Function of the heart
Synonyms
Heart sounds, heart signs, heart rate,
Medical: Cor
English: heart
introduction
Through constant contraction and relaxation, the heart ensures the blood flow to the whole body, so that all oragne are supplied with oxygen and nutrients and degradation products are transported away. The heart's pumping action takes place in several phases.
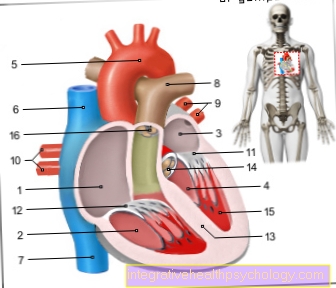
Illustration heart

- Right atrial -
Atrium dextrum - Right ventricle -
Ventriculus dexter - Left atrium -
Atrium sinistrum - Left ventricle -
Ventriculus sinister - Aortic arch - Arcus aortae
- Superior vena cava -
Superior vena cava - Lower vena cava -
Inferior vena cava - Pulmonary artery trunk -
Pulmonary trunk - Left pulmonary veins -
Venae pulmonales sinastrae - Right pulmonary veins -
Venae pulmonales dextrae - Mitral valve - Valva mitralis
- Tricuspid valve -
Tricuspid valva - Chamber partition -
Interventricular septum - Aortic valve - Valva aortae
- Papillary muscle -
Papillary muscle
You can find an overview of all Dr-Gumpert images at: medical illustrations
Heart action
So that heart If the blood can pump so effectively that it flows through the whole body, it must be ensured that all heart muscle cells work together in a coordinated manner within the framework of the cardiac cycle. Basically, this control works through an electrical impulse that arises in the heart itself, then spreads in the muscles and leads to an orderly action (contraction) in the muscle cells. This is only possible because all cells are electrically conductive and connected to one another.
The work cycle / heart function (filling the heart with blood and expelling the blood into the circulation) is divided into 4 phasesthat run regularly one after the other: Relaxation and filling phase (together: Diastole) as Tension and expulsion phase (together: Systole).
In physical rest it is Duration of diastole 2/3 of a cardiac cycle (approx. 0.6 sec), the systole 1/3 (approx. 0.3 sec). If the Heart rate increases (and thus the length of a cardiac cycle decreases), this is done by increasing the shortening of the diastole. The terms of the individual phases relate to the condition of the heart chambers, as they deal with the much more important part of the heart's work. They run right and left simultaneously.
The individual phases in detail:
- Tension phase: When the heart is filled with blood, the muscle cells of the heart chambers begin to tense and increase the pressure inside the heart cavity (isovolumetric work), but without contracting because all the heart valves are closed. The pressure in the chamber is higher than in the atrium, so the leaflet valves are closed. Also in the executing vessels (right: Pulmonary artery = Pulmonary trunk, left artery = aorta) the blood pressure is higher than the pressure in the Chamber of the heart, therefore the pocket flaps are also closed.
- Expulsion phase: The ventricular musculature increases the pressure in the chamber steadily (tensing) until it reaches the Blood pressure of the executing vessels. At this moment the pocket flaps open and the blood flows from the chambers into the executing vessels. The pressure now prevailing is called the Systolic blood pressure (the higher value when measuring blood pressure, approx. 120mmHg). As blood is ejected from the chamber, the volume and therefore the pressure decreases. This process continues until the pressure in the chamber falls below the pressure in the executing vessels (Diastolic blood pressure - the smaller of the two measured values, approx. 80mmHg). When this point is reached, the pocket flaps are passively closed again (by the apparently reversing blood flow) and the systole is over. A total of 60-70 ml was expelled from the heart, which corresponds to an ejection rate (ejection fraction) of 50-60% of the total blood in the heart chamber.
- Relaxation phase: During this phase the myocardial cells relax, whereby all heart valves are closed because of the pressure differences to the inflow path (atria) and expulsion path.
- Filling phase: Because of the closed leaflet valve, the blood from the atrium could no longer flow into the chamber, so that more blood has now collected here. From the point in time at which the pressure in the atrium exceeds the pressure of the (relatively empty) chamber, the filling phase begins and the blood can flow into the chamber again. The filling is favored by the relaxation of the ventricular muscles. The chamber relaxes and returns to the starting position. Since the blood in the heart no longer changes its position, the leaflet valves now literally turn over the blood that had previously collected on the closed leaflet valves. This mechanism is called the valve level mechanism and explains why after the first third of the filling phase, of the chamber filling is already reached - and therefore why you can accept a shortening of the filling phase without a great loss of effectiveness. At the end of the filling phase there is a supporting contraction of the atrial muscles in order to force the remaining amount of blood into the chamber.
Arousal and conduction system
The work of the heart / function of the heart is triggered and controlled by electrical impulses. This includes that the impulses arise somewhere and are passed on. These two functions are taken over by the arousal and conduction system.
The Sinus node (Nodus sinuatrialis) is the origin of the electrical impulses. It is able to spontaneously and regularly generate electrical excitations and thus acts as a clock generator for the Heart muscles.
If the function of the sinus node is disturbed Arrhythmia. The signals from the sinus node are generated in the form of electrical excitation via the cell-cell connections of the muscle cells (no nerves!). Some muscle cells have a special equipment, which is why they can conduct particularly quickly or slowly. The excitement of the heart signs mainly spreads through these paths; they are therefore referred to as Conduction system. The excitation goes from the sinus over the atrium to the AV node, then via further defined sections into the heart chambers, where the bundles finally branch into the Purkinje fibers. From these, the excitation spreads across the ventricular muscles.
The sinus node as the origin of the cardiac excitation lies in the muscle wall of the right atrium and consists of specialized muscle cells that can generate electrical excitations without any external influence. These excitations spread in the atria and then reach the AV node, a cluster of cells near the Atrium-ventricle boundary. It consists of the cells of the atrium with the slowest conduction speed. The cells of the AV node are also special heart muscle cells in this respect; because, like the sinus node, they can autonomously generate excitations (electrical impulses measured as heart signs) - but only with half of them frequency. The function of the AV node is explained by the fact that the AV limb emerges from here as the only electrically conductive connection between the atrium and the ventricle - the AV node is a kind of filter station to protect the vital and sensitive ventricular muscles. Its slow conduction of excitation serves to ensure that the excitation is only passed into the chamber after the atrial contraction and thus the atrial contraction still falls into the diastole of the ventricular muscles. The ability to generate excitation on its own is required if, for whatever reason, the electrical impulses from the sinus node are missing. Then the AV node takes over the task of the sinus node at least partially.
Sinus node
The Sinus node, rarely too Keith Flack Knot called, consists of specialized Heart muscle cells and is through the Transmission of electrical potentials responsible for the contraction of the heart and thus the clock of the heartbeat.
The sinus node lies in the right atrium just below the mouth of the right vena cava (Vena Cava). The size is usually included under an inch. The specialized cells are no nerve cellsalthough they create an electrical potential that, when conducted in the atrium, causes them to contract. From a histological point of view, they are specialized heart muscle cellsthat have the ability to depolarize and thus become one in healthy patients Heart rate of 60-80 beats to lead. The sinus node is supplied with blood through the right one Coronary artery.
The sinus node takes over this in the heart Function of the clock. If you take the healthy heart out of a person, it beats if it continues with blood is supplied, still continue. This is because the normal heart rate is not changing brain, but is controlled from the sinus node. However, through other nerves (Sympathetic and Parasympathetic nervous system) that lead to the heart Influences the speed at which the heart beats. So it can beat faster (Sympathetic), such as when one is excited or else beat slower (Parasympathetic nervous system).
The sinus node has different ion channelsthat cause the cells to depolarize. This means that an electrical signal is given and passed on. This signal now flows through the atrium and hits another node. The so-called Atrioventricular node, short AV node. The name of the AV node comes from the location, as it is between Forecourt (Atrium) and chamber (Ventricle) lies. It serves as a filter for the incoming sinusoidal signals.
A short one Failure of the sinus node is not noticed at first, because the AV node also spontaneous action potentials forms and can thus also contribute to the transmission of stimuli. However, these actions are not sufficient because the AV node is not in the same frequency as the sinus node depolarizedbut only to one Heart rate to about 40 beats the minute is capable. If this knot also fails, cardiac arrest occurs. However, this is rarely the case.
If the sinus node fails completely, this is called sinus arrest. Diseases that affect the sinus node are included Sick sinus syndrome summarized.
Control of the heart's action
This whole process works automatically - however, without connection to the nervous system of the body, the heart has little opportunity to adapt to the changing requirements (= changing oxygen demand) of the entire organism. This adaptation is mediated via the heart nerves from the central nervous system (CNS).
The heart is supplied by nerves of the sympathetic (via the trunk) and the parasympathetic (via the vagus nerve). They give the signals whether the heart's performance should be increased or decreased. The sympathetic nerve and the vagus nerve are nerves of the autonomic nervous system, whose activity cannot be controlled voluntarily and whose function is to regulate various organ functions if necessary (breathing, heart action, digestion, excretion, etc.).
If the cardiac output is to be increased - the ejection output can be increased from 5 l / min to up to 25 l / min - there are various ways in which this can be achieved:
- The heart rate / heart function (in the sinus node) is increased (positive chronotropic). More heartbeats mean more ejection performance in the same amount of time. The pulse rises.
- The impact force (and thus the proportion of blood that is ejected) is increased.
- The excitability of the muscle cells is increased. If the muscle cells react faster to the electrical stimuli, the cardiac cycle can run more easily and effectively (positive bathmotropic).
- The delay in the conduction of excitation in the AV node is reduced (positive dromotropic).
Overall, after activation by the sympathetic nervous system, more blood is released per unit of time and thus more oxygen is pumped through the body. However, the heart also needs more oxygen for its increased work, which is why strict rest is prescribed for a weakened or damaged heart (heart failure = cardiac insufficiency) or if the blood vessels in the heart are known to be deficient (coronary heart disease = CHD).
The information from the nerves is transferred to the muscle cells via special proteins in the cell wall (so-called beta receptors). This is the point of attack of the beta-blockers, which are widely used therapeutically: They limit the increase in cardiac output; in this way they lower the heart's oxygen consumption (use in angina pectoris / myocardial infarction) and thereby indirectly the blood pressure (use in high blood pressure).
If the body wants to throttle the work of the heart, it has fewer mechanisms at its disposal, since the braking nerve fibers from the parasympathetic vagus nerve only reach the atrium up to the border of the auricle. The possibilities are therefore limited to the atrium:
- Lowering the heart rate / heart sign (negative chronotropic) and
- Increase in AV conduction time (negative dromotropic).
In extreme cases, you can see the effects of the vagus nerve on the so-called athlete's heart. A cyclist's ability to perform, for example, is so great that he only needs a fraction of it at rest. You can find resting pulse rates of 40 and less; this is controlled by the parasympathetic nervous system.
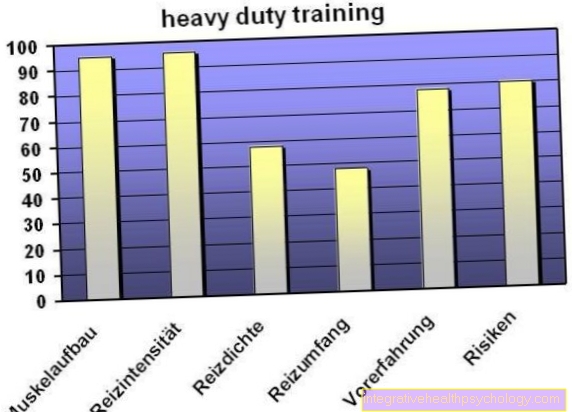
Heart rate calculation
If you want to train in your individually optimal heart rate range, you should use your optimal one Heart rate can calculate.
The calculation is based on the so-called Karvonen formula, the resting frequency is subtracted from the maximum heart rate, the result is multiplied by 0.6 (with high intensity training by 0.75) and then added to the resting heart rate. The maximum heart rate is calculated by subtracting the age of the athlete from 220. You can measure your resting frequency yourself. To do this, lie down quietly for ten minutes and then measure your heart rate.
At Untrained the value will be between 60 and 80 beats per minute lie, whereas Competitive athlete a resting heart rate of up to 35 strokes can have. The calculated values for an exposure with medium intensity (multiplied by 0.6) and high intensity (multiplied by 0.75) are only guidelines.
Endurance training using the endurance method should take place, for example, in the medium intensity range.