Neck Abscess - Is It Dangerous?
definition
An abscess on the neck (neck abscess) is an encapsulated collection of pus in the area of the neck. In most cases, the location is in the side of the neck, sometimes in the neck area, rarely in the front area.

Is a Neck Abscess Dangerous?
A neck abscess is an encapsulated collection of pus. As long as the pus is enclosed in this capsule, it does not represent an acute danger. Only the pressure exerted by the abscess on surrounding structures, such as the cervical vessels and nerves, can be dangerous under certain circumstances.
However, if the abscess bursts and the pus and the associated pathogens reach the throat area, severe local inflammation can develop. In the worst case, the pathogen passes into the bloodstream and "blood poisoning" occurs (Sepsis).
A neck abscess should therefore always be clarified and, if necessary, surgically removed.
Is a Neck Abscess Contagious?
The neck abscess in itself is not contagious. But the pathogens that caused it can be contagious. Often it is the staphylococcus aureus. It is transmitted via droplet infection. Therefore, data subjects should protect their fellow human beings by carefully implementing appropriate security measures. These include, for example, adequate hand hygiene, avoiding shaking hands, keeping your distance from other people and not sharing glasses, cutlery or towels with anyone else.
Causes and forms of the neck abscess
In most cases, a neck abscess is caused by an infection of
- Viruses,
- Bacteria or fungi.
In the statistically most frequent cases of a neck abscess, it is bacteria and, as a rule, bacteria of the Staph aureus strain that lead to abscess formation.
The germ naturally colonizes large parts of the skin. It is not known how an infection with this germ can occur. As a rule, the bacterium is washed into the bloodstream.
Once it has entered the body, it can trigger an infection at any imaginable place, but it can also settle down and become increasingly isolated. In this case the first course for abscess formation has already been set. Soft tissue infections in the neck area can also lead to a neck abscess. Sometimes enlarged and infected lymph nodes can also promote the progression of abscess formation.
Enlarged lymph nodes in a neck abscess
With a neck abscess, the lymph nodes on the neck can be enlarged. It is also possible that enlarged lymph nodes on the neck encourage the development of an abscess. Usually the lymph nodes along the head turner muscle are swollen. The lymph nodes can be painful to touch / pressure.
Also read:
- Lymph node swelling on the neck - how dangerous is it?
- Lymph nodes are swollen - how dangerous is it?
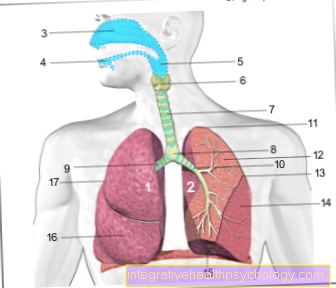
Neck abscess from tonsillitis
A complication in the context of a purulent tonsillitis is the development of a neck abscess. This is an abscess called a peritonsillar abscess. This neck abscess is located in the area of the palatal arches and the pharynx wall. Signs are often severe pain when swallowing, which radiates into the ear. In addition, bad breath, high fever, lumpy language and discomfort when opening the mouth can develop. As a result, eating is difficult and painful. Less often, an abscess develops in the neck area. This is called a parapharyngeal abscess. Here there is a risk of spreading into the chest cavity. Both abscesses must be treated as early as possible to avoid further complications such as bleeding and blood poisoning.
also read:
- Tonsillitis
- Symptoms of tonsillitis
- This is how contagious tonsillitis is
- Treatment of an abscess
Neck abscess through the wisdom teeth
A peritonsillar abscess can result from an abscessed wisdom tooth. But this happens much less often than it happens in the course of a purulent tonsillitis. Instead, abscesses in the floor of the mouth (tongue base abscesses) can develop from a diseased tooth in the lower jaw.
Symptoms of a neck abscess
One of the main symptoms of a neck abscess is the swelling of the neck.
The swelling in a neck abscess is often:
- painful and
- pressure sensitive.
The surface is usually taut, but it is painful to indent a few mm with the index finger. The more pus and inflammatory fluid there is in the abscess, the more painful the swelling usually is.
Sometimes with a neck abscess, the skin in this area becomes overheated and reddened. Depending on the location, there is also a sometimes massive functional impairment in the neck area. The larger the abscess, the greater the impairment of function, which usually manifests itself in a difficulty in turning or stretching the neck.
General symptoms such as malaise or fever can also be triggered by an abscess. As a rule, the more severe the bacterial or virus infestation, the greater the systemic symptoms. If there is a strong fever, medical help must be sought, because there is a risk that the abscess has emptied into the bloodstream and blood poisoning (sepsis) has developed. An abscess can also enlarge and infect and swell the surrounding soft tissues of the neck.
A swelling in the neck can of course also be triggered by other causes than an abscess. A reliable diagnosis can only be made by a doctor and should be made if an abscess is suspected.
Read more on the topic: Swelling of the neck
diagnosis
The diagnosis of an abscess is often made solely by interviewing the patient or by looking at the diagnosis. The most important distinction here is the exclusion of a fistula.
The fistula is characterized by the fact that it forms a corresponding duct that can connect several parts of the body. In contrast, the neck abscess is a self-contained area.
Read more on the subject at: Throat fistula
In order to be able to make this distinction, an ultrasound examination can be used. If this is not clear, a CT examination should be carried out in borderline cases. In the case of a neck abscess, an attempt can also be made to depict a possibly existing fistula by injecting a dye. In this case, the mostly blue color that was injected in the area of the conspicuous area would emerge elsewhere.
Therapy of a neck abscess
In the case of a neck abscess, conservative therapy, which consists of antibiotic treatment and draining therapy, is often sufficient.
Ointments and creams containing tar, in particular, have the property of drawing liquid out of the capsules. If this does not succeed, an attempt can be made to puncture the swelling with a sterile needle or cannula and allow the pus to drain away.
Often, however, abscess formation occurs again despite successful abscess opening. In this case, surgical removal of the neck abscess should be considered. It is important to note that there are important anatomical structures in the neck area (e.g. nerves and vessels) that must not be injured. The surgical intervention in the neck area, in addition to the other abscess operations elsewhere on the body, therefore harbors some risks that must be explained to the patient and which may make it necessary to extend the operation.
Damage to blood vessels can lead to very heavy bleeding, which may have to be stopped by an expanding operation. Muscle pulls can also be injured, which can later impair the movement of the neck. Injury to nerves is another serious risk associated with surgery.
Read more on this topic at:
- Treatment of an abscess
- Treat abscess with an ointment
- Home remedies for an abscess
Surgical removal of the neck abscess
The underlying disease that caused the neck abscess must be treated. In addition, the neck abscess must be surgically removed. Depending on the age and individual factors, the procedure is carried out under general or local anesthesia.
There are different surgical methods. In some cases, a puncture is done. It serves to relieve the abscess. In other cases, the abscess cavity is surgically opened. The goal here is that the pus can escape. In addition, damaged tissue areas are removed. In some cases the cut needs to be extended. It can also happen that the tonsils have to be removed during the operation. In addition, drainage systems can be installed inside and / or outside. In addition, antibiotic carriers can be introduced in various forms. Another antibiotic treatment is often given postoperatively in tablet form or by infusion.
The best possible advice and treatment is sought by the specialist staff before, during and after the operation. In some cases, however, complications can arise. Bleeding, secondary bleeding and scarring can follow. The risk of bleeding and secondary bleeding, especially when removing tonsils, is high. It is possible that nerves may become irritated or injured during the surgical procedure. This can result in reversible or irreversible faults. These can lead to numbness, pain, taste, swallowing and speech disorders, restricted mobility and paralysis. Tissues and structures in the vicinity of the abscess can be irritated or damaged. Allergic reactions can occur. Wound healing disorders occur less frequently.
Read more about this under Surgery of an abscess.
The prognosis for a neck abscess
After surgical removal of the neck abscess, there is usually no abscess formation at this point. If abscesses occur in other places at regular intervals, the cause should be carefully investigated. In this case, prophylactic antibiotic treatment over several weeks should be considered in order to reduce the bacterial load.