Heart failure and blood pressure - what is the connection?
introduction
Heart failure (heart failure) and high blood pressure are mainly diseases that affect the elderly (> 50 years). Over half of all over 50-year-olds are affected. However, many do not know about their illness for a long time, as the blood pressure often rises slowly over the years, the weak heart develops slowly and the body can initially adapt well.
Symptoms often appear late or are not perceived as such by those affected. From values> 120/80 one speaks of an increased blood pressure. Heart failure can develop over time due to poorly controlled blood pressure.

Causes of heart failure and blood pressure
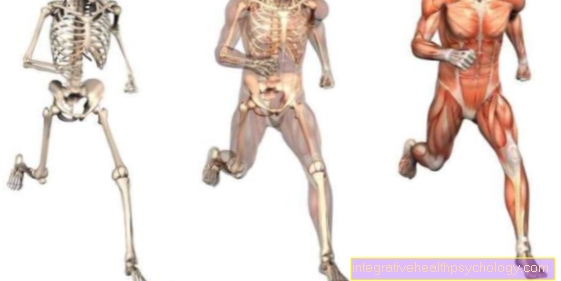
The causes of heart failure are varied. A distinction is made between functional disorders during the systole, i.e. the phase in which the blood is ejected, and disorders of the diastole, in which blood flows back into the heart. Coronary artery disease (CHD) or a heart attack can limit the pumping capacity of the heart muscle. Only a small amount of blood can be ejected per heartbeat.
Other causes are obstacles in the drainage path, e.g. Heart valves that are too narrow (aortic valve stenosis) or too high a vascular resistance, as is the case with high blood pressure. Leaking heart valves allow blood to flow back into the heart during the heartbeat, so-called pendulum blood. The heart is permanently weakened by the increased blood volume. The elasticity of the heart muscle decreases with age, which means that less blood can flow into the heart during diastole (filling phase) and therefore less blood can be expelled.
Read more on the subject at: Heart failure
high blood pressure
With age, the elasticity of the vascular walls decreases. In addition, the vessel diameter decreases due to deposits. Both of these lead to increased blood pressure. The heart must now pump against an increased resistance. In the long run, it cannot produce the normal pumping capacity, less blood is ejected into the circulation, and the stroke volume decreases.
The heart reactively tries to compensate for the drop by increasing the heart rate. This shortens the time in which the heart muscle itself is supplied with blood. The heart muscle receives fewer nutrients and oxygen, which further decreases its performance. At the same time, more water is drawn back into the body via the kidneys (reabsorption) in order to compensate for the low stroke volume. This in turn increases blood pressure. A vicious circle arises in which heart failure and high blood pressure have a negative effect on each other.
Also read the article on the topic: Symptoms of high blood pressure
Heart attack
In the event of a heart attack, sudden closure of the coronary arteries leads to an acute undersupply of the heart muscle behind it. Heart muscle cells are very susceptible to an insufficient supply of oxygen and die quickly. Depending on how long the occlusion has existed and how large the affected vessel is, small or large parts of the heart muscle can die.
The heart muscle is incapable of regeneration and functionless scars develop. As a result, the heart muscle can contract more poorly in the ejection phase and stretch less during the filling phase. Both of these result in a decrease in the pumping capacity.
For more information, see: Consequences of a heart attack
Diagnosing heart failure and blood pressure
A physical exam is performed at the beginning of the diagnosis. Existing valve diseases (constrictions / stenoses or leaking valves / insufficiency) can be recognized by heart murmurs.
The lungs are also monitored in order to rule out any possible fluid backlog in the lungs. The basic diagnosis is echocardiography - an ultrasound of the heart. The movement of the heart walls and the valves can be assessed. Existing wall movement disorders due to a heart attack scar or calcified and thickened heart valves can be identified in this way. In addition, the heart muscle thickness and the diameter of the heart chambers can be measured. In this way it can be assessed on the one hand whether the right or left heart is more severely affected and on the other hand whether it is an acute or chronic event.
With an additional Doppler examination, the blood flow in the heart can be seen and leaky valves or pendulum blood can be revealed. In the further course, an X-ray of the chest can be made to show the extent of the disease. In order to be able to rule out high blood pressure as a cause, a long-term blood pressure measurement over 24 hours is necessary.
Read more on the topic: These tests are done if you have heart failure
Concomitant symptoms
As the heart becomes increasingly weak, the blood arriving at the heart cannot continue to be pumped completely. Depending on which part of the heart is affected, it backs up into the body or lungs. There, water escapes through the vessel walls into the tissue, accumulations of water develop in the legs (leg edema) or in the lungs (pulmonary edema).
Those affected complain of heavy fat legs, shortness of breath, coughing at night and reduced performance. A congestion in the liver can lead to pain in the liver capsule. In the deficiency, congestion causes nausea and loss of appetite (congestion gastritis). Kidney dysfunction can also develop. The symptoms increase as the disease progresses and under exertion.
This article might also interest you: Symptoms of heart failure
Water in the legs
With so-called right heart failure, the heart muscle on the right side of the heart is particularly weakened. It is difficult for blood to be pumped into the pulmonary circulation from the right ventricle. The backflow occurs in front of the heart in the body's circulation. The blood is pressed through the vessel walls into the surrounding tissue. Due to the force of gravity, the liquid collects in the legs.
The girth of the legs increases equally on both sides and gets worse as the day progresses. The legs feel heavy. The skin is soft and can be dented, leaving a dent that only disappears after a while. The skin over the toes, however, is not swollen. Overnight, when lying down, the water is distributed a little and some of it flows back into the blood. It is typical here that those affected have to urinate more frequently at night.
Read more on the topic: Edema in the legs
Racing heart
In adults, the heart normally beats 60-80 times per minute at rest. A racing heart (tachycardia) is used from a frequency of 100 beats per minute. If the heart is weak, the heart can only pump a smaller amount of blood per beat. The blood circulation in the body and all organs is reduced.
In the initial stages of cardiac insufficiency, the body has various compensation mechanisms in order to maintain cardiac output (the amount of blood that the heart pumps per minute). The activation of the sympathetic system and the release of stress hormones (catecholamines) such as adrenaline and noradrenaline lead to an increase in the heart rate.This can improve the cardiac output for a short time. Palpitations can become very uncomfortable for those affected and trigger anxiety states. For the already weakened heart, a permanently increased heart rate is counterproductive, as it tires further and worsens the prognosis.
Also read the article on the topic: Symptoms of racing heart
Therapy of heart failure and blood pressure
Therapy depends on the severity of the heart failure. The classification is based on 4 degrees of severity (NYHA stages). In all stages, however, the basic therapy, consisting of weight reduction, physical activity (light endurance sports), a change in diet and a reduction in salt intake, as well as a ban on nicotine and alcohol, comes first.
In addition, risk factors need to be identified and eliminated, e.g. High blood pressure, valvular heart disease, thyroid dysfunction, anemia or heart attack. From stage 1, ACE inhibitors (e.g. ramipril) or AT1 blockers (sartans) are used as drugs of choice.
In advanced stages 2-4, aldosterone antagonists such as spironolactone or eplerenone can also be used.
Leg edema can also be improved in all stages with diuretics. Daily weight control and regular electrolyte control in the blood are essential here. If the heart rate is too fast, beta-blockers can also supplement the therapy. In the case of severe cardiac arrhythmias or very limited ejection volume, a defibrillator (ICD) can be implanted in the heart. In extremely severe cases and in very young patients, a heart transplant may be considered as the last option.
Find out more about the topic: Heart failure therapy and cardiac pills
Course of disease
The disease usually begins insidiously. In stage 1, the affected person has no symptoms, only heart disease can be diagnosed by heart echo, EKG or an existing underlying disease (coronary heart disease, heart attack, etc.). If the disease progresses, a decline in performance can be observed under greater stress. In the hospital, patients are usually asked how many floors they can go up without a break. In the further course this increases further, so that everyday work is already difficult. In the last stage, symptoms appear even at rest.
What is the life expectancy?
Life expectancy varies greatly depending on the stage at which the disease is recognized and how well the therapy works. In general, however, one has to say that the prognosis is rather bad.
Statistically, 50% survive the next 5 years after the diagnosis was made. Drugs like ACE inhibitors can now reduce overall mortality by 25%. The patient himself can also improve his prognosis by making consistent lifestyle changes and taking regular medication. However, the disease is not curable.
Further information on the subject can be found at: Life expectancy with heart failure