Hemolytic anemia
Note
You are in a sub-topic of the anemia section.
General information on the topic can be found at: Anemia
introduction
Hemolysis is the dissolution of red blood cells. This happens naturally after a red blood cell has a lifespan of 120 days.
An increased and premature breakdown is pathological and leads to anemia if the breakdown rate is higher than the new formation rate, which can be increased to compensate.

Symptoms
In addition to the general signs of anemia, those affected suffer from yellowing of the skin and the conjunctiva of the eye (jaundice).
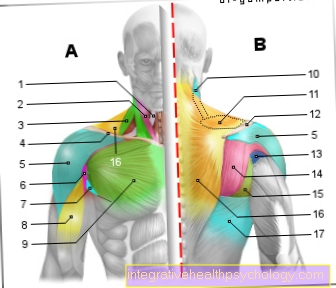
Normally, the breakdown of old red blood cells takes place in the spleen. Therefore, prolonged degradation can lead to an enlargement of the spleen (Splenomegaly).
A hemolytic crisis can occur with severe infections or surgery. The crisis is characterized by massive yellowing of the skin, fever and pain.
Causes and forms
The causes of hemolytic anemia are:
- Defects in the membrane structure of the red blood cells (e.g. spheroidal cell anemia (Hereditary Spherocytosis), Elliptocytosis, Marchiafava anemia)
- Disturbed metabolism in the cells (enzyme defects such as glucose-6-phosphate dehydrogenase deficiency, pyruvate kinase deficiency)
- Disturbances in the hemoglobin structure (e.g. sickle cell anemia)
- Poisoning, drugs, chemicals, radiation, etc.
- Autoimmune antibodies
- Antibodies that are active at certain body temperatures
- Antibodies after incorrect transfusion
- As a result of bone marrow transplant
Antibody-induced hemolysis
In antibody-induced hemolysis, the body produces antibodies which are directed against the red blood cells and lead to their destruction. This antibody formation can be brought about by drugs or infections. Often these are heat autoantibodies. These bind to the red blood cells at body temperature and then lead to their destruction in the spleen or liver. The heat autoantibodies can be detected with the so-called Coombs test. Corticosteroids are used in therapy.
These drugs can cause hemolytic anemia
Taking some drugs stimulates the formation of antibodies that are directed against red blood cells. There are several drugs that can cause hemolytic anemia as a result. However, the drugs rarely induce hemolytic anemia.
Medicines include non-steroidal anti-inflammatory drugs (NSAIDs). This group of drugs includes various pain relievers such as Ibuprofen. Certain antibiotics can also lead to haemolytic anemia in rare cases. These include penicillins and cephalosporins. Another drug is alpha-methyldopa, which is used to treat high blood pressure in pregnant women.
Cold antibodies
Cold antibodies are antibodies formed by the body, which bind to red blood cells at low temperatures and lead to their death.
A distinction is made between the acute cold agglutinin syndrome, which usually occurs 2-3 weeks after an infection, and a chronic form. This can occur with a lymphoma or without an apparent cause. In this case, you should protect yourself from the cold. In the case of pronounced hemolytic anemia, immunosuppressants can also be taken - i.e. drugs that suppress the immune system.
Mechanically induced hemolysis
In mechanically induced hemolysis, the red blood cells are mechanically destroyed by external influences. This can be done through an artificial heart valve or with hemodialysis, when the blood is passed through the dialysis machine for cleaning.
What does the diagnosis look like?
As always, the diagnosis begins with a detailed doctor-patient discussion followed by a physical examination.
A blood test is essential to diagnose anemia. Here, as in all anemias, the hemoglobin is initially reduced. Additional parameters are also collected. By destroying the red blood cells, the LDH (lactate dehydrogenase) increases. Lactate dehydrogenase is an enzyme that is found in the red blood cells and can be measured in increased amounts in the blood due to the loss of these. Serum iron is also increased.
In addition, the haptoglobin is measured. The haptoglobin binds the released hemoglobin until this complex is broken down by the spleen and liver. Furthermore, the indirect bilirubin is increased. This is a breakdown product of hemoglobin. Depending on the suspected cause, further specific examinations are carried out.
Change in blood parameters
Hemolytic anemia is shown by the following blood parameters:
- Haptoglobin decreased
- indirect bilirubin increased
- LDH increased
- free hemoglobin increased
- increased urobilinogen in the urine
- Reticulocytosis (an increase in the number of young red blood cells)
- Enlargement of the blood-forming bone marrow
- Depending on the type of anemia: changed shape of the cells (sphere, ellipse, sickle-shaped)
Life expectancy
It is not possible to make a general statement about life expectancy in the case of haemolytic anemia. Life expectancy depends on the cause of the anemia. If these causes are curable, life expectancy is not restricted.
On the one hand, there are various congenital defects in the red blood cells that lead to hemolytic anemia. Depending on the severity of the defect and the treatment options, the courses are very different and in the worst case can be fatal. The anemia can also be caused by physical and chemical damage or medication. If the therapy is successful and the cause has been eliminated, life expectancy is not affected. Antibody-related hemolysis also usually has a very good prognosis.
In addition, there are rare microangiopathies (diseases of the small blood vessels) which, in addition to other symptoms, also cause anemia. An early start of treatment is crucial for a good prognosis. It looks similar if the cause of an infectious disease, such as Malaria, lies. The general physical condition and the age of the sick person also play an important role. An acute and rapid development of hemolytic anemia can result in a life-threatening emergency situation. One speaks of a hemolytic crisis.













.jpg)