Facial pain
General
Pain in the face is incredibly diverse, so that it is difficult to determine a cause without a more detailed description and investigation.
First of all, facial pain really has to be related to the face, i.e. cheeks, jaws, cheeks, temples up to the ears, the mouth and nose area, the area around the eyes and all associated bone and cartilage parts.
This also includes the tongue, throat and roof of the mouth.
Read more on this topic: Pain over the eyes

The headache must be clearly separated from this - although it can of course happen that someone suffers from facial pain and headache at the same time. If your forehead hurts in connection with a headache, it also belongs more to the headache category.
One can differentiate between different forms of facial pain, depending on how the patient describes it. Whether chronic or acute, whether a connection between the pain and certain situations or moments can be identified. The localization of the pain in its strongest form, whether and if so where it radiates. The extent of the facial pain in particular could provide an indication of whether the pain originates from a certain nerve and spreads along it, which would be expressed in typical painful areas.
causes
The most common and most important cause of facial pain is neuralgia, pain emanating from the nerves, which those affected often describe as very violent, suddenly shooting in and as piercing or cutting. The pain is usually classified as a 9-10 on a pain scale of 1-10.
The pain can occur spontaneously or be triggered by certain sensations of irritation, such as touch, warmth, cold or even light. The best-known form of neuralgia that occurs in the face is probably trigeminal neuralgia.
A problem in the therapy of such nerve pain is that most classic painkillers have no effect on them. For this reason, active ingredients are mainly used for therapy that are also used to treat epilepsy (Anticonvulsants) can be used, carbamazepine as an example. If the symptoms are not satisfactorily alleviated, depending on the cause, local use of anesthetics or surgery may also be considered.
The underlying cause cannot always be found. These include, for example, irritation of the nerve from a neighboring blood vessel, sometimes an underlying disease may be responsible for the pain, such as a head injury, multiple sclerosis or a tumor.
diagnosis
The typical course of pain and its spread are extremely characteristic, so that the description of the pain attacks can provide an important indication of the presence of neuralgia. The diagnosis should be confirmed by a neurologist, who will rule out other causes with the help of imaging tests and the examination of blood and cerebrospinal fluid samples and make the exact diagnosis.
If a clearly identifiable cause can be found, it should be treated. However, if there is no identifiable underlying disease, medication and, under certain circumstances, even surgery is recommended.
unilateral facial pain
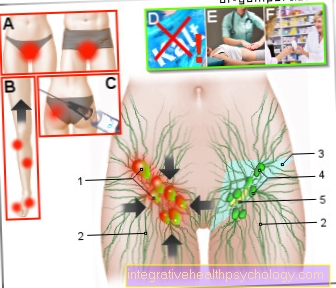
The information as to whether the facial pain is only present on one side or whether it affects the entire face is very important as it is a guiding indicator in the context of diagnostics. Certain diseases that lead to nerve pain traditionally only occur on one side.
These clinical pictures include neuralgia, for example of the glossopharyngeal nerve. Similar to trigeminal neuralgia, the nerve of the same name is strongly irritated and leads to correspondingly severe pain in its supply area. The tongue, the pharynx and the parotid gland on one half of the face are particularly affected. A difference in frequency between the two halves of the face could not be proven.
Another disease, the classic characteristic of which is unilateral facial pain, is shingles of the face. This can affect different nerves in the face, but the typical nerve pain and skin changes such as reddening and blistering usually occur. However, a fast therapy should be aimed for, since otherwise, in severe cases, the nerves may fail.
A very localized pain on the left side of the lower jaw can indicate an acute heart problem, such as a heart attack. However, these are usually accompanied by other symptoms such as tightness, pain in the upper abdomen or the left arm and feelings of fear.
Find out more about the topic Nerve pain on our side.
bilateral facial pain
Bilateral facial pain can be due to variable diseases, so it makes sense to consult a doctor in the presence of bilateral pain that lasts longer in order to be able to rule out possible serious causes. Probably the most common cause of sinus infection is that it usually goes away on its own.
However, facial pain that occurs on both sides can also be an indication of an underlying systemic disease. For example, bilateral nerve pain in the facial area is often reported in patients with multiple sclerosis (MS). As the disease progresses, increasing loss of nerve function is also possible.
Furthermore, bilateral facial pain can also be caused by polyneuropathies. The causes of polyneuropathy can be very diverse and range from alcoholism and diabetes to treatment with certain chemotherapeutic agents. Neuropathy is differentiated from neuralgia in that it usually also has sensory disturbances such as tingling and the focus is not on pain.
If you are interested in the distinction between neuralgia and neuropathy, then read the following article: Polyneuropathy and neuralgia
Trigeminal neuralgia
Trigeminal neuralgia can be recognized by a characteristic pain localization: over the eyes, on the cheekbones or in the chin area. The patients are symptom-free between the individual, usually very short attacks, but in pronounced cases there can be a very high frequency of attacks with almost no pauses between the attacks.The localization is based on the physiological function of the nerve, which is responsible for the sensitive supply of the front half of the face and the motor functions of the temples and masticatory muscles. Damage to it can occur throughout its course.
Due to the strong psychological stress, depressive moods often develop.
Since the individual pain attacks are of very short duration, pain medication usually does not help or does not help enough. So-called anti-epileptic drugs, drugs that are used to treat epilepsy, are more effective. Their effect is based on an inhibiting influence on the excitability of nerves, so that they can prevent attacks and desensitize the nerve.
As part of the potential surgical therapy, the primary aim is to relieve the nerves and remove any pressure stimuli from an adjacent, pulsating blood vessel (decompression). With the help of thermocoagulation, radiological procedures or a so-called CyberKnife, you can also interrupt the transmission of pain. However, the risk of undesirable side effects such as sensory disorders, hearing and vision problems is very high and relapses are by no means excluded.
If you are interested in the topic, read our special article on Trigeminal neuralgia
"Atypical facial pain"
In contrast to tigeminal neuralgia, which is called "typical facial pain", There is also the group of"atypical facial pain“.
Facial pain is classified in this category if the criteria for neuralgia are not met. Tension in the neck muscles, but also in the facial muscles, can lead to this pain. The exact mechanism is not yet understood, but it is assumed that the free nerve endings are irritated by the tense subcutaneous connective tissue and that this irritation can radiate into the facial area.
Find out more about the topic here: Nerve inflammation on the face.
Those affected are increasingly female and often describe the symptoms as a dull pain that is difficult to define, relatively deep-seated and often in the area of the upper jaw or the eye sockets.
At times, hypersensitivity to touch can also occur in this area. It is not uncommon for patients to go to a dentist first, as they classify the pain as deep-seated and this sometimes leads to unnecessary tooth extraction. This does not improve the symptoms, however, so that further interventions are often carried out, which, however, only aggravates the unrecognized atypical facial pain and can contribute to chronicity.
The patients are frustrated, discouraged and no longer know what to do, depression and anxiety disorders can occur. "Atypical facial pain" should be carefully examined and the possible causes must be clarified urgently.
After patient education has been given, medication with tricyclic antidepressants can provide pain relief.
Massages, cold and heat treatments and other manual therapies are also very promising. It is best to choose a combination of drug, psychotherapeutic and manual therapy. Surgical interventions, however, are not advised, as they can promote chronicity.
Facial pain related to stress
Stress, like many other factors, can be a cause of what is known as "atypical facial pain". Initially, the pain is usually limited to a certain skin area, which usually spreads over time. In about 30% of the cases, both halves of the face are affected. In addition, with atypical pain it is rather rare that the pain occurs episodically, as is the case with trigeminal neuralgia. Usually it is a constant pain. Many sufferers report that the pain decreases at night, but remains consistently strong throughout the day. The diagnosis of "atypical facial pain" is usually very tedious, as all possible causes have to be ruled out.
Shingles on the face - herpes zoster as the cause
Another possible cause of facial pain is that Herpes zoster, popularly known as shingles.
The clinical picture of herpes zoster is caused by the reactivation of the chickenpox virus (Varicella zoster virus) triggered as part of an immune deficiency. On the one hand, these viruses primarily cause chickenpox, which soon disappears after successful treatment. But after the acute symptoms of chickenpox have subsided, the viruses attach themselves to the cranial nerves or nerves of the spinal cord and nest there.
However, the human immune system usually ensures that the virus can no longer multiply and consequently the disease does not break out again.
If the person gets older or is weakened by another illness or stress, it can happen that the immune system is no longer strong enough and the virus spreads again. It travels along the affected nerves to the skin, where it causes the typical belt-shaped rashes. The rash is accompanied by very severe pain, which can persist for some time after the external symptoms have healed. It is also important that the varicella zoster virus is a highly infectious virus, direct contact (Smear infection) or airborne infection (airborne) are possible.
This clinical picture is an option for your complaints, then read our article on the subject Shingles.
multiple sclerosis
Multiple sclerosis is a degenerative autoimmune disease in which the protective insulation of the nerves, the so-called myelin sheath, is destroyed by the body. As a result, the speed at which the nerves conduct stimuli can be greatly reduced, which can result in a restriction of their normal function or even complete failure.
The symptoms of this disease are very diverse, as all nerves can be affected by this process. These range from slight sensitivity disorders to a complete loss of nerve function. These breakdown processes on the nerves cause severe irritation and severe nerve pain, a so-called neuralgia, arise. If the sensitive nerves of the face are affected, severe facial pain occurs, which can occur on one side or on both sides.
Find out more at Multiple sclerosis.
migraine
It also often happens that facial pain occurs as part of a migraine.
The patients then often complain of pain rising from the neck, which extends over the entire head and particularly affects the forehead and eye region.
The migraine headache usually manifests itself as a pulsating, stabbing pain, together with strong accompanying symptoms such as nausea, vomiting, sensitivity to light and noise and an increased need for rest on the part of those affected.
If the pain is mainly reflected in the face, many patients mistakenly go to an ophthalmologist or ENT doctor first, but they cannot help in this case. In order to be able to diagnose a migraine, both a physical and a neurological examination is useful in order to be able to rule out any other diseases.
Pain associated with a cold
The most common cause of facial pain is a normal cold. The focus of the complaints is usually not on the pain, but on the typical symptoms of a classic cold and a general feeling of pressure in the nose and sinuses. Thus, the cause of the facial pain is usually clear here. With a slightly more severe cold that lasts longer, it can expand into the sinuses and lead to inflammation. This can be accompanied by severe facial pain and headaches.
Sinus infection
A sinus infection called a Sinusitis, is one of the most common causes of bilateral facial pain, which is usually accompanied by a strong feeling of pressure. The diagnosis of the disease is usually easy, as this inflammation is associated with a blocked nose and pain in the upper jaw or forehead. If the pain and the feeling of pressure get worse when you put pressure on the upper jaw and forehead or when you lean forward, the diagnosis is almost certain.
To treat this inflammation, decongestant nasal sprays are first prescribed, which usually bring about a rapid improvement in pain. If the inflammation cannot be cured adequately with drug therapy, surgery must be performed in rare cases. In the majority of cases, however, a simple sinus infection will go away on its own within two weeks.
For more information on the topic, see our article Sinus infection.
Face pain from drafts
If a person is exposed to increased drafts, as is the case, for example, when sleeping under an air conditioning system, the irritation of the skin can lead to slight facial pain. It is believed that this irritation leads to slight swelling of the skin, which then pinches the nerve branches. This constriction is then felt as pain. However, those affected do not have to worry because these symptoms almost always disappear quickly by avoiding drafts. If the pain is still there after a few days, it is advisable to see a neurologist to rule out other causes.
Cervical spine discomfort
Recent studies have shown that facial pain can also be triggered by problems in the cervical spine (cervical spine). Pain and functional restrictions in the area of the cervical spine are usually summarized under the so-called cervical spine syndrome. The chronic form of this syndrome can drag on for several months and is usually associated with severe pain and muscle hardening, which can lead to restricted mobility. The irritation of these structures can spread over time and, in addition to neck and shoulder pain, it can also radiate into the facial area, especially the cheeks and forehead. In the case of facial pain associated with pain in the cervical spine, a connection between these two symptoms should also be considered.
If you have a cervical spine syndrome as a cause, read the following articles: Symptoms and Treatment of the cervical spine syndrome
Fibromyalgia
Fibromyalgia is a chronic disease that is characterized by chronic, therapy-resistant muscle pain that can change its location. Furthermore, there is a strong sensitivity to pressure and there are other accompanying symptoms such as swelling, fatigue or sleep disorders. The exact cause and the development of the disease (Pathogenesis) are largely unexplained to this day.
If the muscles of the face are affected by this condition, it can lead to severe facial pain that gets worse when you talk or chew.
The symptoms of fibromyalgia can only be influenced to a limited extent by the current therapy standards. As part of the so-called multimodal pain therapy, attempts are made to alleviate the symptoms as much as possible through various therapeutic approaches. In addition to the drug treatment with antidepressants, relaxation exercises, physical therapy and a change in diet are the focus of the therapy.
Further information can be found on our corresponding topic page Fibromyalgia.
Facial pain caused by craniomandibular dysfunction
Another possible cause of facial pain, especially when described as originating from the jaw or TMJ, is craniomandibular dysfunction (CMD). In the specialist literature, the CMD is also often referred to as myoarthria of the masticatory system and relates to the following anatomical structures: the temporomandibular joint, the masticatory muscles and the temporal muscle are involved.
The cause of pain lies in the temporomandibular joint itself. This consists of the skull bone and the jaw bone, connected by a small disc of cartilage in between. If the lower jaw is now moved, this cartilage slides between the two bones and reduces the resulting friction. Sometimes there may be crunching noises, but these are quite normal.
If you notice that these noises occur more frequently or if the patient complains of long-lasting pain, medical attention is required.
Tension of the masticatory muscles or wear of the cartilage disc are often the cause. Nocturnal teeth grinding is often an expression of tension in the temporomandibular joint and during the day it can lead to severe jaw pain, especially in the temples.
Grinding teeth can be treated relatively easily. A bite splint is made, which on the one hand relieves the joint and on the other hand tries to improve the unfavorable learned movement patterns in the jaw by changing position. Physiotherapy with progressive muscle relaxation is also recommended.
If necessary, the use of medication can also be discussed, primarily tricyclic antidepressants, which may make you tired as a side effect.
If the cause of the craniomandibular dysfunction is wear and tear of the cartilaginous parts of the temporomandibular joint, surgical removal of the cartilage disc can improve the patient. However, if the symptoms are more likely to be caused by inflammation of the temporomandibular joint, anti-inflammatory drugs can help.
For more information, see Crandiomandibular dysfunction
Thyroid disease
In rare cases, facial pain can also be caused by a disease of the thyroid gland. This is especially the case with a certain type of inflammation called Hashimoto's thyroiditis. In this case, the body produces (auto) antibodies against its own thyroid; it is therefore an autoimmune disease. The result is inflammation, which usually leads to an underactive thyroid, but also to pain that can spread to the neck and face.
Dental causes
If the pain is more localized in the area of the mouth or the oral cavity, other causes are more likely. In the oral cavity itself, for example, inflammation of the mucous membrane can occur, especially in young adults, breaking the whiteness teeth can be an option or bacteria or viruses can have lodged in the gums.
Of course, the teeth themselves also have sensitive nerves that are primarily sensitive to temperatures and chemical substances (acid contained in food) respond.
Normal, healthy teeth are able to hold off these stimuli without any problems, but the tooth decay has only manifested itself and the dentin lies (Dentine) free, the nerve no longer has a protective covering and transmits the stimulus to the brain in the form of pain.
The most common cause of pain in the mouth is pulpitis, an inflammation of the nerves and blood vessels inside the tooth pulp (pulp) lie.
The pain that this causes is very intense and sometimes radiates far. The teeth burn, squeeze and pound painfully even at night. At the beginning it may be that you cannot assign the pain to a single tooth. This is because the anatomical structures in which the inflammation takes place in pulpitis are immobile, i.e. solid bones and teeth. If there is an inflammatory reaction in the tissue, the blood flow to the tooth is reactively increased. Due to the tightness, however, it is not possible for the tissue to expand and so, in addition to the inflammation pain, there is also pressure and stretch pain that can extend over the entire jaw.
After treatment of the pulpitits, i.e. removal of the cause of the inflammation, it either recedes (reversible pulpitis) or it was already too advanced and continues (irreversible pulpitits), which leads to the death of the tooth nerve.
If this process proceeds very slowly, the patient may not even notice the death of the nerve, since the loss of the nerve also loses the ability to perceive pain. It often happens, however, that a new focus of inflammation later forms at the site, now localized in the bone at the tip of the tooth: apical periodontitis.
In order to treat this, the root canal must be opened and the remaining nerve and vascular residues completely removed. Then you disinfect the cavity several times and insert a filling to prevent bacteria from settling there again and causing inflammation.
Very similar to the painful character of pulpitis, but fundamentally different in its cause, is atypical odontalgia, the so-called "Phantom toothache". This is characterized by long-lasting pain in an area where a tooth was previously pulled. Even with thorough examinations and imaging procedures, it is not possible for the doctor to pinpoint a cause for the pain, so that one assumes that the pain originates from damage to the nerve fibers in the affected tooth or its immediate vicinity. Often times, patients complain of an exacerbation of pain in cold weather. Pulling the tooth prematurely is not advisable, as this does not result in improvement, but in the worst case even deterioration.
Find out more about the topic here: The atypical odontalgia
Pain can also occur in the tongue area. A relatively common occurrence, especially in older women, is the burning tongue symptom.
However, the cause of the burning pain has not yet been clearly identified; damage to the thin nerve fibers that run in the tongue and the entire mouth area is likely to be the cause.
Complaints after dental treatment
It is not uncommon for patients to complain of facial pain after dental work. The upper and lower jaw are sensitively supplied by the trigeminal nerve. However, since this innervates the entire face sensitively, irritation of the nerves in the area of the jaw can spread to other areas of the face. Such irritation is possible, for example, in interventions with dental fillings that are relatively close to the nerves. The pain can pull up into the ear and be very uncomfortable.
If the pain persists a few days after treatment, you should see a dentist again so that damage to the nerve can be excluded.
Homeopathy for facial pain
Homeopathic therapy for facial pain depends on the underlying cause. For example, other remedies are used in trigeminal neuralgia, such as sinusitis.
Belladonna, the poison of the deadly nightshade, is one of the most well-known remedies in neuralgia therapy. This is used in the general therapy of painful conditions and alleviates the pain that is triggered by pressure and vibrations. Other remedies that are used in homeopathic therapy are Aconitum napellus, Arsenicum album and Thuja occidentalis.
However, it is important to point out that homeopathic therapy alone is usually not sufficient to relieve the pain of trigeminal neuralgia. This therapeutic approach should therefore be viewed as a supplement to classic drug therapy.