Complication of hip replacement surgery
Synonyms in a broader sense
- Artificial hip joint
- Total hip replacement (HTEP or HTE)
- Hip joint prosthesis
- Total hip replacement
definition
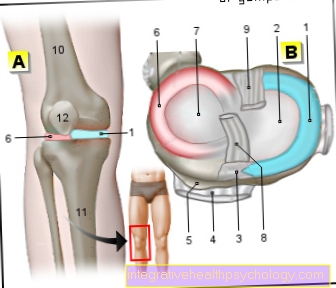
A total hip joint prosthesis is understood to mean a artificial hip joint. The artificial hip joint consists of the same parts as the human hip joint. During the prosthesis implantation, the pelvic joint socket is replaced by an "artificial" one. Of the Femoral neck and the femoral head is replaced by the prosthetic part of the thigh bone (shaft) with the “artificial head” sitting on it.

Complications
What are the possible complications?
Complications are always dependent on individual components and circumstances. A hip prosthesis implantation can lead to general as well as so-called specific complications. While the general complications can appear in the context of any major surgery, the specific complications include those that are typical complications in the context of a Hip joint surgery may occur.
Appointment with a hip expert?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The hip joint is one of the joints that are exposed to the greatest stress.
The treatment of the hip (e.g. hip arthrosis, hip impingement, etc.) therefore requires a lot of experience.
I treat all hip diseases with a focus on conservative methods.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
The "typical" general complications For example, there is the possibility of blood clots forming, thus the possibility of a thrombosis, which under certain circumstances can lead to an embolism. Functional disorders in the area of the heart, the possibility of secondary bleeding in the surgical area are conceivable, and wound healing disorders or infections can never be ruled out in the operating area.
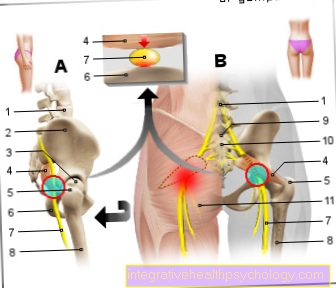
In the context of hip joint surgery, depending on the location of the operation, injuries in the immediate area, such as injuries to the sciatic nerve (= sciatic nerve) or the Femoral nerve (= Femoral nerve) can never be excluded. Due to this specific procedure, the length of the legs may change, and bone cracks or even fractures cannot be ruled out during the operation. The possible complications mentioned as examples in this section fall under the so-called procedure-specific complications.
Both forms of complication are only listed here as examples. The list does not claim to be complete.
There are various scientific studies that investigate endoprosthetic hip joint operations and possible complications. The rate of complications can vary considerably. If you look at these studies, it comes in between, depending on the investigation 3 to 30% of all endoprosthetic hip operations lead to complications.
Not only is the complication rate different, but also the type of complication. So here are the occurrences of a
- Wound infection
- thrombosis
- Pulmonary embolism or
- the inflammation of the adjacent bone tissue
called. The occurrence of a urinary tract infection (cystitis) was recorded relatively frequently, which is due to the fact that the older the patient, the greater the likelihood that one would occur after the operation Urinary catheter is / must be laid. Listed below you will find the percentage distribution of the respective complications, which have a partially different percentage distribution due to the different studies.
- Urinary tract infection / cystitis (in about 2 - 6% of cases, depending on the respective studies)
- Wound infections (in approx. 2 - 18% of the cases, depending on the respective studies, which in some cases also consider minor infections (high rate), while these minor infections are not considered in other studies (low rate)).
- Thrombosis (in about 0.5 - 5% of cases, depending on the respective studies)
- Pulmonary embolism (in approx. 1 - 3% of cases, depending on the respective studies)
- Inflammation of the bone tissue (in about 0.2-4% of all cases, depending on the respective studies)
While the above studies also include patients whose hip joint because of a Coxarthrosis was undertaken, a small national study examined only such patients. It was found that patients whose hip joint due to such Hip arthrosis / coxarthrosis was replaced have a lower complication rate. Compared to the studies mentioned above, they had a complication rate of around 8%. The complication rates including their percentage distribution are listed below. The information relates to the study and does not give any indication of possible individual forms of complications.
- Thrombosis (in approx. 2% of all cases)
- Heart problems (in approx. 2% of all cases)
- Wound healing disorder (in approx. 1% of all cases)
- Infections / problems in the kidney and urinary tract (in approx. 1% of all cases)
- Procedure-specific complications (in less than 1% of all cases: fractures / tears or damage to the sciatic nerve in around 0.5% of all cases; displacement of the replaced
- Hip joint in about 0.6% of all cases)
These complications do not indicate any long-term complications to be feared. These complications include, for example
- the non-inflammatory (aseptic) loosening of the prosthesis
- the periarticular calcification (heterotopic ossification)
As part of a so-called non-inflammatory (aseptic) loosening of the prosthesis often appear several years after the operation. There are several reasons for such Loosening of the hip prosthesis cause, however, the most important trigger is the harmful influence of the so-called Wear products of the prosthesis. Since research tries to find materials that are less susceptible to abrasion, it can be assumed that the influencing factor will continue to decrease. You can already see that modern materials such as polyethylene or ceramic sliding or metal sliding pairs minimize the influencing factor. Such a form of loosening the prosthesis is always accompanied by severe pain and can even lead to functional disorders. In such cases, the hip prosthesis is usually changed.
In general, it should be remembered that a prosthesis has a certain lifespan and that due to the inevitable material aging process with an average prosthesis age of approx. 15 years, a replacement of the prosthesis may / will be necessary. Since particularly young and physically active people belong to a so-called "risk group" for a loosening of the prosthesis, explains the reason why one should carefully weigh the advantages and disadvantages of an artificial hip joint, especially in this patient group.
Of course there are other “risk factors” for the possibility of the loosening of the prosthesis. For example, being overweight is certainly a part of some patients, as the new hip joint is immediately asked a lot in this individual case.
The periarticular calcification (heterotopic ossification) is a special form of complication in the context of hip arthroplasty. This is understood to mean foci of calcification in the area of the soft tissue (the muscles), which appear a few weeks or months after the operation. These calcifications are new bone formation in the immediate vicinity of the operated hip joint, which - depending on the individual situation - can lead to severe pain and even restricted movement, which the operation actually wanted to remove.
It has been found that one is this periarticular ossifications (heterotopic ossification) by the administration of an anti-inflammatory drug, usually by the administration of Indomethacin, dicolofenac or Ibuprofen can prevent.
Alternatively, it is possible to treat with the help of a single hip joint radiation treatment. The dose of 7 Gy has proven its worth. On the one hand, irradiation can be used prophylactically, but on the other hand it can also be used when calcifications have already occurred.
Irradiation can also be considered prophylactically, especially if the patient is classified as a so-called “risk patient” with regard to the occurrence of periarticular ossification. This includes, for example, patients who already had such a form of calcification after an earlier operation or patients who suffered from particularly severe mobility restrictions prior to the operation (e.g. ankylosing spondylitis) Even patients with extensive tissue damage are considered so-called "risk patients".
If prophylaxis is used, the risk can be considerably reduced. The literature describes a reduction in the risk from approx. 80 to up to 10 percent.
Lunar cycle and complication
Author's note:
A question about the influence of the moon on the complication rate was investigated by an Austrian team. This study came to the clear result that the lunar cycle has no influence on the complication rate.
Loosening of the hip prosthesis
Not least because of the high life expectancy is now a Replacement operation of the hip prosthesis quite common. Thus, the replacement operation after loosening the prosthesis is not uncommon, although it is always to be classified as complex and sometimes technically very difficult to carry out.
In contrast to the first operation, the loosened prosthesis must first be removed. This means that a stage must be established which enables a new prosthesis to be anchored in the bone again at all. Depending on the individual circumstances, this can lead to major bone defects, which then either with body's own bone from other parts of the body, with Replacement bone from the bone bank or with cement fill out.
Which method is used in each individual case depends on the individual circumstances and is ultimately up to the decision of the doctor who performs the replacement operation. The decision, however, depends to a considerable extent on the age of the patient, his mobility and the quality of the bone.
Should the case of a very thin or one by an advanced stage of the osteoporosis If the bone is weakened, the surgeon can additionally reinforce the shaft of the thigh with a plate (stainless steel or titanium). This measure increases the resistance and resilience enormously.
You can find more information under our topic osteoporosis.
As already described in the context of hip arthroplasty, a replacement operation also carries the risk of high blood loss. Since this is a planned operation, there is an option to have one some time before the planned operation Autologous blood donation to undertake. This has the advantage that there is no need to resort to foreign blood.
So-called also appear more and more frequently Retransfusion systems are used, which work up the blood from the wound directly and can be returned as blood from the patient's own blood.
The question of how often you can carry out a replacement operation cannot be answered in general at this point. The given, individual factors must always be taken into account.
However, there is one thing that you should always be aware of: with each replacement operation, it becomes more difficult to anchor the prosthesis firmly in the bone.
Special prostheses should be mentioned at this point, which the operating doctor can consider if a firm anchorage in the bone is hardly possible.
In very difficult cases where the loosening of the prosthesis has occurred, it can also happen that the loosened prosthesis is completely removed and initially not replaced. One then speaks of the creation of a so-called Girdlestone situation. It depends on the individual case whether another hip joint will be installed in the future or the one mentioned above Girdlestone situation is retained.
Hip prosthesis pain
Usually it comes with the insertion of a Hip prosthesis very rarely to complications. In exceptional cases, however, an allergic reaction in the surrounding tissue can occur. This is a defense reaction of the body to the inserted foreign body, which leads to pain in the patient.
It can also cause inflammation, causing severe pain. This can be triggered by bacteria directly after the operation or after some time.
During the operation, nerves or blood vessels can be damaged, causing pain. This is one of the risks of any operation, but it happens very rarely.
Some time after the hip prosthesis has been inserted, calcifications can develop on the bones, which are expressed in pain and often in the resulting relieving postures. Overloading a hip prosthesis through being overweight or moving a lot can also lead to pain. This often leads to a Loosening of the prosthesiswhich is initially noticeable as pain in the buttock region of the groin and thigh. In the further course, the pain intensity increases and leads to restrictions in mobility.