TMJ osteoarthritis
synonym
TMJ wear
introduction
The TMJ arthrosis belongs to the most common diseases occurring in Germany in the area of Oral cavity. In Germany alone, according to extensive studies, around 10 million patients are approached continuously or at least temporarily TMJ osteoarthritis Suffer.
In the TMJ arthrosis is it a Wear and tear disease of Temporomandibular jointthat in most cases by Incorrect loads and mechanical wear the articular surfaces consisting of cartilage.
The risk Developing TMJ osteoarthritis increases with the Age, something every third person from the age of about 70 years suffers at least from a temporary form of TMJ arthrosis. In addition to age, there is also a possible one genetic predisposition or heavy physical labor play a vital role in developing this disorder.

TMJ anatomy
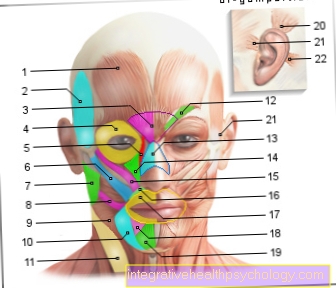
The Temporomandibular joint (lat. Temporo-mandibular articulation) provides a flexible connection between the bony Upper- (lat. Maxilla) and the Lower jaw (lat. Mandible) represent.
The Mandibular fossa (lat. Mandibular fossa) is in direct contact with the jaw joint Maxillary head (Caput mandibulae) a.
Within this connection, the upper jawbone forms the rather stare Part of the temporomandibular joint, whereas the lower jaw versatile is clamped in the joint. These two structures are only made possible by the movable one Cartilage (Articular disc) separated from each other. In this way, the cartilage disc divides the temporomandibular joint into two functionally independent parts, the upper and the lower Joint space.
The upper part of the joint (upper joint space) is for the execution of Sliding movements responsible, Turning movements are mainly implemented in the area of the lower joint space. At the Chewing process or that Speak However, these two ranges of motion have to be cleverly combined.
in the Temporomandibular joint can therefore also so-called Rotating and sliding movements are executed. The lower jaw pit forms a kind of joint socket and is forwarded by one under the name Articular tuberosity known structure limited. The rear limit is the so-called Retroarticular process.
causes
The causes one TMJ arthrosis can be diverse.
In many affected patients, the loss of the Molars over a longer period of time to changes in the Bone structure and for the development of TMJ arthrosis. The basis of this phenomenon is the fact that the "normal" Load pattern the bone sections move strongly after losing the molars and for this reason Incorrect loads be provoked.
In addition, such Incorrect loads of the Jawbone triggered by:
- worn or incorrectly adjusted Crown,
- bridges
- and or Dental fillings
In addition, many affected patients report that they grind their teeth in particularly stressful situations at night.
In some cases the occurrence of TMJ osteoarthritis can be caused by the so-called CMD syndrome (Craniomandibular dysfunction) are provoked.
At the CMD syndrome is it a pronounced malfunction of the Temporomandibular joint parts itself. Pronounced misaligned teeth that are not, only incomplete or faulty orthodontic The most common triggers are one Craniomandibular dysfunctionwhich can ultimately lead to the development of TMJ osteoarthritis.
Also a pronounced one Tooth decay (especially in the area of to bake- and Premolars) can lead to a long-term failure to take appropriate treatment TMJ osteoarthritis to lead.
Symptoms
To the same extent as the causes of this disease, the symptoms of TMJ osteoarthritis can take many forms.
The symptoms experienced by the affected patient depend on:
- On the one hand from the cause of the TMJ osteoarthritis and
- on the other hand on the severity of the disease.
In the early stages of TMJ arthrosis, the affected person usually feels mild to strong feelings of tension in the area of the masticatory muscles and the joint itself.
The occurrence of back and / or neck pain as an accompanying symptom can also provide an initial indication of a possible illness. In addition, the signs of wear and tear on the cartilaginous joint parts can increase the incorrect loading of the temporomandibular joints.
The consequences are, among other things, the development of ventilation disorders of the inner ear and ear pain.
Especially with:
- Chew,
- when yawning,
- Many patients feel a pulling force when speaking and opening their mouths.
The temporomandibular joint arthrosis can lead to pain sensations in the area of the temporomandibular joint at an early stage. The further the disease progresses, the more intensely the typical symptoms are perceived by the patient. Over time, the jaw opening and closing become increasingly restricted. The majority of the affected patients report early on of the occurrence of cracking and grinding noises during mouth opening.
Read on under: Lock jaw
Diagnosis of TMJ osteoarthritis
The diagnosis of TMJ osteoarthritis primarily takes place at the level of imaging procedures.
This means that for a reliable assessment of the joint condition, an X-ray image must be made that fully depicts the jawbone and the teeth embedded in it, as well as the temporomandibular joint itself.
As a rule, the so-called orthopantomogram (short: OPG) serves as a significant aid in the diagnosis of TMJ arthrosis.
In addition, the tissue around the temporomandibular joint must be assessed with the help of other imaging methods. This necessity is based on the fact that in the course of TMJ osteoarthritis typical changes occur in the soft tissue area, which can provide an indication of the underlying problem.
The attending physician may also order an MRI of the temporomandibular joint.
therapy
Since there are various causes for the development of TMJ osteoarthritis, the therapy of this disease is primarily aimed at eliminating the underlying problem.
In the course of this, the search for the cause is the top priority for an optimal osteoarthritis treatment. If carious defects are the reason for the incorrect loading of the temporomandibular joints and the formation of signs of wear, these must be removed and the affected teeth filled with fillings.
In temporomandibular joint osteoarthritis patients who have faulty, worn or incorrectly adjusted crowns, bridges or dental fillings, these too must be replaced by a more suitable prosthetic restoration in order to relieve the temporomandibular joint in the long term.
For patients who report the habit of grinding their teeth due to stress, various relaxation exercises need to be learned and used regularly.
Furthermore, it should be noted that TMJ osteoarthritis is a sign of wear and tear, which usually results in the occurrence of inflammatory processes in the area of the affected joints. For this reason, in addition to eliminating the cause, anti-inflammatory therapy is also advisable.
See below: Grinding splint
The general reduction of stress is also essential for the effective and, above all, long-term treatment of TMJ osteoarthritis. This is related to the fact that excessive stress has a particularly negative influence on the organism. The result is the increased formation of specific inflammatory factors that promote TMJ arthrosis and worsen the symptoms. In addition, the tension in the course of the stress leads to night-time grinding of teeth in many patients. Some people also report that they react to emotional stress by clenching the rows of teeth. This habit also leads to increased stress on the temporomandibular joints.
Furthermore, relaxation of the masticatory muscles can help reduce the pain and tension that occurs in the course of TMJ osteoarthritis. For this reason, the use of acupuncture needles can be useful for affected patients.
In order to counteract the inflammatory processes in the temporomandibular joint area, it may be necessary to switch to an anti-inflammatory diet. Especially
- Fish (e.g. herring or mackerel),
- herbs and spices
can help to contain the inflammatory reaction of the organism. Wheat should be avoided as far as possible in the presence of TMJ osteoarthritis. In addition, certain foods can promote joint development and thus the regeneration of the temporomandibular joints. Patients who suffer from TMJ osteoarthritis should consume sufficient nutrients every day if possible.
You might also be interested in: Proper nutrition for osteoarthritis
Foods containing collagen, such as horsetail, promote the networking of collagen fibers, the main component of cartilage in the jaw joints. Food supplements containing glucosamine and chondroitin sulphate can also help to regenerate the joint cartilage.