Phases of wound healing
introduction
Wound healing phases are the various stages in which the complete healing of a wound takes place. A healthy body is able to regenerate injuries through complete regeneration of tissue or the formation of replacement tissue (scar tissue). A distinction is made between four to five phases of wound healing. Healing begins with the body's own bleeding control (hemostasis), followed by the three main phases of wound healing, the cleansing phase, the granulation phase and the regeneration phase. Hemostasis is sometimes added to the cleaning phase.

Procedure and duration of the phases
Wound healing begins immediately after the injury Hemostasis (Hemostasis) characterized. Immediately after the damage to the affected tissue, the blood vessels contract reflexively (reflex vasoconstriction). This stops the blood flow and enables the Clasp the wound through a fibrin network. fibrin is a protein that is produced by the body and, when tissue is damaged, is released by various enzymes from its precursor fibrinogen, which circulates in the blood. Many fibrin proteins accumulate to form a “plug” at the site of the tissue damage and thus close the wound.
This first wound healing phase is already after few minutes (5-10) completed.
Now cells of the immune system migrate to the wound and loosen it Cleaning phase (also exudative phase). White blood cells (Leukocytes) and Phagocytes (Macrophages) remove the fibrin plug and any intruding Germs. Classic signs of inflammation like warmth, Redness and pain therefore occur especially during this approx. 3-day Phase up. During the following Granulation phase New tissue and blood vessels form at the site of the wound. First, connective tissue cells migrate (Fibroblasts) and attach to the remains of the fibrin network. That is where they begin to form Collagen, the protein that is the main component of our skin and connective tissue. However, the collagen formation is not completed, rather a species is created Filling fabric, the so-called Granulation tissue. Like the cleaning phase, the granulation phase lasts up to 3 days. The last phase closes after about a week Regeneration phase on. Collagen is now fully formed, as are new skin cells. Depending on the size and depth of the wound, this phase can occur Days to months last for.
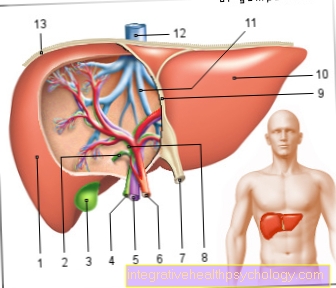
Granulation tissue
Granulation tissue refers to the "filling tissue" of a wound that develops in the granulation phase. It closes the wound and forms the basis for the creation of new skin cells and blood vessels. Outwardly, this type of tissue often appears reddish With grainier (more granulated) Surface. This includes connective tissue cells (Fibroblasts), which are responsible for the formation of new connective tissue and skin as well as the smallest new blood vessels (Capillaries). If little or no granulation tissue forms, the wound healing phases cannot be completed completely because the lack of blood vessels means that they are insufficient Oxygen supply is possible. In this case, the edges of the wound greasy and turn a strong red to bluish color. This can be remedied by scraping the edges of the wound with a sharp spoon (curettage), whereby the outdated wound tissue is removed, creating space for healthy new growth.
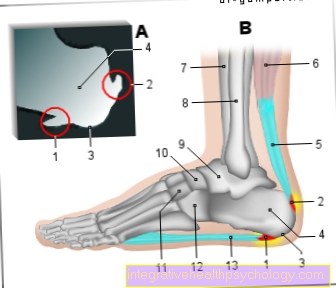
Phases of wound healing in bones
The healing process of a broken bone (fracture) is divided into two types. In primary bone healing, the fragments are usually still in contact with each other; the fracture heals after a few weeks due to new bone formation. If the fracture ends are no longer in contact, secondary bone healing takes place. Similar to wound healing, secondary bone healing can also be divided into five different wound healing phases. After the first phase, the injury phase, in which the fracture and a bruise occurred in the bone, the inflammation phase follows (phase 2). Phagocytes (Macrophages), White blood cells (Leukocytes), bone-forming cells (Osteoblasts) and cartilage builders (Chondroblasts) begin with the breakdown of the fibrin network and the build-up of bone-forming protein (Collagen). This build-up of new bone and cartilage substance continues in the granulation phase (phase 3). A “callus” (thickening of “young” bone substance) is created, which thickens more and more in the fourth phase, the “callus hardening”. Ultimately, the original lamellar bone with its typical structural features, the seminiferous tubules (longitudinal and transverse channels in the bone that carry blood vessels), emerges from the callus through the ingrowth of blood vessels. After a total of 6 months to 2 years, a bone is completely healed.
Phases of wound healing in the mouth
In addition to the typical wound healing phases, i.e. cleaning phase, granulation phase and regeneration phase, wounds in the mouth also have a special feature. The oral cavity of healthy people is covered with a film of saliva. In addition to water, mucus and digestive enzymes, saliva also contains protein Histatin. This protein contains a lot histamine (an amino acid) and inhibits invading germs such as bacteria or Mushrooms in the spread. The wound healing in the mouth goes because of this uncomplicated of equip, infections are less common than on other parts of the body.
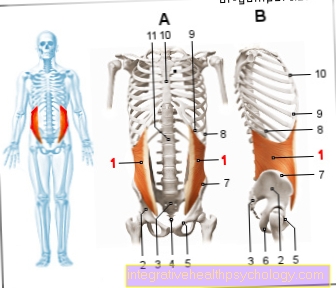
Pressure ulcer

The wound healing of a pressure ulcer (extensive skin damage caused by pressure and shear forces), like the healing of other wounds, follows the 3 main phases of wound healing. Since a pressure ulcer almost always occurs in parts of the body that are exposed to constant pressure, for example on the tailbone or shoulder blades in bedridden patients, this type of chronic wound is extremely long and difficult to treat. If possible, the body's own healing should be supported to close the wound.
In the first phase, the Cleaning phase it is important to help the body keep the wound off Germinate keep free. Bandages that contain blood and Wound secretion take up quickly are an advantage, but must up to six times a day change. This is the only way to reliably remove bacteria and other germs from the wound. To the following Granulation phase Propel pressure ulcers can surgically be "cleared out". Be there dead (Necrotic) areas of skin removed until a clean wound bed is formed. This makes it easier for the body to form granulation tissue from which new skin can develop. Finally during the Regeneration phase it is important to protect the affected body part as much as possible low pressure to store so as not to disrupt wound healing and to avoid a new pressure ulcer. Aids that are often used here are "pressure ulcer mattresses" and many others Rearrange of the bedridden patient. If the body is optimally supported during the wound healing phases, pressure ulcers that have existed for a long time can also be made to heal.
















.jpg)


.jpg)