Cartilage damage behind the kneecap
synonym
Chondropathia patellae
definition
A Cartilage damage behind the Kneecap (medical: Chondropathia patellae) denotes a painful change in the Cartilage tissue behind the kneecap, which especially with athletes occurs and in many cases to a Overload is due.

The cartilage behind the kneecap is a Buffer between the kneecapthat lies in front of the knee and the bonewhich that Knee joint form. It serves as a kind of buffer and absorbs mechanical loads for the knee joint. It is also part of the ligament that binds the strongest thigh muscle (Quadriceps femoris) connects to the shin and creates one Lever arm to maximize force between thigh and lower leg.
Various causes can lead to the cartilage behind the patella being damaged. Such damage often leads to a so-called patellofemoral pain syndrome, which is the most common cause of chronic knee pain.
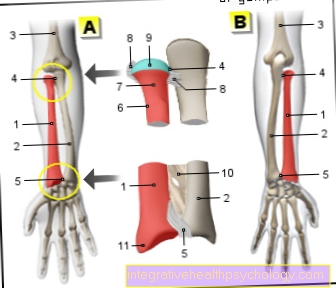
Illustration of a cartilage damage

- Articular cartilage
(hyaline cartilage) -
Cartilago articularis - Cartilage remodeling zone
in bones -
Zona ossificationis - Joint body (articular gnar
of the femur) -
Femoral condyle - Femur -
Femur - Articular cartilage -
Cartilago articularis - Outer band -
Ligamentum collaterale fibulare - Outer meniscus -
Lateral meniscus - Inner meniscus -
Meniscus medialis - Fibula - Fibula
- Shin - Tibia
You can find an overview of all Dr-Gumpert images at: medical illustrations
Causes and Risk Factors
Risk factors for that Development of cartilage damage behind the kneecap divide into three groups: Overuse, injuries and anatomical factors.
These three groups result in certain risk groups that are often confronted with the diagnosis of cartilage damage behind the kneecap. Already from the synonym often used, especially in the USA "runner's knee" it can be deduced that above all athletes and among them above all runner, are particularly affected. It also follows that many of the Affected younger age are what is unusual for other cartilage damage.
Since the kneecap and its surrounding structures including the cartilage act as a kind of buffer for the knee joint, it is logical that traumatic injuries (Knee contusion), and especially those who have a hit on the kneecap as a result, also favor the development of this clinical picture. Such cartilage damage is common after traffic accidents and sports injuries to observe.
A functioning knee joint is a requirement for the frictionless movement in everyday life. With each step, the kneecap is moved over the knee joint. If there are congenital diseases that affect the knee joint affect anatomically, this can also result in cartilage damage behind the kneecap. These include congenital hip malpositions, a X position the legs, different leg lengths and malformations or misalignments of the kneecap.
It is also noticeable that mostly young women Are affected by cartilage damage behind the kneecap. Attempted explanations see the reason for this in an anatomical predisposition: through the wider pelvis a woman compared to the man they tend to suffer from cartilage damage behind the kneecap.
Persons of both sexes are also often affected during puberty, which is often explained by a "growth spurt" that during this time a particular stress on the joints represents.
In general, however, one can say that in many cases a exact cause for the appearance of cartilage damage behind the kneecap cannot be found.
Appointment with a knee specialist?
I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The knee joint is one of the joints with the greatest stress.
Therefore, the treatment of the knee joint (e.g. meniscus tear, cartilage damage, cruciate ligament damage, runner's knee, etc.) requires a lot of experience.
I treat a wide variety of knee diseases in a conservative way.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
Cartilage damage behind the kneecap from exercise
In connection with sport, it occurs both through improper or excessive stress and through sports accidents Cartilage damage behind the kneecap.
Since many sports, such as soccer, skiing and jogging, put a lot of strain on the knee joint, bad posture has a very strong effect. The cartilage surfaces of the bones then rub against each other more intensely and wear off.
The development of cartilage damage is favored by congenital misalignments of the legs, such as Knock knees, and by being overweight.
Also from previous injuries to the knee joint, such as Cruciate ligament tears or Meniscus damage, the cartilage behind the kneecap can be exposed to increased stress, which leads to increased wear.
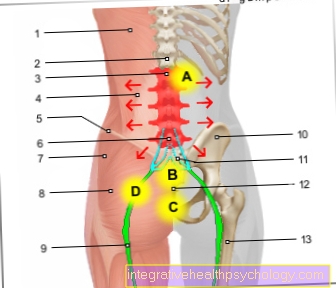
Symptoms
It is characteristic pain for the cartilage damage behind the kneecap a dull pain that is difficult to localize which of those affected as pain "in" the knee joint such as "behind", "around" or "under" the kneecap is described.
A Increase in pain sensation occurs during sports activities such as to jog, Hopping, but also with everyday movements like Climb stairs or long periods of sitting and squatting on. The symptoms are mostly called chronic pain described, although they can also be traced back to a specific injury. The symptoms can one-sided, such as both sides occur.
The Swelling of the knee is not a typical sign for this cartilage damage, with some sufferers a certain "Stiffness" in the Knee joint describe. A "popping" or "cracking" feeling is also often described. If there are also loose pieces of cartilage, a Restriction of movement present and symptomatic.
diagnosis

The diagnosis for cartilage damage behind the kneecap may develop sometimes as difficult. It is not always easy to assess whether the knee joint is damaged or the cartilage behind the kneecap is affected. This can be done primarily through a detailed anamnesis (Medical history) happen and through advanced movement testswho may detect a limitation of the joint. So is often one Tension pain in the patella area (Kneecap) given as well as a effusionwhich can be determined through specific orthopedic tests.
Imaging procedures are relatively well suited for diagnosis, i.e. the presence of one Cartilage damage behind the kneecap, are also good at rule out other conditions with similar symptoms to be able to.
In rare cases it may be necessary to have a Knee arthroscopy (Knee arthroscopy) to be able to safely rule out other diseases.
The two most important imaging procedures to make the diagnosis is:
- the X-ray image (X-ray knee in 3 planes)
and - the MRI of the knee
The X-ray image shows bony changes that depend on the degree of Osteoarthritis of the kneecap closes. The cartilage damage cannot be assessed directly.Nevertheless, the X-ray image is a valuable diagnostic tool to assess the structure of the knee joint and the kneecap.
The MRI of the knee can do the actual Cartilage damage pose in the knee joint. The extent of the cartilage damage can be determined precisely because the cartilage behind the kneecap is particularly thick. The MRI divides cartilage damage into four degrees of severity.
Read more about our topics:
- X-ray image
and - MRI of the knee
Classification degrees 0 - 4
Cartilage damage behind the kneecap is divided into different degrees of severity, depending on the surface of the cartilage and the depth of the damage.
Depending on the severity, different therapeutic approaches are carried out.
- At a Grade 1 cartilage damage the cartilage surface is still preserved, but may contain softening (Chondromalacia).
- From Grade 2 There are also cracks in the cartilage that are as long as half the thickness of the cartilage. In the first two stages, cartilage damage is often barely or barely noticeable.
- From damage to the 3rd degree those affected usually have stress pain. Here, the cartilage damage usually extends to the bone.
- With a cartilage damage Grade 4 there is nothing left of the cartilage. It is completely worn out and the bone is exposed. One speaks of a so-called Bald cartilage.
Since the Pain in the knee usually only occur when the cartilage has already been destroyed, conservative therapy is then often no longer possible. Once cartilage wears out, it does not reform.
therapy
The appropriate therapy as well as the success of the therapy for the cartilage damage in the knee joint depend crucially on the given circumstances from. So leave discomfort that during the puberty due to a growth spurt they usually re-emerge after a while. Of this, symptoms that point to a massive overload cannot necessarily be assumed.
It is clear that certain loadsthat occur mainly during sporting activities, must be avoided. Changes in training procedures in terms of duration, intensity and frequency should also be taken into account and usually reversed. Everyday movements toowhich put a strain on the knee joint and the affected area should be avoided. This includes frequent climbing stairs, carrying heavy loads and sitting or squatting all the time.
Sometimes it may be necessary pain reliever drugs to take to relieve the symptoms of cartilage damage behind the kneecap. So-called NSAIDs are often used here, to which acetylsalicylic acid (aspirin), Ibuprofen and Diclofenac counting. In addition to the pain reliever component, these also have a anti-inflammatory effect on the affected area, which is also beneficial for the healing success.
Treatment success also have according to recent studies Physiotherapy and physical treatment methods, which is why these are now included in the treatment. Physiotherapy is supposed to joint take the "stiffness" that some patients complain of with cartilage damage behind the kneecap. Physical therapy approaches include, among other things Ultrasonic, Cold and heat therapy and Electrotherapy.
To treatments that the person concerned carry out himself can also include physiotherapy exercises that can be shown to the patient by a physiotherapist or doctor regular implementation can significantly improve the chances of recovery. Women are also advised Flat-heeled shoes to wear so as not to put unnecessary strain on the cartilage.
Special bandages can also provide relief for long-lasting symptoms. The main aim of these bandages is to restore the stability of the joint.
A surgical intervention is only suggested in cases where no chance of healing through non-surgical attempts at healing. Surgical intervention is therefore only useful in certain cases. Surgical attempts can be made to regenerate the cartilage using a so-called Pridie hole to stimulate. Here, holes are drilled through the kneecap, and with them the tissue that lies around the cartilage for the formation of new cartilage (so-called. Replacement cartilage) stimulated.
The surgical procedure is also useful if the cause of the damage is on one increased pressure on the kneecap is due. This pressure can be reduced by means of an operation, which leads to better sliding movement of the kneecap. Other surgical approaches to treating cartilage damage behind the kneecap can be Microfracturing, Mosaic sculpture and a Cartilage graft be.
The operation for cartilage damage
Surgery is especially serious in young patients with Cartilage damage carried out behind the kneecap to prevent further progression of the damage to osteoarthritis.
Often an operation consists in smoothing the inner surface of the joint and "clean". This procedure is called Debridement and is performed arthroscopically. This means that there is no open operation and the knee is cut open, but only small, approximately 1cm long incisions are made, where the surgical instruments and a camera are inserted. With this method, any loose pieces of cartilage that may be present are removed and the synovial membrane is smoothed to alleviate the symptoms.
In addition, there are a few other surgical procedures that can be performed if there is cartilage damage behind the kneecap. A so-called Abrasion plastic is rarely performed and can only be used for minor cartilage damage. At a Arthroscopy the remaining cartilage is milled away in the damaged cartilage area and hemorrhage occurs from the Bone marrow. As a result, so-called stem cells reach the defect area and form new cartilage. However, this newly formed bone is not as strong and resilient as the original cartilage.
In the Mosaic sculpture the cartilage is punched out in the area of the damage and replaced by a cylinder punched out in another part of the body. The intact cartilage is taken from another part of the knee joint that is not so heavily stressed. Depending on the size of the cartilage damage, one or more cylinders must be removed.
A similar process is the osteochondral allografts. Here, however, the newly inserted cylinder is synthetic and supports the cartilage and bone structure by absorbing the stem cells necessary for the new formation and being broken down parallel to the new cartilage formation.
The Microfracturing is a very common procedure for the surgical treatment of cartilage damage behind the kneecap. This can be done arthroscopically, which means that it is not an open operation, but a minimally invasive procedure. Therefore it carries comparatively few risks for the patient. The procedure consists in making small holes in the bone under the cartilage is located. This leads to bleeding into the damaged joint from the bone marrow and certain cells in the blood attach themselves to the places where the holes are in order to form new cartilage substance. This procedure is useful if there is cartilage damage to the shin or femur. On the back of the kneecap, the pressure and friction are so great that the newly formed cartilage tissue is quickly rubbed off again.
Another method is the so-called autologous cartilage cell transplantation (ACT). The ACT is an open transplantation of cartilage cells that were previously grown and inserted into the damaged cartilage. Two interventions are necessary for this. Both can now be performed arthroscopically. During the first knee examination, cartilage cells are taken from a less stressed area of the knee joint. These cartilage cells are then multiplied in the laboratory and after about 3 to 4 weeks the body's own cartilage cells are introduced into the area of the damaged cartilage.
How will the result
The result of most operations is not very satisfactory because the area behind the kneecap is very stressed. Cartilage that has been stimulated to regenerate by the various surgical procedures wears off quickly. Often it only makes sense to clean the joint.
Read more on the topic: Arthroscopy of the knee joint
forecast
The prognosis after the diagnosis of cartilage damage behind the kneecap falls usually cheap out. In most cases it can be assumed that a Healing possible but it is take a long time can.
For many sufferers, the pain leaves spontaneously after a few weeks and even disappear completely. However, there may be pain after years of freedom from symptoms occur again. In rare cases, damage to the cartilage behind the kneecap can result in a arthrosis emerge.
prophylaxis
There are a few Behaviorswhich may prevent cartilage damage behind the kneecap.
- Excessive training should definitely be avoided. Especially sportswhich are associated with an increased risk of damage to the cartilage should be avoided. This includes above all to jog, but also basketball, volleyball and To go biking with high translation.
- A unilateral burden only one knee should also be avoided. If the whole body weight often only has to be worn from one side, this greatly increases the incidence of cartilage damage.
- Certain Occupational groupsassociated with a greatly increased load on the patella, such as Tiler, should consciously protect the knee and avoid kneeling work. Alternatively to the Use of a pad are advised.