Hemangioma
definition
A hemangioma is also known colloquially as a blood sponge or strawberry spot. The hemangioma is a common benign tumor (swelling, increase in the volume of a tissue) of the vessels and arises in the embryonic development in which small vascular plexuses form. As a rule, a blood sponge develops in babies in the first four weeks of life; older children or adults rarely develop a hemangioma.
A hemangioma belongs to the group of angiomas. An angioma is a tumor-like neovascularization or developmental malformation of the vessels. The origin of hemangiomas in infancy and childhood is still unclear.

Occurrence
As a rule, hemangiomas are still very small at birth, but in some cases they can increase significantly in size (especially in the first year of life). Most often it is a hemangioma innate and can show different growth tendencies. For the most part, hemangiomas form again by itself Most blood sponges do not show a tendency to become malignant later. However, there are also hemangiomas that are not congenital and only appear during Adulthood occur. This form of hemangioma occurs mostly after the 3rd decade of life on.
A hemangioma can appear anywhere on the body and also on the internal organs. In approximately two thirds however, there is a hemangioma in the cases Head and neck area. 30 percent the blood sponges are in the liver localized. These are often noticed as incidental findings during a liver ultrasound exam.
About 3 to 5 percent of infants have one or more hemangiomas at birth. At Premature babies the blood sponges are a little more common. Because of this, the hemangioma is the most common tumor in toddler age. Girls are two to three times haemangiomas more often than boys.
Treatment for hemangioma can be dispensed with in most cases as it will go away on its own. Early treatment is advisable for growing blood sponges.
The so-called hemangioma is not to be confused with a hemangioma Stork bite. This is also an expansion of blood vessels, but the stork bite does not protrude above the skin level.
Symptoms

Usually hemangioma does not cause symptoms. On the surface of the skin or Mucous membrane blood sponges located as reddish spots or Surveys to recognize. Hemangiomas deeper under the skin can bluish appear and one Bruising on the baby (Hematoma) resemble. Read our topic: Bruise in the child
In the first few months of life, the hemangioma can grow at very different rates. Usually it comes to one in later infancy Growth stall and disappears on its own after a few years with nothing left behind. A clear hemangioma, for example in the face localized can be emotionally stressful for cosmetic reasons. Physical symptoms may occur depending on the location of the blood sponge. For example, a hemangioma can be am eyelid make it difficult to open the eye Armpit blood sponges can pressure sensitive be and cause pain.
Pain
Most people who have hemangioma do not experience pain. Pain can result from a mass in the internal organs, but does not affect the much more common skin hemangiomas. In so-called cavernous hemangiomas, thrombi can form. This means that blood clots will form in the hemangioma because the flow is different. If these thrombi are washed into other parts of the body, they can lead to vascular occlusions with severe pain. A doctor should be consulted immediately.
Hemangioma in the baby
Most, about three quarters, of all hemangiomas occur in infancy. At birth, hemangiomas are often not clearly visible and only the increase in size in the first year of life allows the hemangioma to become visible. The frequent occurrence of hemangiomas in infancy can be explained by the fact that it is an embryonic tumor. A hemangioma, also known as blood sponges, consists of cells that humans only produce in their embryonic period and infancy. About three to five percent of all babies are affected. Premature babies are affected up to twenty times more often than full term babies.
Most babies wait to see how the hemangioma develops, as many hemangiomas regress in the first few years of life and hemangiomas do not degenerate into cancer. Treatment of the baby is sought if the hemangioma is particularly large or the location is unfavorable. In babies and toddlers, drug treatment with the beta blocker propanolol is permitted, which can contribute to regression. Blood sponges are usually completely painless for the baby and do not restrict it in everyday life.
Read more on the subject at: Blood sponge in the baby
Forms of hemangioma
Capillary hemangioma
One form of hemangioma is the so-called Capillary hemangioma. It derives from the Capillaries, the smallest blood vessels in the human body. Capillaries form a fine network in the organs and tissues of the body and enable the exchange of oxygen and nutrients between blood and body tissue. About 30 to 40 percent of all vascular tumors are to be assigned to the capillary hemangioma.
A capillary hemangioma shows up on the skin as a bright red and something raised vascular plexus. It occurs very much frequently (one in 200 births) and usually shortly after birth on. Capillary hemangioma often increases in the first few months of life size to. However, more than 70 percent the blood sponges up to 7th year of life completely back again.
A treatment is at uncomplicated hemangiomas unnecessary. However, if the capillary hemangioma is in face or in Buttocks or genital area localized, therapy should be initiated early. Therapy can be done using Laser technology or Cold therapy (Cryogenics). For very large blood sponges, treatment with Chemotherapy drugs (inhibit the growth of cells) Cortisone or with Beta blockers (antihypertensive drugs that also work on certain receptors in the hemangioma vessels). In very rare cases a surgical intervention to be required.
Cavernoma
The so-called cavernous hemangioma or cavernoma is in some cases already visible at birth, but more often it occurs in the first days of life. A cavernoma is a bright red vascular malformation with large vascular cavities. Depending on the skin layer in which a cavernoma occurs, it is divided into a cutaneous, cutaneous-subcutaneous or subcutaneous hemangioma.
About 80 percent of all cavernomas regress on their own. Cavernous hemangiomas can bleed profusely, which is a dangerous complication of this form of hemangioma. Large cavernomas can lead to growth problems in the arms or legs of children. Early therapy should be initiated in these cases. The cavernous hemangioma can be treated well and is therefore usually treated nowadays.
A cavernoma can also occur in the central nervous system, i.e. in the brain or spinal cord. This can trigger epileptic seizures or neurological deficits (e.g. paralysis, sensory disorders, etc.). The most serious complication of a cavernous hemangioma is cerebral haemorrhage. Depending on the size of the cavernoma, the probability of bleeding is 1 to 10 percent per year. If bleeding occurs or if epileptic seizures occur that cannot be treated otherwise, a cavernous hemangioma in the area of the brain is removed by surgery. Such an operation is not generally recommended if the findings are symptom-free.
An important special form of the hemangioma is the cavernous hemangioma. To learn more about it, read: Cavernous Hemangioma - How Dangerous Is It?
Sclerosing hemangioma
Especially in the middle adulthood a sclerosing hemangioma can occur. This form of the blood sponge is relatively mobile, up to one centimeter in size Lump in the skin (Dermis) or subcutis (subcutis). The sclerosing hemangioma grows slowly and is as benign tumor on the skin. It can occur on any part of the skin of the body, but occurs preferentially on the extremities on. Treatment of the sclerosing hemangioma is not absolutely necessary. However, the blood sponge can be very simple at the request of the person concerned surgically removed. In approximately five percent of the cases it can become one Recurrence (Relapse) of the sclerosing hemangioma.
Hemangioma in the brain
In principle, hemangiomas can occur wherever there are blood vessels. It is not uncommon for hemangiomas to occur in the brain area. Not all of these angiomas lead to the development of discomfort. However, this is largely dependent on the size and the exact location. This can lead to mild symptoms such as headaches or dizziness, which, however, often cannot be diagnosed as such in young children. However, impairment of vision, sensitivity disorders, speech disorders, memory disorders and other neurological deficits as a result of displacement by a hemangioma are also possible.
Another reason is that the weaker vascular wall in the area of the hemangiomas means that blood pressure cannot be built up as high as would be necessary for adequate supply to the surrounding areas. These symptoms represent a clear indication for therapy. Depending on the exact location, there are different therapy options such as radiation, one Embolization (= Closure of the hemangioma) and a surgical procedure in question.
Hemangioma of the eye socket
A hemangioma can also be found in the Eye socket (Orbit) occur. The eye socket is one of Skull bones Surrounded area in which comparatively very few tumors occur. Because of this, the hemangioma is the most common benign tumor the adult eye socket. The hemangioma of the eye socket is often discovered as an incidental finding during skull examinations. In some cases it makes its way through a Change of position of the eyeball noticeable as the hemangioma can increase in size and displace the eyeball. The diagnosis can be made by a Angio magnetic resonance imaging (Nuclear spin to show the vessels) or one Computed tomography (CT) the Sinuses be asked.
A hemangioma of the eye socket (also Orbital hemangioma called) occurs in middle age on. The slow but steady growth of the hemangioma leads to complications such as a progressive one Exophthalmus (pathological protrusion of the eyeball from the eye socket), one Decrease in visual acuity (Visual acuity reduction), Farsightedness (Hyperopia) or Diplopia (Seeing double images) come. Treatment is only used for steadily growing hemangiomas of the eye socket that cause discomfort. For this is a surgical intervention required, in which the vascular tumor is first obliterated and then removed. Since such an operation involves many dangers, hemangiomas that do not cause discomfort should be left in place. Regular checks should be carried out in these cases.
Hemangioma on the lip
Hemangiomas in the lip area are relative frequently. They are often treated very early for aesthetic reasons, but this should also reduce the risk of functional disorders. If it is a rapidly growing hemangioma, this can be in the lip area Disruption of food intake and the Jaw and tooth development come. In addition, there is a risk that, above a certain size, the lip will remain permanently deformed even after the operation. All of these are reasons why, with a diagnosed hemangioma on the lip, action is taken relatively early and one does not wait for the tumor to recede itself, as is the case with other locations. Furthermore, the smaller the hemangioma, the easier the removal. In a guided therapy, gentle techniques that produce aesthetic results can be used.
Hemangioma of the skin
Hemangiomas appear in the skin area very often and can be very different in their characteristics. They usually appear as dark blue to blackish blue areas that are either flat or spherical. The structure is soft and often expressible. Their size can be from a few millimeters up to 10 cm vary. In the first months of life there is rapid growth, which, however, slowly decreases after the first 9 months of life.
Fortunately, most skin hemangiomas show one after the ages of 6–9 spontaneous regression on. In many cases, no signs or only small scars remain. Life-threatening complications are not to be expected.Skin hemangiomas, for example, usually only require treatment if they have exceeded a certain size. However, they are often removed beforehand for aesthetic reasons.
Hemangioma of the liver
The most common benign neoplasm (neoplasm) of the liver is the hemangioma. In most cases, the hemangiomas of the liver are discovered incidentally during an ultrasound examination (sonography) or during an MRI of the liver. These hemangiomas are harmless and can be left in the liver without therapy. Only when a hemangioma is located on the surface of the liver can it rupture and bleed. A deeper hemangioma of the liver can in rare cases lead to an obstruction of the drainage of the bile. The benign cells of the hemangioma do not degenerate into malignant tumor cells.
You can find a lot more information under our topic: Hemangioma of the liver
Hemagioma of the spleen
Hemangiomas are those most common benign tumors of the spleen and are often an incidental finding during an ultrasound examination. In many cases these are unproblematic and go away on their own after a few years. However, during this time there is a risk of a Splenomegaly, so one Enlargement of the spleen, and a slightly higher risk for Bleeding within the spleen. Here there is initially a bleeding into the tight Spleen capsule. If the bleeding is heavy, the spleen capsule can rupture and cause extensive internal bleeding. However, this still occurs very rarely. In most cases, hemangiomas of the spleen do not require treatment and are only treated if they lead to symptoms.
Hemangioma on the spine
Hemangiomas can occur not only in the skin, but other areas of the body as well. The hemangioma vertebra is a hemangioma in the vertebral body. Women are affected more often than men. A hemangioma vertebra is usually an incidental finding, as it only causes symptoms in very rare cases. The hemangioma is visible in computer tomographic images or in magnetic resonance tomography. Treatment is rarely necessary. In the case of symptoms that occur rarely, pain therapy or surgical therapy can be sought.
More about this on our website Hemangioma on the spine
Angiomatosis
Hemangiomatosis describes the simultaneous presence of many hemangiomas. In many cases, hemangiomatosis is a component of other diseases, such as Sturge-Weber syndrome or Mafucci-Kast syndrome. If the internal organs, especially the liver, are involved, there is an acute risk of death for the affected newborn as the hemangiomas change the blood circulation. There are many different forms of hemangiomatosis. These range from a restriction to the skin to hemangiomas in all organs.
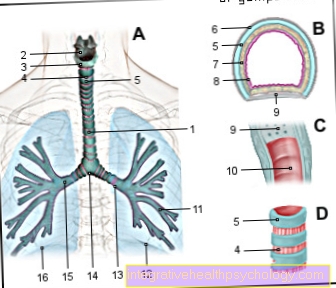
Benign neonatal hemangiomatosis is the most harmless form because it is simply a collection of skin hemangiomas. The very rare diffuse neonatal hemangiomatosis also affects all internal organs. The cause for this is not yet known. Capillary pulmonary hemangiomatosis particularly affects the lungs and can therefore lead to pulmonary hypertension and cardiac stress. In addition to these forms, there are other genetic causes of hemangiomatosis. Depending on the location of the hemangioma, various accompanying diseases and complications occur. In most cases, hemangiomatoses are chronic diseases in which only the symptoms can be alleviated.
Kasabach-Merritt syndrome
The so-called Kasabach-Merritt syndrome is due to the appearance of a special form of Giant hemangiomas marked. The disease goes with one Consumption Coagulopathy (Coagulation disorder) hand in hand, which means that there is a consumption of coagulation factors and Platelets (Platelets) is coming. In the hemangiomas there is the formation of Blood clots (Thrombi) and through the consumption of platelets there is an increased Bleeding tendency.
The giant hemangiomas can, for example, extend over an entire limb. So far, the origin of hemangiomas is unknown, in some cases they regress on their own. Come for treatment of the condition Laser surgery, interventional radiology or drug therapies (e.g. with Cortisone) into consideration.
What should I do if a hemangioma is bleeding?
A hemangioma is a benign tumor of the blood vessels and is accordingly well supplied with blood. Injury to the hemangioma can therefore lead to profuse bleeding. In a person with normal blood clotting, the bleeding should stop on its own or with a little external pressure.
If the bleeding persists, a firm bandage should be placed around the hemangioma and a doctor should be consulted who can properly treat the bleeding. Bleeding from a hemangioma cannot be treated any differently than any other bleeding wound and is no more dangerous than any other bleeding.
Can a Hemangioma Become Malignant?
A hemangioma only becomes malignant in very rare cases. A degeneration cannot be foreseen, which is why regular control of hemangiomas makes sense. If a hemangioma is malignant, it has a high growth rate. In addition to the actual malignant degeneration, a capillary hemangioma can develop into a cavernous hemangioma. This is not a malignant tumor, but thrombi can form in the hemangioma and thus also lead to serious complications.
How can you remove a hemangioma?
There are many different methods of removing a hemangioma today. The fundamental direction here is to try to remove as few hemangiomas as possible openly surgically, but through minimally invasive or non-invasive therapies to treat. Which therapy option is ultimately chosen depends heavily on growth, size, location and existing complications. For hemangiomas of the internal organs, such as the spleen, is usually one laparoscopy carried out. Here only very small cuts are made in the building ceiling and operated through them with elongated instruments. This method has meanwhile proven itself and is used in many areas of surgery.
Another therapy option is this Laser treatment of superficial hemangiomas the skin. This is the most tolerable form of therapy for the patient. Hemangiomas in the brain may be in areas that cannot be operated on. Here is one Irradiation the means of choice. This also shows good results. In addition to all of these more invasive therapy options, there is now one drug treatment with corticosteroids or beta blockers, so proven to be just as effective.
Can a hemangioma also be lasered?
Hemangiomas can also be treated with laser therapy. Since a laser has a penetration depth of less than one centimeter, the children should be introduced early. In some cases, multiple treatments are required. Since laser treatment is painful, local anesthesia can be performed before treatment. After the laser treatment, the skin turns dark, but this disappears after a few weeks.
Who pays for the removal?
If removal of the hemangioma is necessary in childhood, these costs will be covered by the Health insurance carried. The same applies to hemangiomas in adults as soon as they become symptomatic and mean functional limitations for the patient. If there is a desire for distance aesthetic reasons the cost is usually not borne by the health insurance. In most cases this is a Laser therapythat depending on the size between 50 € and 150 € costs.
Treatment in babies with propanolol
In the meantime, drug therapy for hemangiomas with beta blockers has also become established. The beta blocker propranolol is mainly used here. These types of active ingredients are heart medication in the original sense of the word, to relieve the heart and counteract any cardiac insufficiency. They are mainly used for deep hemangiomas of the skin, which would leave larger scars if treated with a standard laser procedure. Propranolol is a non-selective beta blocker. Propranolol has been officially approved for the treatment of hemangiomas in babies and young children since 2014. The drug can be taken up by mouth or applied as an ointment. Propranolol is used especially for hemangiomas in critical areas such as the eyes or mucous membranes. Treatment usually lasts about half a year.
Taking into account the actual effect, propranolol is only given in small doses and an EKG and an ultrasound of the heart are carried out before therapy in order to be able to assess any complications. The duration of the therapy is usually about six months and shows very few side effects, especially when compared to drug therapy with corticosteroids. In most cases it is taken by dissolving the powder in water. In addition, gels that contain the active ingredient and are applied directly to the affected area have also become established.