive expression requires supportive therapy with antibiotics. In doing so, aminopenicillins such as amoxicillin are used. The amoxicillin is taken three times a day for five days.
If necessary, ibuprofen can also be taken as pain medication. The maximum dose for adults is 2400 mg per day and should not be exceeded.
If these painkillers are insufficient, ibuprofen can be combined with Novalgin® if necessary.
Ask your doctor for advice if you have pain in your jaw.
In the case of an advanced abscess that develops into sepsis, admission to hospital or clinic is immediate.
Read more on this topic at: Symptoms of blood poisoning
Homeopathy for pus in the jaw
In the case of pus-filled abscesses, supportive homeopathic therapies in addition to surgical therapy are quite useful.
Globular preparations that can be taken for this indication are, for example, Hepar sulfuris or Mercurius solubilis. However, the appropriate dosage should be clarified with the treating dentist.
Which home remedies can help?
If there is a build-up of pus in the jaw with severe swelling, the person affected should always keep their head up in order to keep the airways free and to avoid increased blood flow towards the head. This would create heat that could encourage inflammation to develop and spread.
Furthermore, the patient should regularly cool the affected area about once to a maximum of twice an hour. The cooling process takes about five to a maximum of ten minutes. The cooling is supposed to fight the bacteria, prevent the swelling from enlarging and relieve the pain symptoms for a short time.
It is also advisable to drink plenty of fluids and avoid strenuous activities.
After the incision has already been made, the patient can massage and knead the affected area so that the pus is completely drained. Rinsing with chamomile tea or herbal tinctures diluted with water can soothe gums and prevent unpleasant smells and tastes.
The patient should avoid grains such as sesame and poppy seeds in food, as they could settle in the wound and cause re-inflammation.
Duration of an abscess in the jaw
The abscess can develop very quickly. After the initial signs of inflammation, the "thick cheek" can appear overnight.
Slower processes with the formation of the abscess within a week are also conceivable. Healing can take anywhere from one to two weeks until the inflammatory cells recede and the wound is completely closed.