Urinary tract infection
definition
The urinary tract infection in the narrower sense describes what is popularly known as cystitis. The technical term for this is Cystitis. However, urinary tract infections can actually - as the name suggests - affect the entire urinary system. A distinction is therefore made between the upper and lower urinary tract infections.
While cystitis and urethritis are referred to as lower urinary tract infections, upper urinary tract infections include involvement of the ureters and / or kidneys (Pelvic inflammation) with a.
Cystitis is a very common condition that occurs more frequently in women.Kidney inflammation can result from untreated cystitis. Also the Urosepsis arises from an untreated cystitis and is potentially life-threatening. Nevertheless, cystitis does not always have to be treated with medication.

causes
A urinary tract infection results from an infection. An infection, in turn, occurs when the body or part of the body is colonized with bacteria. In all types of urinary tract infections, including cystitis, bacteria that ascend into the bladder via the urethra are the most common cause of infection.
An upper urinary tract infection can develop from an untreated lower urinary tract infection. The bacteria rise from the bladder further into the urinary system and thus get into the ureters (urethra) or even down to the kidneys. While a simple cystitis is often a harmless clinical picture, the upper urinary tract infection can lead to an inflammation of the kidney pelvis, which is accompanied by severe general symptoms.
A urinary tract infection can also develop into what is known as urosepsis. With sepsis, the bacteria get into the blood and this leads to a kind of infection of the whole body. Sepsis is a life-threatening condition that urgently needs treatment.
Read more about this under Urosepsis
There are risk factors that favor the occurrence of a urinary tract infection. These include malformations in the urinary system as they most often occur in young boys, an enlargement of the prostate (Prostatic hyperplasia) as it occurs in older men, urinary stones, improper intimate hygiene, urinary catheters, diabetes mellitus and women. The fact that women are considered a risk factor for developing a urinary tract infection is due to the fact that a woman's urethra is significantly shorter than that of a man. This makes it much easier for bacteria to get into the bladder from the outside. Cold, or cold feet, can also promote cystitis. Read more about this: Cystitis from cold feet
E. Coli
Escherichia coli (abbreviated E. Coli) is a gram negative bacterium. It occurs mainly in the intestinal flora, i.e. in the gastrointestinal tract. In healthy patients who live at home, the most common cause of E. coli-induced urinary tract infections is improper intimate hygiene. This allows bacteria from the anus area to move forward into the urinary tract and then ascend into the bladder. This usually happens much more frequently in women than in men because the urethra in women is significantly shorter.
E. coli is the most common cause of urinary tract infections acquired in the home (community-acquired urinary tract infections). E. coli is the detected bacterium in around 70% of these community-acquired urinary tract infections. Bacteria from the group of enterobacteria are less common. For example Klebsiella or Proteus species. Staphylococci and enterococci also occur. Urinary tract infections that were acquired during a stay in a care facility (e.g. hospital) are referred to as nosocomial urinary tract infections. The most common pathogens here are Klebsiella, Proteus and Pseudomonas aeruginosa. But E. coli is also common.
Through sexual intercourse (GV)
There are germs that are transmitted through sexual contact and can trigger a lower urinary tract infection. This includes above all Neisseria gonnorhoeae, Trigger of gonorrhea (gonorrhea), and Chlamydia trachomatis.
Read more about this under
- Chlamydial infection
- gonorrhea
Infection with one of these pathogens often leads to an isolated inflammation of the urethra (Urethritis). However, there are also many women who develop cystitis a few days after intercourse. This type of cystitis even has its own name, the so-called Honeymoon cystitis (Honeymoon cystitis). This type of cystitis is particularly common when a new sexual partner is found. Everyone has a slightly different intestinal flora. During sexual intercourse, germs from the intestinal flora can get into the vaginal area of women. Especially when women are not yet "used" to the man's intestinal flora, cystitis is not uncommon. In some cases, honeymoon cystitis can be prevented by a relatively simple measure: Carefully washing the genital area before and immediately after intercourse. The man should wash himself before intercourse in order to reduce the woman's risk of cystitis. In general - especially with sensitive women - vaginal intercourse immediately following anal intercourse should be avoided, as this carries a relatively high risk of developing a bladder infection.
Through a urinary catheter
A urinary catheter is a thin, flexible tube that is pushed from the outside through the urethra into the urinary bladder. The purpose of the catheter is to drain urine from the bladder to the outside. This can be useful, for example, in patients with neurological disorders that affect urination, in old incontinent patients, or in the context of an operation with subsequent immobility.
Even if the urinary catheter is placed under sterile measures, it is a potential source of infection. Bacteria can rise from the outside through the tube in the urethra into the bladder and cause inflammation. Urinary catheters should therefore only be left in place for as long as is absolutely necessary. The longer the catheter is in place, the higher the risk of infection.
An alternative for patients who need a urinary catheter permanently is the so-called suprapubic bladder catheters. It is not introduced into the bladder through the urethra but through an incision above the pubic bone. The risk of infection with this type of catheter is lower. In addition, adequate hygiene of the urinary catheters in place and the patient's genital area should be carried out daily in order to minimize the risk of infection.
Urinary catheters are the most common cause of urinary tract infections in hospitals (nosocomial urinary tract infections). Even if such a urinary tract infection sounds like a rather banal disease at first, it should not be underestimated. Such an infection can develop into life-threatening urosepsis - especially in patients with serious previous illnesses or a weakened immune system.
Concomitant symptoms
Symptoms that can accompany a urinary tract infection are varied, depending on which part of the urinary system is affected by the infection.
If the urethra itself is infected, this can manifest itself as a strong burning sensation when urinating and itching in the area of the urethra.
Even with a bladder infection, urination is often accompanied by a very painful stinging.
The amount of urine per toilet is small, but there is a constant urge to urinate, one speaks of one Pollakiuria. Blood can be found in the urine (Hematuria) come.
If the infection has risen to the kidneys, it is an inflammation of the kidney pelvis (Pyelonephritis). This is often associated with a greatly reduced general condition, high fever and chills. The affected kidney length is pounding. Nausea and vomiting can also occur with inflammation of the kidney pelvis.
Read more about this under Pelvic inflammation
With Pain
Pain is a fairly common symptom of a urinary tract infection. If the bladder or urethra is affected by the inflammation, the pain occurs mainly as a sharp stinging and burning sensation each time you urinate. With inflammation of the kidney pelvis, dull pain in the area of the affected kidney bed and severe knocking pain in the kidney bed can occur.
Without pain
A urinary tract infection is typically associated with pain. With classic cystitis, pain occurs when urinating, with kidney inflammation regardless of this. However, there are also patients who do not feel pain when they have a urinary tract infection. Old and confused people in particular can have pain, but cannot express it adequately. This makes the diagnosis more difficult.
fever
Fever is a typical symptom of an upper urinary tract infection, an infection that particularly includes one of the two kidneys. The pelvic inflammation (Pyelonephritis) is a serious clinical picture that can be accompanied by a high fever of over 40 ° C, chills and a greatly reduced general condition. Antipyretic agents and antibiotics should be used here.
itching
Itching is a symptom that is particularly common with isolated inflammation of the urethra (Urethritis) occurs. The itching is then localized in the area of the urethra. Accompanying this may be a painful stinging and burning sensation when urinating.
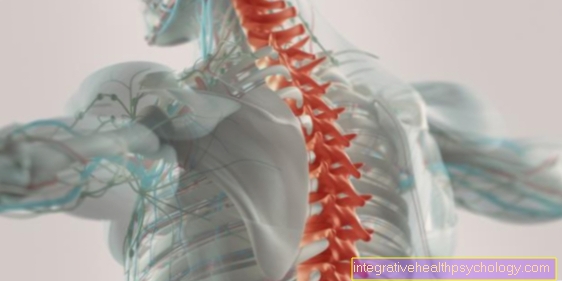
Back pain
Back pain occurs mainly as part of an upper urinary tract infection. Although the pain feels like it is localized in the back, most of the time it is pain in one of the two renal pelvis.
If the kidney is infected, it can swell. The kidney itself is not sensitive to pain. However, when it swells, the capsule surrounding the kidney becomes under tension. The capsule is equipped with pain-sensitive stretch sensors. An inflammation-related enlargement of the kidney can lead to flank pain. One speaks of a pain in the kidney capsule.
Read more about this under Differentiation from kidney pain to back pain
nausea
Nausea and vomiting are also symptoms that can occur, especially with inflammation of the kidney pelvis. With uncomplicated cystitis, they are rather rare. In the case of inflammation of the renal pelvis, there is also a severe impairment of the general condition with chills, fever and pain.
Blood in the urine
Blood in the urine is known in technical jargon as Hematuria designated. Macrohematuria refers to the amount of blood that can be seen in the urine with the naked eye. A Microhematuria means evidence of blood in the laboratory or by means of a strip test without the blood being visible to the naked eye.
One of the most common causes of blood in the urine is kidney stones. However, urinary tract infections can also be accompanied by blood in the urine. A cystitis with blood in the urine is also called hemorrhagic cystitis designated.
After the infection has healed, no more blood can be detected in the urine. The detection of blood in the urine is carried out either by visual diagnosis or by urine examination via laboratory test or urine strip test.
Read more on this topic on the main page Blood in the urine
discharge
Discharge is not a typical symptom of cystitis. Discharge rarely occurs even if a kidney is inflamed.
In isolated inflammation of the urethra (Urethritis) however, in addition to burning sensation when urinating and itching, there is often a discharge from the urethra.
stomach pain
In the context of a bladder infection, burning pains in the lower abdomen when urinating and frequent urination occur. Pain in the lower abdomen at rest (regardless of urination) can also occur as part of a cystitis. In otherwise healthy patients, the symptoms often completely disappear after a few days, even if left untreated.
diagnosis
The diagnosis of a urinary tract infection consists of several components.
First, the anamnesis should be done. The doctor asks about the symptoms, how long they have existed, whether there has ever been a urinary tract infection, whether there are previous illnesses and whether medication is taken regularly. It is also important to know whether the urinary tract infection was acquired at home or in a care facility (hospital, nursing home).
This is followed by the physical exam with a focus on examining the lower abdomen and kidney region. For example, the doctor will knock his fist loosely on both kidney beds to check whether there is any pain. Depending on how old and how morbid the patient is, a blood sample can also be taken. In young healthy women, the most common group of patients with simple urinary tract infections, there is no need to take additional blood. In older, previously ill patients, a blood sample can be useful. Blood is usually drawn even in patients with knocking pain in the kidneys.
The decisive criterion for deciding whether there is a bladder infection or not is a urine test, the so-called Urine status. This is explained in more detail in the next section. In addition to the diagnostic measures mentioned above, an ultrasound scan may also be used to assess the urinary bladder and kidneys and to rule out urinary congestion.
With a quick and easy self-test at home, you can determine an initial suspicion of a cystitis yourself. More information is available at: Rapid test for a cystitis
Which doctor treats the urinary tract infection?
A urinary tract infection is usually treated by the family doctor. They have a wide range of diseases that they can treat. In most cases in the hospital, the internists, i.e. the doctors for internal diseases, are responsible for treating urinary tract infections. In hospitals where there is a urology department, this department can also treat urinary tract infections.
What is the urine status?
The urine status is a laboratory test to clarify various diseases.
The urine to be examined should ideally be midstream urine. This means that when going to the toilet some urine is left first, only the urine from the middle phase of urination is then collected. The urine is now either given to the laboratory and examined there or a quick test is made with a test strip.
The urine is tested for the presence of red blood cells (blood in urine = Hematuria), white blood cells (Leukocyturia), Nitrite, protein, sugar and other components were examined.
An increased number of white blood cells in the urine is essential for the diagnosis of a urinary tract infection. Often nitrite is also present as many bacteria such as E. coli produce nitrite. However, a lack of evidence of nitrite does not rule out the presence of a urinary tract infection. In addition to diagnosing urinary tract infections, the urine status is also used for diagnosing other kidney diseases as well as diabetes mellitus and, more rarely, pheochromocytoma and liver diseases.
Read more about this under Urinalysis
What do you think of test strips?
As a rule, hospitals always have the option of having urine tests precisely evaluated by a laboratory. If an acute laboratory is not available, as is the case in a doctor's office, for example, urine test strips are used as an alternative. It is a strip of plastic on which different colored zones can be seen. These zones check the presence of certain substances in the urine. A normal urine test strip tests for the presence of red blood cells (Erythrocytes), white blood cells (Leukocytes), Nitrite, sugar (glucose), Egg white (protein), Ketones, pH and urobilinogen.
Each zone contains an indicator which changes color when it comes into contact with the substance to be tested. The more of the substance to be tested is present, the stronger the color change. The urine test strip is briefly held in the container with the midstream urine to be checked and can then be read immediately. An attached reference scale, which provides explanations for the different color changes, serves as an aid.
The urine test strip is a helpful tool for an initial diagnosis. It provides rough indications of the possible presence of certain diseases. However, the strip test cannot make any precise statements about the amount of the substances to be tested. The intensity of the color change only shows a rough estimate of the amount. A more detailed urine test in the laboratory is then necessary to obtain more precise information. Urine test strips are used in practice (general practitioners, gynecologists, paediatricians) and can also be used by the patient as a self-test. They are a very helpful primary diagnostic tool for the above measures and can be supplemented with further tests if necessary.
What is the therapy like?
The therapy of a urinary tract infection depends on its precise localization.
An inflammation of the urethra (Urethritis) is treated with antibiotics in most cases. The choice of antibiotic depends on which pathogen is most likely to be the trigger.When it comes to cystitis, a decision is made between an uncomplicated and a complicated urinary tract infection.
An uncomplicated cystitis, which occurs relatively often in healthy women, can in principle also occur without drug therapy. In these cases, pain therapy over a few days, for example with ibuprofen, is usually the best way to treat the pain. Antibiotic therapy for uncomplicated bladder infections is also possible. Various antibiotics are available here. For example, fosfomycin, which only has to be taken once, as well as nitrofurantoin, which has to be taken over 5 days, or antibiotics from the group of fluoroquinolines such as ciprofloxacin, which must be taken over 3 days.
A complicated urinary tract infection, as it is defined, for example, in men, should generally be treated with antibiotics with one of the substances mentioned above.
There is also the clinical picture of asymptomatic bacteriuria. In this case, leukocytes are increasingly found in the urine status so that there is a formal cystitis. Those affected have no complaints whatsoever. Such asymptomatic bacteriuria usually does not require antibiotic treatment. Exceptions to this are pregnant women, who should also be given antibiotic therapy in this case.
Read more about this under Bacteria in the urine - how dangerous is it?
Another important clinical picture in the area of urinary tract infections is pelvic inflammation. In any case, this must be treated with antibiotics. Fluoroquinolones such as ciprofloxacin or the active ingredient cefpodoxime from the group of cephalosporins are used as agents of choice. Co-trimoxazole or amoxicillin can also be used. Antibiotic therapy should take place over 7-10 days. In the case of kidney inflammation, antipyretic drugs such as paracetamol or metamizole are often necessary at the beginning. In the case of kidney inflammation, it is important to take care of yourself.
When do i need an antibiotic?
An antibiotic is not always necessary for a urinary tract infection. In the case of uncomplicated cystitis, the treatment can also be carried out without antibiotics. The same is true of asymptomatic bacteriuria.
Antibiotic treatment should always be used for a complicated urinary tract infection and inflammation of the kidney pelvis (Pyelonephritis) respectively. Pregnant women should also always receive antibiotic therapy.
Read more about this under Antibiotics in Pregnancy
Otherwise, the patient's level of suffering is decisive when deciding whether or not antibiotic treatment of uncomplicated cystitis is necessary. It is not uncommon for pain relievers such as ibuprofen to help here for 2-3 days.
Ciprofloxacin
Ciprofloxacin is a fluoroquinolone antibiotic. It is used to treat numerous diseases. For a long time it was the most commonly prescribed drug for bladder infections. In the current guidelines, however, it is only a second choice or alternative solution if there is an intolerance to the first choice. These first-line agents include fosfomycin and nitrofurantoin. In the treatment of pelvic inflammation, however, ciprofloxacin is still the first choice.
Which drugs besides antibiotics are used?
The drug treatment of urinary tract infections is primarily done with antibiotics. In addition, drugs for pain relief, such as ibuprofen, can be used.
homeopathy
Various homeopathic remedies are available for treating the symptoms of cystitis.
Used to treat the pain that occurs Cantharis vesicatoria (Spanish fly) recommended. It is said to help relieve the burning sensation in the bladder and urethra area when urinating. It is recommended to take 3 globules every 30 minutes for use.
If the pain is very severe, the application of Mercurius corrosivus (Mercury chloride) recommended. Here, too, 3 globules can be taken every half hour. Also Equisetum hiemale (Winter horsetail) is used to treat pain associated with a bladder infection. Other possible homeopathic remedies for pain management are Terebinthina (Turpentine), Apis mellifica (Honey bee) and Pareira gooda (groundwort). Of all these remedies, 3 globules can be taken every 30 minutes. Also used Colibacillinum (Anti-Colibacillary Serum) that can be taken four to six times a day. Furthermore you can Formica rufa (red wood ant), Rhus toxocodendron (Poison oak), sepia (Octopus), Belladonna (Deadly nightshade), Aconitum napellus (Monkshood), Mercurius solubilis (Mercury) and Lycopodium clavatum (Bärlappe) for the symptomatic treatment of a urinary tract infection are used. The selection of homeopathic remedies is large so that in the event of acute complaints, it is best to ask a homeopath which remedy is best.
It is important, however, that homeopathic drugs do not cure the disease, only relieve the symptoms. A doctor should therefore be consulted promptly in the case of urinary tract infections with fever, chills and worsening of the general condition and in the case of urinary tract infections during pregnancy, homeopathic remedies are not sufficient for adequate treatment.
tea
During a urinary tract infection, especially during classic cystitis, it is extremely important to drink a lot so that the bacteria are flushed out of the urinary tract. Whether tea or water is drunk here is irrelevant. It is important to drink more than 2 liters per day provided there are no diseases that prohibit this.
There are also numerous suppliers of so-called bladder-and-kidney teas. In the end, these teas don't do much else than other liquids: they flush the kidney and urinary tract. The package insert states that they are used to increase the amount of urine and to prevent urine gravel and urinary stone formation. The ingredients are said to have a diuretic and slightly anti-inflammatory effect. Bladder and kidney teas are not much more expensive than normal teas from some suppliers. Such teas can definitely be used by people who like to drink tea and have a urinary tract infection. However, an advantage over drinking sufficient amounts of other teas or liquids has not yet been proven with certainty.
Read more about this under Indian kidney and bladder tea
cranberry
Cranberry becomes German as large-fruited cranberries or Cranberry designated. However, the English term cranberry is also much more common in Germany. Cranberry is best known as a traditional cure for bladder infections. However, there is no clear scientific evidence of the effectiveness of cranberries in the treatment of urinary tract infections. Nonetheless, cranberry can be used to prevent urinary tract infections. Cranberry prophylaxis can be attempted especially in people (mostly women) who are prone to frequent bladder infections. Cranberry comes in pill, capsule, and juice form. The preparations are available in pharmacies and drugstores without a prescription. 500 ml of cranberry juice cost 5-6 euros. For the prophylaxis of urinary tract infections, about 50 ml of juice should be consumed daily.
Also read the article: The cranberry capsules.
When do I have to go to the hospital?
Inpatient hospital treatment is rarely necessary if a urinary tract infection is present. However, inpatient therapy may be necessary for babies and toddlers with urinary tract infections who are in poor general condition.
Kidney inflammation is a serious clinical picture that may also have to be treated as an inpatient. In otherwise healthy patients, antibiotic and antipyretic outpatient therapy is usually also possible. Especially with old and previously ill patients, a Pyelonephritis make inpatient treatment necessary.
In patients who have developed urosepsis from a urinary tract infection, i.e. who have bacteria spread into the blood, hospital treatment with intravenous antibiotic therapy is often necessary. It may happen that these patients need close care in the intensive care unit. In general, however, a simple cystitis, no matter if uncomplicated or complicated, does not have to be treated in hospital for otherwise physically fit people.
Duration
An uncomplicated cystitis lasts a few days to a week. The pain is particularly pronounced in the first 3-4 days. They usually go back a little faster under antibiotic therapy, i.e. without therapy.
Complicated urinary tract infections, which should always be treated with antibiotics, do not necessarily last less long due to the antibiotic treatment, but the symptoms may decrease sooner. If antibiotic therapy is started quickly, a clear reduction in symptoms can be expected after about 1-2 days.
Kidney inflammation is a serious disease that lasts for 1-2 weeks in most cases. Antibiotic treatment should be started as soon as possible. The symptoms then usually go away slowly within 3-5 days. However, the intake of fever-lowering agents and painkillers already leads to a control of the symptoms by the onset of the antibiotic effect.
How contagious is a urethral infection?
A urethral infection or inflammation of the urethra (Urethritis) is a disease that is often transmitted through sexual contact. So it is highly contagious.
A distinction is made between gonorrheic and non-gonorrheic urethritis.
The gonorrheic form is caused by infection with the bacterium Neisseria gonorrhoeae triggered. This condition is better known as gonorrhea. It is one of the most common sexually transmitted diseases. Transmission can take place directly via the genital area but also via the oral or anal mucosa during oral or anal intercourse. An infection of the eyes is also possible. Gonorrhea is a highly contagious disease. The use of condoms can significantly reduce the infection rate, but if used improperly there is still a risk of infection from smear infection.
In addition to gonorrheic urethritis, there is also non-gonorrheic urethritis. It is most commonly caused by chlamydia. The incidence of this type of urethritis is significantly higher than that of gonorrhea (gonorrhea). The infection occurs through unprotected sexual intercourse. In antibiotic treatment after infection, the sexual partner must usually also be treated, otherwise mutual infection is always possible.
What is the transmission route for a urinary tract infection?
Except for urethritis, urinary tract infections cannot be transmitted from one person to another. Cystitis is caused by bacteria that get into the bladder through the urethra. If the bacteria continue to rise, they can trigger inflammation of the kidney pelvis.
Can you have a urinary tract infection without bacteria?
In the vast majority of cases, urinary tract infections are caused by bacteria. In extremely rare cases, viruses, fungi or parasites can irritate the bladder mucosa and thus lead to inflammation.
How can you prevent urinary tract infections?
Women in particular tend to keep developing bladder infections. Hence, it is crucial to take preventive measures.
Non-drug measures include sufficient fluid intake of at least 2 liters per day, complete emptying of the bladder when using the toilet and warm clothing.
Correct intimate hygiene is also very important. After a bowel movement, you should always wipe from front to back; when washing with a cloth, the vagina should always be cleaned first and then the anal area. Otherwise there is a risk of introducing bacteria from the intestinal tract into the urinary tract. These bacteria can then cause a urinary tract infection.
During sexual intercourse, care should be taken not to immediately follow anal intercourse with vaginal intercourse. Women should empty their bladders and wash themselves after intercourse. Drug prophylaxis can be attempted in patients in whom the bladder infection occurs primarily after sexual intercourse. The antibiotic is used once after intercourse Trimethoprim taken. The quality of the effectiveness is not sufficiently proven with studies.
One also often hears that the regular intake of cranberry supplements should protect against recurrent urinary tract infections. Women who suffer from urinary tract infections more often can give this a try. So far, however, there are no recommendations in the guidelines.
There is also a type of vaccine that is supposed to reduce the body's sensitivity to certain bacteria. For example, there are capsules that contain killed Escherichia coli pathogens. One tablet should be taken daily for 3 months. A vaccination against cystitis is also available in syringe form. It contains inactivated bacterial pathogens. Three vaccinations should be given every two weeks. A booster vaccination should be given after about a year. The effectiveness of the vaccination has not yet been sufficiently proven.
Can I be vaccinated against a urinary tract infection?
Yes, there is the possibility of vaccination against recurring (recurrent) Urinary tract infections. There are different types of vaccination. A vaccine is given in the form of syringes. It contains inactivated bacteria. These bacteria are those that typically trigger a urinary tract infection. The aim is to present the pathogens to the body in a weakened form so that the immune system can develop an adequate defense against these pathogens and can then kill them effectively in the event of a urinary tract infection. The basic vaccination consists of 3 syringes which have to be given every 2 weeks. This basic immunization should ensure that the body is immune to the relevant bacteria for about 1 year. A booster vaccination must be given after one year.
There is also a vaccination in tablet form. The tablets contain inactivated Escherichia coli pathogens. One tablet must be taken daily for the first three months, after which the primary vaccination course is complete. Then the refreshment takes place in month 7-9. Here, 1 tablet per day must be taken 3 times over 10 days. The interval between the 10 days must be 20 days. So far, the benefits of the vaccinations mentioned for the prevention of urinary tract infections have not been sufficiently proven.
L-methionine
L-methionine is an essential amino acid. There is evidence in the literature that acidifying the urine (e.g. with methionine) is helpful in preventing recurrent urinary tract infections. This has to do with the fact that bacteria grow less well in an acidic / acidified environment. If the urine is now acidified with the help of methionine, this should create more difficult conditions for the bacteria and their growth. So far, there is no sufficient evidence of the effectiveness of methionine so that there is no recommendation for it to be taken.
particularities
Special features in women
Urinary tract infections are relatively common in women. The reason is the short way from the outside via the urethra to the bladder. Not all urinary tract infections in women require antibiotic treatment. In some cases, pain therapy for a few days is sufficient. However, women during pregnancy should always be treated with antibiotics.
In women who frequently suffer from urinary tract infections (recurrent urinary tract infections) prophylactic therapy can be used. This can be done independently with herbal remedies. This includes, for example, cranberries in the form of juice or tablets. Medicinal preventive measures can be discussed with the attending physician.
Read about this too
- Home remedies for cystitis
- Homeopathy for cystitis
In early pregnancy / pregnancy
Middle-aged women are much more likely to develop bladder infections than men. The rate of urinary tract infections increases again during pregnancy. They occur about 4-7% of the time. Such an infection during pregnancy is always considered to be complicated, so it should always be treated with antibiotics.
As is the case with non-pregnant women, the urine test is of the greatest diagnostic importance. A urine culture should also be performed. The exact pathogens are determined and it is evaluated which antibiotics are most effective against these pathogens. During pregnancy you also need a asymptomatic bacteriuria, i.e. a urinary tract infection that only shows itself through the urine values but does not cause any symptoms, can be treated. The reason for this is the assumption that urinary tract infections cause an increased rate of premature births during pregnancy. In addition, if left untreated, there is a risk that the urinary tract infection will develop into kidney inflammation.
Only certain antibiotics can be used to treat urinary tract infections during pregnancy. These include, for example, drugs from the group of Cephalosporins and Amoxicillin. Fosfomycin is recommended as first choice by some authors, and only as second choice by others. The recommendations for the duration of therapy vary; the guideline recommends a therapy duration of 7 days. Kidney inflammation should be treated with cephalosporins. Due to the severity of the clinical picture, inpatient therapy should be considered.
Read more about this under Cystitis During Pregnancy
In the puerperium
A urinary tract infection can also occur during the puerperium. As in pregnancy, it occurs more frequently here than in non-pregnant women. Symptoms include burning pain when urinating and an increased need to urinate. A urine test must be done for diagnosis. In the presence of a urinary tract infection, increased white blood cells can be detected in the urine, one speaks of one Leukocyturia. Antibiotic treatment is usually sought. However, this must be decided by the treating gynecologist on a case-by-case basis.
Read more about this under Bed sicknesses
What should I watch out for while breastfeeding?
A urinary tract infection that occurs during breastfeeding is ultimately nothing more than a urinary tract infection during pregnancy. The main difference is that an infection must always be treated with antibiotics during pregnancy. During breastfeeding, it can be decided individually whether antibiotic treatment is necessary. There are special antibiotics that can be safely used during pregnancy and breastfeeding. These include, for example, the cephalosporins.
Read also on this topic Antibiotics in Pregnancy
Urinary tract infection in the baby
Babies can also develop a urinary tract infection. Diagnosis is much more difficult, especially in infancy.
If the child has symptoms such as fever, vomiting, increased tiredness or excessive crying and irritability, loss of appetite, or abnormalities in the urine (blood in the urine, foul-smelling urine), this could be a sign of a urinary tract infection.
However, other diseases are also possible. In any case, the treating pediatrician should be consulted, who can take further diagnostic measures. The doctor needs a urine sample to make a diagnosis. This is of course difficult to implement, especially with babies who have not yet been put on the pot. The doctor will give the parents a urine bag that must be glued on. If the diagnosis of a urinary tract infection is confirmed, antibiotic treatment is usually started.
For very young children there are antibiotics in liquid form. If the child is in poor general condition, does not drink anything, or has a very high fever, hospitalization with intravenous infusion therapy may be necessary. Urinary tract infections are always considered complicated in children up to 2 years of age. They need rapid antibiotic treatment.
Read more on the subject at: Urinary tract infection in the baby
Urinary tract infection in the child
Urinary tract infections can occur at any age. In addition, at any age there is also the risk that if left untreated, inflammation will advance to the kidneys with the development of dangerous pelvic inflammation.
In slightly older children, the diagnosis may be a little easier, for example if the children complain that they have burning pain when urinating and often have to go to the toilet. However, non-specific symptoms such as abdominal pain can also occur.
As in adults, the diagnosis is made by examining the urine. The urine of toddlers can be obtained from the pot, slightly older children may even be able to put water into a cup provided for this purpose with support. If there is a urinary tract infection, antibiotic treatment is usually initiated in children. In addition to drug therapy, it is important that the children drink a lot in order to flush the urinary tract sufficiently.
Read more on the subject at: Urinary tract infections in children - it's that dangerous!
Particularities in men
The man has a longer urethra than the woman because it runs through the penis. The way from the outside through the urethra to the bladder is longer than with women. Therefore, urinary tract infections are less common in men. Since urinary tract infections occur rarely in men, a urinary tract infection in men is always considered to be complicated. He should always be treated with antibiotics. The drugs of choice are fosfomycin or nitrofurantoin. Older men often have an enlarged prostate (Prostatic hyperplasia). This can narrow the urethra and lead to a problem with the flow of urine. Therefore, older men are more likely to have urinary tract infections.
Read more about this under Enlarged prostate and vas deferens swollen - what's behind it?















.jpg)







-mit-ten-(titanic-elastic-nail)-oder-sten.jpg)
