Parathyroid
Synonyms in a broader sense
- Accessory thyroid glands
- Epithelial bodies
Medical: parathyroid gland
English: parathyroid glands
anatomy
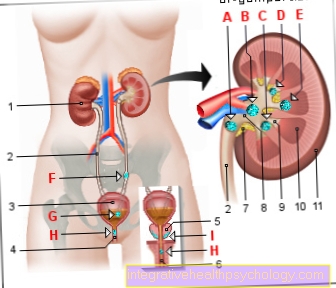
The parathyroid glands are four lens-sized glands weighing approx. 40 mg. They lie behind the thyroid gland. Usually two of them are at the top (pole) of the thyroid lobes, while the other two are at the bottom pole (see also: Thyroid). The lower thyroid glands are rarely found on the thymus or even in the middle chest space between the lungs (this space is also known as the mediastinum). Sometimes additional parathyroid glands are found.
Illustration of the thyroid

thyroid
- Hyoid bone -
Os hyoideum - Thyroid cartilage
Hyoid bone membrane -
Thyrohyoid membrane - Thyroid cartilage -
Cartilago thyroidea - Cricoid cartilage
Thyroid cartilage muscle -
Cricothyroid muscle - Upper Parathyroid -.
Parathyroid gland
superior - Thyroid constriction -
Isthmus glandulae
thyroideae - Thyroid,
right lobe -
Glandula thyroidea,
Lobus dexter - Lower Parathyroid -.
Parathyroid gland
inferior - Trachea - Trachea
You can find an overview of all Dr-Gumpert images at: medical illustrations
function
In contrast to many other glands (e.g. the pancreas = Pancreas), the parathyroid gland (glandula parathyroidea) does not have its own outlet ducts for the secretion it forms, the hormone Parathyroid hormone (short PTH, also: parathyrin). Therefore, the messenger substance is released (secreted) directly into the blood and arrives at your destination. This secretion mechanism is also known as endocrine secretion. That is why the parathyroid glands are criss-crossed by a dense network of capillaries, the capillaries of which have a special structure.
Capillaries are the smallest human vessels through which a red blood cell (erythrocyte) can fit.
In the parathyroid gland there are special, so-called fenestrated capillaries, the cells of which do not form a tightly enclosed vessel, but rather have small gaps (so-called 70 nm “windows”) and thus allow the hormone to pass into the bloodstream without the blood components escaping can. Target tissues, i.e. the place of action, of the parathyroid hormone are bones and kidney. There the peptide hormone (i.e. it is made up of 10 to 100 amino acids) intervenes in a regulating manner in the calcium metabolism. The amount of hormones is controlled by a simple feedback mechanism: the amount of hormone released depends on the Calcium concentration in the blood. The parathyroid glands have their own "calcium sensor" for this.
If there is a lack of Calcium / calcium parathyroid hormone is increasingly released into the blood; if there is sufficient calcium in the blood, secretion (release) is inhibited. The hormone promotes the supply of calcium through two mechanisms: Calcium is released from the bone by degrading cells, the osteoclasts. These are stimulated / activated by parathyroid hormone. In the kidney, the hormone prevents too much calcium from being excreted in the urine: (It causes calcium to be reabsorbed from the primary urine produced in the kidney and supplied to the organism.) It reduces the excretion of calcium in the urine. This effect is reinforced indirectly by promoting the formation of Vitamin D, which also reduces the excretion of calcium with the kidneys and furthermore promotes the absorption from food in the intestine. Both Hormones look like that osteoporosis (Bone decalcification).
The concentration of the blood calcium is kept constant within narrow limits at 2.5 mmol per liter. Furthermore, PTH (parathyroid hormone) promotes the excretion of phosphate about the kidney.
Parathyroid disorders
The Parathyroid is vital; a complete absence (agenesis) is incompatible with life. Accidental removal of or damage to epithelial cells during thyroid surgery or an underactive (hypoparathyroidism) can have serious consequences: The drop in blood calcium levels leads to hypocalcemia, which is characterized by seizures and general over-excitability of the Musculature makes noticeable.
However, hyperfunction of the parathyroid glands is no less dangerous: Initially, it manifests itself through rapid fatigue, muscle weakness, depressions and anxiety. Inflammation of the pancreas is also common (Pancreatitis) and ulcers of the stomach (Ulcer) on. In serious cases there is a life-threatening threat hypercalcemic crisis with calcifications of the lungs, kidneys and stomach. Hence the name "stone, leg, stomach pain."
Causes of hyperfunction are called primary hyperparathyroidism if they are caused by a disease of the parathyroid glands themselves. The most common underlying cause is a benign tumor (known as an adenoma). Hyperparathyroidism is hereditary in the clinical picture of Multiple endocrine neoplasia (short MEN) caused by an enlargement (hyperplasia) of the parathyroid glands and tumors in the pituitary gland (pituitary gland), the pancreas, the Small intestine as well as various other organs. In contrast to this, one speaks of secondary hyperparathreoidism when the disturbed calcium balance is not caused by the parathyroid glands themselves, but by other diseases. In most cases, a kidney disease is in the foreground, which leads to such a high loss of calcium that an increased secretion of parathyroid hormone is necessary to provide the necessary amounts of calcium. As a result, there is excessive growth (hyperplasia) with the following overfunction of the epithelial cells. The symptoms largely correspond to those of primary hyperparathyroidism. Damage to the skeletal system is often caused by the increased release of calcium from the bones, resulting in bone decalcification (osteoporosis). The disease is not based on early enough Laboratory values (increased calcium in the blood) recognized, the breakdown of bone tissue causes a tendency to spontaneous fractures. According to its first description, the anatomy professor v. Recklinghausen, the full picture of the disease has been known as Osteodystrophia generalisata (generalized destruction of the bone) since 1891.



















-buschmcke.jpg)