Hormonal contraceptives
Synonyms in a broader sense
Pill, birth control pill, Gynefix, depot injection, hormone stick, hormone patch
definition
Contraceptives are used to prevent pregnancy and to bridge the fertile days. There are different methods of contraception.
Hormonal birth control is a very popular method for women.
Different methods
There are different hormonal contraceptives available. We will go into the following methods in detail.
Hormonal contraception methods:
- birth control pills
- The three-month injection
- Hormonal IUD
- Vaginal ring
- Hormone stick
- Hormonal patch
Do you want basic information about your options for contraception? You can find them all with us
- Overview of contraception methods
Cerazette is also a contraceptive method in tablet form. You should also deal with this promising form of contraception before you decide on a variant. For the most important information, read: Cerazette - the most important information at a glance
Pearl Index
How safe the individual contraceptive methods are is checked in clinical studies.The reliability of a particular contraceptive can be assessed using the Pearl Index (PI).
The Pearl Index shows how many out of 100 women got pregnant using a single specific method of contraception in a specific period of time. A Pearl Index of 5, for example, means that 5 out of 100 women became pregnant using a certain method of contraception. The bigger is the numerical value of the Pearl Index, the more unsafe is the contraceptive.
The spermatic duct valve is a new invention for male contraception.
Find out more about this in our article:
The spermatic duct valve - an evolution in contraception?
The pill

The pill is the most popular hormonal contraceptive. The birth control pill was first introduced in the US in 1960 and in Europe in 1961 and has been one of the most widely used contraceptives ever since.
The pill contains the hormones estrogen and progestin as a hormonal active ingredient. The hormonal components of the pill, which were still in high doses in the past, have been reduced more and more up to the present day. Thus, with doses that are just high enough to ensure a safe effect of the pill, the side effects of the pill (see: Thrombosis risk of the pill) are greatly reduced and the pill can be used well as a contraceptive even in adolescents.
In some studies it has been shown that women affected by taking the birth control pill have less severe PMS symptoms. Read more about this under: This is how premenstrual syndrome is treated
The morning-after pill
What is special about the morning-after pill is that if one of the other contraceptives is used inappropriately, it can be taken up to 48 hours after sexual intercourse and can prevent pregnancy. It consists of tablets that contain high doses of gestagens or gestagens and oestrogens and which prevent ovulation and implantation of the egg cell.
For more information on this topic, see: morning-after pill
The three-month injection

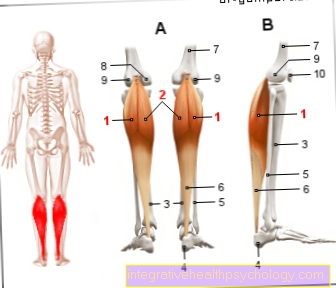
In the Three-month syringe, also depot syringe called, it is a hormonal contraceptive that only uses the hormone Progestin contains. It will all two to three months The gynecologist will give an injection either in the upper arm muscle (deltoid muscle = Musculus deltoideus) or in the gluteus muscle (Musculus gluteus).
After an injection, the hormone accumulates in the respective muscle and is then gradually released into the body. Since the delivery takes place within a period of 8 to 12 weeks, an injection is also a preventive effect for such a long time.
The Effect of the progestin in an injection is analogous to the effect of the progestin in the birth control pill. Ovulation (ovulation) prevents the mucus of the Cervix (Cervical mucus) is thickened in order for the Sperm to be harder to happen and the correct structure of the uterine lining (endometrium) is made more difficult, so that an egg can only implant with difficulty.
The three-month injection is prescribed to women who use other contraceptives such as the Pill not tolerated or sent to nursing mothers. Breastfeeding mothers should, at best, not use hormonal contraception at all, but rather use a different type of contraceptive. The three - month injection is again the best hormonal contraceptive for breastfeeding mothers, as it only contains progestins and no estrogens and therefore does not affect the production of breast milk as much.
As Side effects the three-month injection results in weight gain, Mood swings, Reducing the Lust (Loss of libido) and irregular bleeding (spotting and intermenstrual bleeding = menorrhagia and metrorrhagia). Menstrual bleeding can also stop entirely. After stopping the injections, the natural ovulation cycle may take some time to re-establish itself.
It is also possible that the regular cycle no longer levels off after the three-month injection has been stopped. Another disadvantage of the three-month injection is that if the depot gestagen is intolerant, it cannot simply be discontinued, but rather one has to wait for the depot effect to subside. Interactions with antibiotics also lead to a loss of effectiveness of the hormone while taking it.
It is certainly an advantage that, in contrast to the pill, one does not have to think about the daily pill intake and safe contraception with one Pearl index around 0.5 Has. However, the three-month injection is not recommended for young women who later wish to have children, which is due to the possible problems after stopping the injection.
Read more on the subject at: Three-month syringe
Hormonal IUD
The hormone coil is made of plastic and is filled with the hormone progestin inside. It is inserted into the uterus (uterus) during a gynecological examination by the gynecologist during menstrual bleeding (intramenstrual). It can remain there for a maximum of five years and develop its effect. The procedure is usually painless. Sometimes, however, this can result in injuries to the uterus or the cervix (cervix uteri). Mild pain can also arise a few hours after the procedure. It is important that the correct fit of the hormonal IUD is checked after the procedure and at regular intervals.
The contraceptive effect occurs in two different ways. On the one hand, the hormonal coil acts as a mechanical disruptive factor and prevents the sperm from ascending towards the egg cell. The path of the sperm is blocked, so to speak. On the other hand, the hormone coil continuously releases progestins, so that pregnancy is prevented at the same time by hormones. As with the birth control pill, ovulation is prevented and a plug of mucus forms in the cervix, which makes it difficult for the sperm to penetrate the uterus (uterus).
Since the IUD does not contain any oestrogens, it is particularly popular to prescribe it to women who cannot tolerate oestrogens and to women who do not want to think about taking pills every day.
The hormonal IUD is for young women who want to have children later Not to recommend. It is also not used for malformations of the uterus (uterine malformations).
The advantage is certainly that with a Pearl Index of approx. 0.15, very safe contraception is guaranteed. In addition, in the best case scenario, women do not have to worry about contraception for five years. Menstrual bleeding also becomes smaller, shorter and less painful in some women.
Disadvantages result from the action of the progestin:
- Depressed moods (depression)
- Mood swings and
- an increase in weight
can come about as a result of the hormone. Since the hormone coil is made of plastic and is therefore a foreign body, it can be rejected by the body. This mainly happens in the first few months after use.
In rare cases, infections can also occur after an operation.
More detailed information is available at spiral
Also our article on inserting the IUD could be of interest to you.
Vaginal ring
The vaginal ring is a soft, flexible plastic ring that contains both progestin and estrogens inside. It is prescribed by the gynecologist and can then be inserted into the vagina by the woman herself during the first five days of menstrual bleeding. The insertion is similar to that of a tampon.
The vaginal ring should be used in such a way that the woman does not perceive it as annoying, at best not at all. It may sometimes fall out, for example during intercourse. It should then simply be used again. As long as the vaginal ring has not been removed from the vagina for more than three hours, the safety of the contraceptive will not be affected. It can therefore also be deliberately removed for a short time, for example if it is found to be a nuisance during sexual intercourse.
The vaginal ring remains in the vagina for a total of 21 days and is then removed. A new vaginal ring is inserted after seven days of the break, during which the menstrual bleeding occurs.
The vaginal ring releases an equal amount of progestin and estrogen every day, thus ensuring a constant level of hormones.
The effect is therefore identical to that of the birth control pill. The hormones prevent ovulation (ovulation) so that no mature, fertile egg cell is ready for fertilization. Due to the thickening of the mucous plug of the cervix and the inhibition of the growth of the uterine lining (endometrium), on the one hand the sperm cannot reach the egg cell so easily, and on the other hand an egg cell cannot implant well because the uterine lining is not built up.
With a Pearl Index of 0.5, the vaginal ring is just as safe a contraceptive as the birth control pill.
You might also be interested in: Ovulation and temperature - what is the relationship?
The continuous release of progestins and estrogens results in side effects that are identical to those of the pill. The growth of hormone-dependent tumors is favored (hormone-dependent breast cancer = breast carcinoma) and the development of benign liver tumors (focal, nodular hyperplasia and liver cell adenoma).
It can be used to:
- Weight gain
- Water retention / edema
- thrombosis
- Mood swings and
- Loss of libido
come.
Therefore, women with certain pre-existing conditions or risk factors should use a different contraceptive. These include women with an increased risk of thrombosis, existing liver problems, a previous heart attack or embolism, but also older women (from the age of 30) if they are heavy smokers. The gynecologist should decide whether the vaginal ring is suitable for a woman after exploring possible risk factors. In principle, after the exclusion of contraindications, the vaginal ring is very suitable for all women who do not want to think about taking pills every day.
The advantage over taking pills is that the hormones in the vaginal ring are absorbed through the vaginal lining and not through the intestinal lining. Thus, diarrhea and vomiting do not affect the effect of the vaginal ring. This is to be distinguished from the loss of effectiveness of the hormones when taking antibiotics. When taking antibiotics, the effect of the hormones is always influenced, whether with the pill or the vaginal ring. The reason for this is that the hormones and antibiotics are each metabolized in the liver and can influence each other there.
Women rarely report that the vaginal ring can be felt during sexual intercourse or even disturbs it. Ultimately, every woman should find out for herself whether this method of contraception is best for her.
Hormone stick

Hormone stick are thin sticks made of plastic, which are filled with the hormone progestin inside. They will be for in the upper arm planted (implanted). This procedure takes place on an outpatient basis. After numbing the relevant area of the skin, a stick is pushed into the skin with a thin needle and implanted there.
It then remains for a maximum of three years at this point and has a preventive effect for three years from the date of implantation. If there is a desire to have children before the end of the three years or if the woman no longer wants to use the hormone stick for contraception for other reasons, it can be removed beforehand.
The preventive effect is due to the hormone Progestin reached. Like the birth control pill, the hormone stick prevents ovulation by releasing progestin from its depot every day. In addition, the mucous membrane of the uterus (endometrium) is not built up, so that implantation of the egg is not possible. Additionally, the mucus of the cervix is thickened, allowing the sperm to penetrate into the uterus (Uterus) is difficult.
As Side effectsAs with the birth control pill, mood swings, bleeding disorders (intermenstrual bleeding and spotting = menorrhagia and metrorrhagia), breast tenderness and weight gain occur.
In addition, it can sometimes be difficult to remove the hormone stick because it can grow in too tightly.
Since the hormone stick contains only progestins and no estrogens, it is particularly suitable for women who cannot tolerate estrogens or who have certain previous illnesses or risk factors that prevent them from using an estrogen-based contraceptive. Risk factors can be, for example, an existing increased risk of thrombosis.
In any case, it is advantageous that the woman does not have to think about the daily pill intake and with a very safe contraceptive, with one Pearl index from 0.00 - 0.05 prevent.
Since the hormones from the implantation site enter the bloodstream via the tissue and are not absorbed through the gastrointestinal tract, as is the case with birth control pills, the hormone rod does not lose its effectiveness in the event of diarrhea or vomiting.
However, the effectiveness of antibiotics or anti-epileptic drugs (anti-seizure medication) is limited, so another (mechanical) contraceptive should be used during this time.
Hormonal patch
Hormone patches work in a similar way to birth control pills. They can be anywhere on the body except the Chest, to be glued and remain there for seven days. After the seven days, a new hormone patch is placed on the skin and remains there for seven days. Then another, third patch follows for another seven days. This is followed by a seven-day break until a new three-plaster pack can be started. The patch continuously releases hormones into the tissue that enter the bloodstream and, like the birth control pill, ovulation and the structure of the lining of the uterus (endometrium).
According to the manufacturer, the patch stays on the skin even in extreme situations, such as in the sauna, swimming pool or whirlpool.
Should it fall off, a new hormone patch must be stuck on the skin within the next 48 hours.
The Side effects correspond to those of the birth control pill. For example, the blood changes so that the patch is not suitable for women at risk of thrombosis. In addition, it can lead to an increase in weight, depression, water retention (edema) and an increase in appetite. The skin to which the patch is attached can also become irritated. Therefore, it is best to stick it to a different place each time.
Since the hormones are not absorbed in the gastrointestinal tract, their effect is not affected by diarrhea or vomiting.
With a Pearl index of about 0.88 is the hormonal patch as well as the birth control pill very sure.