Endoscopy
definition
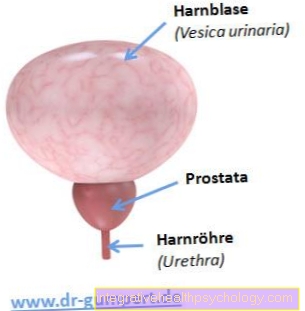
With the uterine specimen, medically Hysteroscopy, on the one hand, it is a diagnostic procedure in which the cervix, the uterus and the fallopian tubes are examined and assessed. For this purpose, an optical instrument is pushed through the vagina, over the cervix, into the cervix and further into the uterine cavity, and supplies image material to a monitor, which the examiner evaluates.
On the other hand, the endoscopy is also a therapeutic procedure, whereby surgical interventions on the uterus can be carried out if necessary. For this purpose, in addition to the optics, further instruments are inserted into the uterus after widening the cervix.

When is a hysteroscopy performed?
For the endoscopy (Hysteroscopy) there can be diagnostic as well as therapeutic indications. Diagnostic goals are pursued if, for example, abnormal ultrasound findings are present and these should be clarified more precisely hysteroscopically.
Other reasons for this investigation could be:
- an unfulfilled desire to have children
- Bleeding disorders or irregularities
- Polyps
- Fibroids of the uterine cavity
Read more on the topic: Menstrual disorders
If malicious changes are suspected, the principle of fractional abrasion be carried out, i.e. the separate scraping of the uterine cavity and neck in order to be able to process the samples separately for histological examinations. Hysteroscopy often allows an assessment of the underlying complaints and enables a better diagnosis.
The therapeutic indications include:
- the removal of fibroids or polyps
- the loosening of adhesions or sticking of the uterine lining (Synechiae)
- the removal of the mucous membrane (Endometrial resection / ablation) for heavy bleeding
In addition, after an abortion, the uterine cavity is scraped off during hysteroscopy to loosen fruit residues and prevent infections. In general, the attempt is not made to perform the uterine specimen during the menstrual period, but in urgent cases, for example, it can be scraped off during the period.
Read more on the topic: Uterine scraping
Is it possible without anesthesia?
General anesthesia can be dispensed with in the case of diagnostic endoscopy. The examination can be uncomfortable, but the pain is usually only mild and limited. Local anesthesia is performed if desired. At her request, the patient can even follow the diagnostic endoscopy with some doctors on a screen.
In the case of therapeutic, surgical uterine endoscopies, however, anesthesia is always necessary. If the patient was conscious, the pain would be too great and the intervention would not be feasible due to physical defensive tension. With regard to pain-relieving options, epidural (PDA) or spinal anesthesia are in rare cases also options for a uterine specimen.
Read more on the topic: Anesthesia
How big is the pain?
The pain after an endoscopy is very individual and varies from patient to patient. Not only does the procedure itself play a role, the patient's personal pain perception and pain tolerance also play a role. After an endoscopy, patients usually complain of pain that is similar in intensity to menstrual cramps or slightly greater than them.
The pain also differs between the patients after a diagnostic or therapeutic endoscopy, as significantly more tissue is manipulated and irritated in the latter. As a rule, the symptoms that last a few days can be managed with light painkillers. The doctor should be consulted about which preparations are recommended for this purpose. Some active ingredients, such as aspirin (Acetylsalicylic acid), increase the bleeding tendency, which should be taken into account in a therapeutic endoscopy due to the frequent secondary bleeding. In general, persistent and severe pain requires a doctor's consultation to rule out possible complications.
Is an outpatient endoscopy possible?
Since this is one of the most common gynecological routine examinations, which can usually be carried out very quickly, the vast majority of diagnostic uteroscopy can now be done on an outpatient basis. Whether an inpatient or outpatient endoscopy should be performed depends on the underlying indication. In the case of therapeutic endoscopies, an inpatient stay may be necessary, although most patients can leave the hospital the day after the operation.
Smaller polyp removals, for example, can also be carried out on an outpatient basis and after a sufficiently long period of monitoring in the recovery room, the patient can go home on the same day, provided the patient is in good general condition and with medical consent. The disadvantage of outpatient treatment, however, is that in the case of a diagnostically planned mirroring, changes that may require treatment may not be removed in the same procedure. A second uterine specimen may therefore be necessary.
It is important to discuss the necessary rules of conduct to be followed for the time after the operation with the doctor for all uteroscopy and to carry out any necessary follow-up examinations. Care should also be taken not to overuse yourself, especially during outpatient examinations. Patients who leave the hospital on the same day often forget to take a long time to rest.
What are the risks?
The uterine endoscopy is a low-risk procedure. However, like any medical procedure, the examination can have potential complications. After the endoscopy, the patients often have abdominal pain that lasts for a few days, which is similar in intensity to menstrual cramps. Spotting is particularly common with therapeutic uteroscopy and usually lasts a few days.
There is also the risk of infection of the uterus, fallopian tubes and ovaries from germs carried over during the procedure. Therefore, if you have unexplained pain or fever, you should see a doctor after a hysteroscopy. It can also be used for perforation, i.e. the rupture and injury of the uterus caused by the instruments used with subsequent bleeding into the abdomen.
Depending on the extent of the bleeding, it may be necessary to stop it by surgery; in minor cases, close monitoring of the patient's vital parameters is sufficient. An extremely rare complication of the procedure is the emergency removal of the uterus if it has been severely injured and is bleeding uncontrollably. In rare cases, the use of blood reserves is necessary. Another rare scenario is a build-up of water in the lungs after the endoscopy, which is caused by the excessive use of irrigation fluids in the uterus.
You might also be interested in the topic: Uterine inflammation
Is it possible to have a hysteroscopy during pregnancy?
A hysteroscopy is relatively contraindicated during an intact pregnancy, which means it should not be performed. In urgent exceptional cases, however, mirroring is possible. Due to the danger to the fetus from the medical instruments introduced, it is not recommended.
If the pregnancy is no longer intact and the fruit does not shed on its own or if parts of the fetus or placenta (placenta) remain in the uterus, a Abortion curettage made, i.e. a scraping of the remaining fetus. This procedure can be viewed hysteroscopically or checked for completeness using ultrasound.
Should a uterine specimen be performed before an artificial insemination?
In patients who suspect possible restrictions in the implantation conditions of the uterus, it is recommended that prior to a planned artificial insemination (In Vitro Fertilization (IVF)) to perform a diagnostic endoscopy. In this way, possible obstacles to embryonic implantation such as myomas, polyps, etc. can be discovered and treated later.
This enables the implantation conditions to be optimized and the success rate of an IVF to be increased. Furthermore, the reflection can be used to determine the individual nature of the uterine cavity and thus the best area for the later embryo transfer.
Read more about: In-Vitro-Fertilization
Uteroscopy after a miscarriage
After a miscarriage, a uterine specimen can be useful. The aim here is to find any remaining fruit and placenta residues and, if necessary, by means of scraping (curettage) completely. This can reduce the risk of infections. Also can with repeated miscarriages, so-called habitual abortionswho have hysteroscopy performed for diagnostic purposes.
In this way, possible causes of the tendency to abort can be determined and potential obstacles to implantation in the uterine cavity can be found. Ideally, they can be removed in the same procedure, for example if there are anatomical obstacles.
Duration of a uterine specimen
The duration of an endoscopy depends on the underlying indication. If it is only a diagnostic intervention, the examination by an experienced doctor takes about five minutes. If, on the other hand, scraping is planned, the duration of the operation is around 15-30 minutes.
Are ablations (Resections) If necessary, the endoscopy may take up to 45 minutes. All figures mentioned refer to normal cases; in the case of complications or anatomical peculiarities, the duration of the uterine surgery can be extended accordingly.
Is that a cash benefit?
The reimbursement of the costs of a hysteroscopy depends largely on the indication. In the medically justified cases, it is usually a matter of cash benefits. These include, for example, uteroscopy as part of miscarriages and the removal of myomas or polyps.
However, if the examination is carried out for personal reasons, such as in the context of fertility treatment, the patient may have to bear the costs herself. In general, it is advisable to clarify the cost issue with your health insurance company before the examination.