Electromyography
definition
Electromyography (EMG, electromyography) is a clinical examination method that can be used to objectively record the electrical activity of one or more muscle fibers at the same time. This may be necessary in order to identify damage in the muscular area and to limit it more precisely.
Measurement method
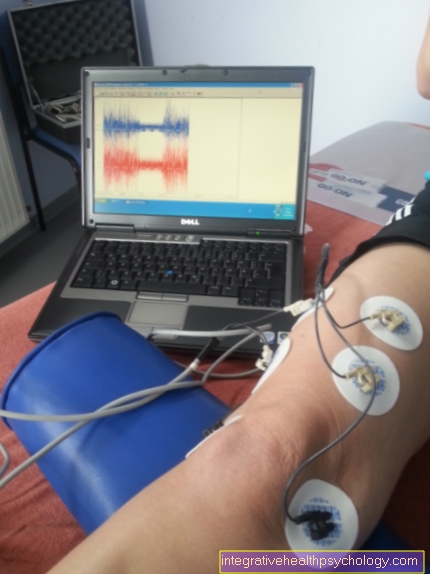
In electromyography, the electrical activity of the muscle fibers can be derived either through a superficial electrode attached to the skin, or through a needle electrode directly on the muscle. Two different types of needle electrodes are used.
The monopolar electrode in electromyography serves as a measuring electrode, while an electrode glued to the skin serves as a reference electrode.
With the concentric electrode there is a fine wire as a measuring electrode in the needle, the needle cover serves directly as a reference electrode. With both methods of electromyography (EMG), the voltage difference between the measuring and reference electrodes is used for the clinical evaluation.
Anatomical basics
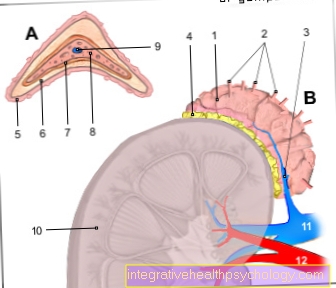
A muscle is made up of a large number of individual motor units, which, depending on the type of muscle, consist of a few or very many muscle fibers can exist. Each of these motor units is about an individual nerve controlled (front horn cell with Axon). The more motor units a muscle has, the finer movements are possible, as many different motor units can be individually controlled by different nerves.
Cumulative action potential of a motor unit
When a nerve (Anterior horn cell) from brain is controlled, discharged (depolarize) all muscles belonging to this motor unit contract and contract, i.e. the muscle moves (contraction). The electrical activity that results from this movement is known as Action potential a motor unit (MUAP), as the electrical potentials of many individual muscle fibers are superimposed and recorded together. You can find out more about the exact transmission of excitation in the muscles under "Motorized end plate"read.
Electromyography Risks
The Electromyography (EMG) is an invasive diagnostic method that is very widespread and in the rarest of cases leads to complications such as Bleeding, Infections and Injuries to the nerve himself leads.
Procedure EMG
The goal of Electromyography (EMG) it must be found out whether the clinical symptoms consist of:
- one Damage to the nerve,
- from a Damage to the muscle or
- out none the mentioned arises.
For this purpose, the Electromyography (EMG) various characteristics of the action potential of motor units (MUAP) are used in order to enable a dedicated evaluation of the electromyography. The parameters to be evaluated include the wavelength (amplitude) of the MUAP, time to the first peak, duration of the MUAP and the number of phases. In addition, it can be discussed whether the number of MUAPs triggered per stimulation of the muscle is sufficient, increased or decreased. The electromyographic examination of each muscle consists of four different test procedures, all of which are carried out at different locations on the muscle.
When the electrode is inserted, the muscle is briefly stimulated and an electrical potential that can be diverted is created. If this electrical activity continues well after the needle has been inserted into the muscle, this indicates that the muscle has previously been damaged.
This can be the result of Inflammation (Inflammation), abnormal changes in the muscle (Myotonia) as well as lack of connection to the nerve (Denervation) of the muscle. If there is no electrical activity whatsoever when inserting the needle, this either speaks for a clear one muscular dystrophy (atrophy) or a connective tissue remodeling of the muscle (fibrotic muscle).
As a second test procedure the Electromyography (EMG) one assesses the spontaneous activity of the muscle after inserting the needle.
A normal muscle does not emit any electrical impulses at rest, except for smaller potentials near the motor endplate, at the point of transmission between nerve and muscle.
These potentials are with 0.5 - 2 ms very short and completely normal (physiological). In this case, one should try to reinsert the needle at a different point where no motor end plates are stimulated in order to remove this interference factor from the electrical discharge.
If an electrical potential is found in the muscle to be examined, it is called Fibrillation. These usually occur when the muscle is no longer in contact with its actual nerve and then permanently generates an electrical potential itself.
Fibrillation potentials usually last 1 to 4 milliseconds and can have a wavelength of several 100 microvolts to have. In addition, fibrillation potentials are strictly rhythmic and often occur two or three times in direct succession. After nerve damage it can take 10-14 days for fibrillation in the Electromyography (EMG) are visible.
In addition to disturbances of the innervation, inflammatory changes can also lead to increased electrical activity at rest, especially when these occur acutely and with Cell death (necrosis) are connected. In addition to the fibrillation, fasciculations can also occur at rest. This fasciculation is caused by damage to the nerve that innervates the motor unit. The nerve is electrically discharged (depolarized) which leads to the formation of action potentials in the motor unit. This usually happens several times a minute and is a sign of one Nerve damage (Neuropathy).
In addition to nerve damage, the recording can also be used to identify damage to the muscle itself. The so-called myotonic discharges are action potentials that approx. 100 times per second triggered and take a few seconds. They indicate damage to the ion channels in the muscle membrane.
In the third Investigation method the electrical activity of the muscle is derived with minimal voluntary movement of the muscle. This method examines whether the muscles have a pause interval of between contraction 50 to 250 ms insert. If this time is significantly reduced (2 - 20ms), this indicates increased excitability (hyperexcitatory) of the muscle. This status can be for example through Hyperventilation, tetanus or neuronal diseases like Amyotrophic Lateral Sclerosis (AS) be conditional.
In this phase one finds the Electromyography (EMG) no electrical potential, one assumes a complete separation of the nerve fibers from the muscle (total denervation) out.
Renewing the supply of nerve fibers to the muscle can take a long time, since nerve fibers only move at a speed of 1mm / day grow and this can take a correspondingly long time after the muscle to the injury site has been removed.
However, one can be found much more frequently in everyday clinical practice chronic partial denervation of muscle fibers. In this case, some motor units of the muscle are no longer supplied by the nerves assigned to them, for example as a result of an illness or an accident. The body tries to repair this by branching out the remaining nerve fibers again to innervate muscle fibers that are no longer supplied by nerves.
Individual nerve fibers can control up to five times more muscle fibers than before. If, on the other hand, there is a loss of motor units, one often sees one enlargement (hypertrophy) of the remaining motor units.
The fourth discipline of electromyography is used to record the MUAPs with increased voluntary muscle contraction up to maximum contraction. This is also called the Interference pattern analysis designated.
This way of looking at things gives an initial indication of whether the clinical picture is due to damage to the nerve or the muscle. If the muscle is damaged as the cause of the symptoms, this MUAP a lower amplitude, if the nerve is the cause of the complaints, the MUAP has a greater amplitude and the MUAP itself lasts longer. However, neither of the two findings is solely characteristic of one of the two types of damage.
Summary
By the principles of Electromyography electrical potentials of motor units can be recorded and evaluated. Especially together with the analysis of the nerve conduction velocity (NLG) the EMG offer a possibility of clinical symptoms such as Muscle weakness to work on it in a dedicated manner, as well as to make first assessments for the prognosis as well as the first diagnosis of various nerve disorders and inflammatory processes in the muscle.
However, there is no particular potential in the Electromyography (EMG) characteristic of a single disease; therefore the result of the Electromyography (EMG) must always be interpreted in the context of the patient as well as his other diseases and examinations in order to present a profitable diagnostic method for the patient.