Mole
Synonyms in a broader sense
Birthmark, Mal
Medical: nevus, nevus cell nevus, nevus pigmentosus, junction nevus, compound nevus, dermal nevus
English: liver spot, beauty spot
definition

A “mole” is generally referred to in medicine as a nevus (= Mal, plural Nevi) and describes a locally limited malformation of the skin, which is characterized by an increase in pigment cells, so-called nevus cells. These are probably genetically modified pigment cells (melanocytes).
A distinction is made between congenital (occurring at birth or within weeks) and acquired mole. Each of these forms can still be divided into junction, compound and dermal nevi organize.
Epidemiology / incidence / frequency
The mole is one of the most common skin changes.
Congenital forms are less common than acquired ones. In newborns, the incidence is about 1: 100; Larger birthmarks in babies are even less common (1:10 000-500 000).
A familial accumulation of congenital moles has been described. Men and women are equally affected.
The acquired mole as a more common form occurs across all ethnic groups, but more often in the white population than in the more pigmented. On average, each person has about 30 acquired ones Nevus cell nevi, Men show a little more than women. The mole forms primarily on parts of the body exposed to light and reaches its greatest extent in the 3rd and 4th decades of life. Then he regresses.
In principle, they all represent the precursors of skin cancer (malignant melanoma), but the degeneration is very rare and the exception. Only the congenital liver spots and the "Clark nevi", a special form of acquired nevi, show an increased risk of degeneration.
causes
The genes play a role in the acquired mole. In addition, sex hormones and UV light.
According to current theory, it is assumed that the nevus cells that form the mole develop from defective pigment cell precursor cells, the nevomelanoblasts. These colonize in the course of the Embryonic development the skin.
In the upper layer of the skin they either multiply in the womb and thus form the congenital nevus cell nevi or they first rest there and multiply in the course of life, which in turn leads to the acquired form.
Both forms of Mole go through a stereotypical path of development. First, they are as Junction nevus before, then develop into one Compound nevus and ultimately develop into a dermal nevus. These shapes reflect the gradual migration of the firmly adhering nevus cells from the surface of the skin downwards.
As a rule, the congenital mole the nevus cells in deeper layers than in the acquired mole.
Symptoms
The acquired Mole offers a morphological diversity.
What they have in common, however, is that they are small (less than 5 mm in diameter), round, not very sharp and not excessively pigmented. In addition, they usually fit well and homogeneously into the surrounding area skin a.
Depending on the stage of development, the mole presents a slightly different picture. In the first stage - as Junction nevus - it looks small and flat. The color varies from light to dark brown; reddish forms also exist. Furthermore own Junction nevi often a granular surface.
Coumpoundnävi on the other hand, the next level, are larger, more raised and knotty, but also homogeneous. The color is light - to dark brown. Hair is also often found.
Finally, the last stage, the dermal nevus, usually only occurs in the second half of life. Compared to the forerunner species, it is more prominent and meatier. The hemispherical shape is smooth and possibly hairy.
Congenital moles, on the other hand, are larger, usually 1 to 3 cm, and are deeper than the acquired ones. Their round to oval shape is well defined, homogeneous, knotty and brown to brownish-black, whereby they become darker over time. They often have hairiness.
Furthermore, they show less spontaneous regression.
Other malformations that do not affect the skin also occur in around 10% of those affected, for example the eyes, Ears or on the skeleton.
Even less often there is one at the same time Neurofibromatosis (Hereditary disease with, among other things, neoplasms annoy) or involvement of the meninges before (Colonization with nevus cell nevi).
A special form of acquired liver spots is the Clark nevus this one is bigger (larger than 5 mm), round, flat and centrally darker and raised. Partly or completely they are reddish, the border blurred.
Mole itches
If a mole is itchy, it can have several causes. There is not always something dangerous behind it, but if the symptoms persist, a professional should be consulted. Under no circumstances should an itchy mole be scratched, as it can subsequently become inflamed and possibly degenerate.
One possible cause for the itching can simply be very dry skin or mechanical skin irritation. Just as other areas of skin can itch in this condition, so can liver spots. In this case, the symptoms usually subside by themselves within a few days. A fat cream can be used as a support.
Inflammation or infection of a mole can also cause the annoying, itchy feeling. But even here it is important, if possible not to scratch! Is it a eczema if you have an allergic reaction, for example, you should see your dermatologist for a ointment containing cortisone to be able to apply to the mole.
In addition to these rather harmless causes, itching can also be a warning sign of malignant skin cancer. The itchy feeling arises as a reaction of the surrounding tissue to the change or degeneration of the mole. Especially if there is burning or stinging in addition to the itching, this should definitely be further clarified by the specialist.
Sudden bleeding without scratching is also very suspicious.
It is important to see a doctor as early as possible in the course of the process, as this is important for the prognosis Skin cancer Starting therapy as early as possible with the early removal of the degenerated mole is of essential importance. In addition, itchy moles that have long had to grow deep into the skin have an increased likelihood of metastasis (scattering) cancer.
diagnosis

The diagnosis includes the clinical appearance. Incident light microscopy is helpful here. This means looking at the mole with a magnifying glass using a dermatoscope.
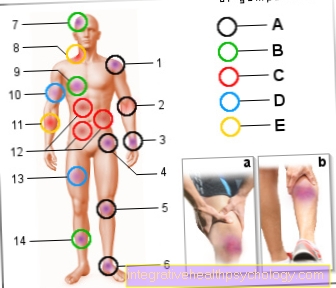
The so-called ABCD rule is used in the assessment, which can be used to distinguish whether a benign nevus or a tumor (Melanoma) is present.
The letters stand for "Asymmetry", "Limitation", "Colorit" and "Diameter".
The benign mole is symmetrical, sharply defined, homogeneously pigmented and smaller than 5 mm.
However, this rule is only an aid and approximation of the differentiation; a proof of goodness or badness does not succeed.
Upon removal, a histological (= microscopic) Examination of the material so that the diagnosis can be made with certainty.
treatment
Moles can be removed using a variety of methods.
A dermatologist can use a biopsy to determine whether this also makes sense in individual cases (Tissue extraction) and depends on the findings. For example, if it is a harmless mole, its removal is not necessarily indicated from a medical point of view. But becomes more malicious with the sample taken Skin cancer (Malignant melanoma) it is advisable to have the mole removed to prevent further spread of the disease. In this case, the mole should be surgically removed generously and with a certain safety margin. (please refer: Mole and skin cancer)
Other methods like that Laser process or a special light method are used purely to remove moles from a cosmetic point of view. No statement can be made about the malignancy of the liver spots because the tissue is irreversibly destroyed and it is no longer possible to remove tissue from this area. Any degeneration of the affected mole must therefore be ruled out in advance.
With the laser procedure, the area is first disinfected and a local anesthetic is applied. The laser beams then penetrate the top layer of skin and produce heat in the process.
This heat energy destroys the too much melanin that has formed in the mole, the substance that is responsible for the dark color. Since the laser beams can be applied very precisely, the surrounding tissue is not damaged. Immediately after the treatment, the mole often looks a little darker than before, but scabs after a few days and then heals without any problems. Overall, the laser process is a very gentle method, which is good but also only suitable for cosmetically disturbing moles.
The method with light is the IPL method with intensely pulsed light. The principle works very similar to that of laser beams, namely that high-energy light destroys the melanin in the top layer of skin and thus makes the mole optically disappear.
The cells of the surrounding skin tissue are not damaged. This method is also only suitable for the treatment of cosmetically disturbing liver spots, not for the treatment of degenerate liver spots, since the depth of penetration of these light rays is not deep enough.
Malignant liver spots should always be removed surgically. After sufficient disinfection and anesthesia of the operating area, the mole is cut out with a scalpel with the necessary surrounding safety margin.
Small incisions do not require a suture, but if a slightly larger mole and surrounding structures are removed, a few stitches may be necessary.
Very small moles can also be punched. The patient himself usually does not notice this procedure and can go home immediately after the treatment. An inpatient stay is usually not necessary for this. The only thing that should be done in the following two weeks is not to exercise, and to avoid movements that put a particular strain on the operated skin area. It should also be sufficient Wound hygiene be respected.
Under no circumstances should moles be cut out independently. On the one hand, this can lead to cosmetically very ugly scars, but the area could also become infected and lead to further associated complications. Both the final assessment of malignancy and the removal of moles should always be left to a specialist, i.e. an experienced dermatologist.
Remove the mole
Moles have a very low risk of degeneration and therefore generally do not pose a health risk.However, as soon as it is suspected that the mole could be malignant and that it could develop into skin cancer, it should be removed. There are several methods for doing this.
- Surgical Removal: The removal of liver spots using a scalpel, so the Excision (Excision = cutting out) is a very often used method, as you can then send the suspicious skin area to a laboratory and thus obtain evidence of whether it was actually a malignant mole.
The procedure for surgical excision is as follows: The area to be operated on generously disinfected to prevent inflammation of the wound. Then the skin is treated with an anesthetic (Local anesthetic) injected under. This has two functions. On the one hand, the area is numbed and the operation can be performed painlessly. On the other hand, the mole lifts up through the injection of liquid and can thus be removed more easily. When the local anesthetic works, the mole becomes cut out with a safety margin of a few millimeters. The dermatologist will ensure that the entire nevus is reached in depth. After that the wound sewn up depending on size. After one to three weeks, the stitches can be pulled, then the treatment is over. Usually a small scar remains. - Especially when a mole is being removed for cosmetic reasons only, patients want to avoid the surgical method as it will almost certainly result in a scar. You can get the mole too through laser treatment remove. This method is suitable primarily for cosmetic interventions, because the mole is destroyed and no material can be obtained for a laboratory examination (no prognosis for possible malignancy). During laser treatment, the Skin not opened, the risk of wound healing disorders and inflammation is minimized. In addition, there is usually no or very little scarring. One disadvantage, however, is that high costs for the procedure, which is almost never covered by health insurances. There is also a small risk that the mole has not been completely removed and therefore grows back.
Laser mole
The laser procedure for removing liver spots is only used if the removal is purely for cosmetic reasons.
It is by no means suitable for treating malignant changes, as tissue removal for further diagnosis is no longer possible with this method. The irradiated tissue is irrevocably destroyed and can no longer be used for assessment.
But if a malignant change is definitely excluded, the mole to be removed is first anesthetized and then irradiated.
The result is not always precisely predictable. It may be that the mole disappears almost completely, but it can also sometimes be that it only fades a little or even reappears after a while.
Good and comprehensive advice from a specialist is therefore particularly important for exposed parts of the body such as the face. Possible complications with this method are Scarring, a local burn or other tissue damage or nerve damage that can lead to abnormal sensations in the affected skin area.
An infection following the treatment is also conceivable, although an ointment containing antibiotics is usually used prophylactically. It is therefore important to have laser treatment carried out only by an experienced specialist and, if possible, in a dedicated center in order to prevent further complications as far as possible.
Mole scratched
Is a Mole scratched it usually bleeds and incrustations appear which can initially look very threatening. Usually these are protruding moles that have been accidentally injured by mechanical stress. This is usually not dangerous and heals this skin area by itself with a little protection.
However, if the injury triggers fears in the person concerned, it is advisable to consult a dermatologist.
The situation is different with liver spots, which itch constantly or are located on parts of the body that are exposed to increased friction, for example the soles of the feet. If these moles are scratched open frequently, their removal should definitely be considered, as chronic stress can lead to inflammation.
This, in turn, could encourage further degeneration of these moles and, in the worst case, lead to malignant skin cancer.
These moles should therefore be clarified immediately by a doctor.
Mole in the eye
Moles can appear on and in the eye just like anywhere on the body.
Are you on lid or in the iris (Iris) they can also be visible from the outside, whereas moles in the choroid membrane, i.e. inside the eye, can only be diagnosed by an ophthalmologist.
However, moles in the eye are not uncommon and, unless they degenerate, are just as harmless as anywhere else on the body. They should only be checked by an ophthalmologist at regular intervals and removed if necessary in the event of malicious changes. Both the surgical method and radiation or laser methods are used for this, which should be discussed with the treating doctor in each case.
But moles on the eye can also be operated on for cosmetic reasons, for example if they are very large, are perceived as annoying or even restrict the field of vision. These interventions are usually carried out in general anesthetic and a short inpatient stay is therefore recommended.
The mole is bleeding

A mole can also bleed and become infected if it is exposed to constant stimuli due to its anatomical location. This is the case, for example, on the sole of the foot; constant pressure can cause the mole to bleed and crusts.
You should remove a mole on awkward parts of the body. In general, a mole could turn into black skin cancer. Black skin cancer is easy to cure, but only if it is detected early, so you should see a dermatologist regularly and get skin cancer screening done. Screening is recommended every two years. Between visits to the doctor you should pay attention to your moles yourself, using the ABCD rule you can quickly see whether the mole is benign or malignant:
- A = asymmetry, the melanoma grows asymmetrically, not round or oval.
- B = limitation, melanomas grow frayed, fuzzy and jagged.
- C = coloring, different colors within the mole indicate melanoma.
- D = diameter, noticeable growth is a sign of malignancy.
If there are signs of melanoma according to this rule, you should see a dermatologist as soon as possible and have a screening carried out. This will cut out the suspicious mole. If it turns out that it is a melanoma, depending on the size and condition, further therapies are initiated. In addition to regular skin cancer screening, you can prevent melanoma by protecting yourself adequately from the sun's UV radiation. Here it is important to apply sun protection cream with a high sun protection factor, especially for light skin.
Children's skin in particular needs to be protected; toddlers in their first year of life should not be exposed to the blazing sun at all. In addition to these influenceable factors, there seems to be a genetic component for the degeneration of liver spots; melanomas occur more frequently in certain families. If close relatives are already suffering from melanoma, you should be particularly careful and seek advice from a dermatologist.
Read more on this topic at: Bleeding mole
Mole inflamed
Should be a Mole ignite or a red border forms around it, this can be due to different causes.
These can be more harmless processes, such as an allergic reaction or infection.
However, permanent inflammation can also lead to cell degeneration, which in the worst case can become malignant Skin cancer (Malignant melanoma) can lead. An inflamed mole should therefore be further clarified by a specialist if possible in order to safely rule out dangerous causes.
Accompanying symptoms such as pain, stinging, itching or bleeding should be recognized as warning signs of possible degeneration and reported to the doctor immediately.
prophylaxis
For prevention of the acquired Mole it can help to avoid UV light, as it is also caused by sunlight.
There is no prevention of congenital moles.
forecast
The prognosis of the acquired form from Mole is good, as these only very rarely degenerate and in most cases are benign in nature.
Offer an exception Clark nevias they are more common in Skin cancer pass over and thus have a worse prognosis than the other acquired moles.
Even for the congenital forms, the degeneration rate is higher and the prognosis is slightly worse, but with regular monitoring, it is likely that skin cancer will be detected in the early stages and the chance of recovery is good.
Summary
Everyone doesn't have just one Mole, distinguishing congenital from acquired forms.
The congenital shape of the mole should be controlled more closely by observation than the acquired one in order to recognize possible degeneration early and to initiate removal. The acquired Mole is usually harmless.













.jpg)