Pneumonia in the baby
introduction

Pneumonia is an inflammatory disease of the lung tissue and is also known as pneumonia. It is one of the most common diseases of the respiratory system in childhood. It can be triggered by different pathogens. The time of the infection also plays a role for the course, but also for the identification of the pathogen. The baby can be infected as a newborn immediately at or shortly after birth or in the following weeks and months. Since the baby's immune system is constantly maturing, but is also initially supported by antibodies from the mother (so-called maternity protection), the phase in which the baby is infected is extremely relevant. An estimated 150 million children worldwide develop pneumonia each year. 2 million of these children die from pneumonia, but developing countries in Asia and Africa are driving these numbers up.
In addition to the age of the patient and the pathogen strain, pneumonia can also be subdivided according to where it occurs. A distinction is made here between pneumonia acquired on an outpatient basis and infections that have arisen nosocomially. Outpatient means that the baby was infected with a pathogen outside of the hospital in its natural environment. Nosocomial is another term for "hospital acquired". Infections acquired in the hospital are usually less favorable, as the child is often admitted to the hospital because of another illness and the immune system is thus additionally weakened.
Read more on the topic: Nosocomial infection
Risk factors
Several factors can increase a baby's risk of having one pneumonia to develop. One can distinguish those factors that increase the risk of infection from those that negatively affect the defense against pathogens. Basically one increases bad environment the risk of disease. This means that babies and children with socially disadvantaged backgrounds are more likely to be sources of danger like hygienic deficits, unhealthy diet and maybe Passive smoking are exposed. The maturing one lung cannot cope with such circumstances and gets sick. Malformations of the respiratory system, one congenital immunodeficiency, bronchial asthma, Heart defect, but also acquired infections with viruses causing a systemic disease (for example measles) can promote the occurrence of pneumonia.
The longer a hospital stay, the greater the risk of nosocomial infection. If the baby has to be ventilated because his condition leaves no other option, the risk of pneumonia increases again.
root cause
Outpatient acquired pneumonia is common in babies and young children Mixed infections from bacteria and viruses. A bacterial infection is often preceded by a viral upper respiratory tract infection. About a quarter of all pneumonias are viral, and the younger the patient, the more likely it is that viruses have caused the pneumonia. 80% of illnesses in children between 2 months and 2 years of age have a viral cause. The Respiratory Syncytial Virus (RSV), Influenza- and Adenoviruses on. Other viruses that can cause pneumonia include the following: Rhinovirus, Enteroviruses, Varicella zoster virus (chickenpox), Epstein-Barr Virus, various Herpes viruses, of the Cytomegalovirus (CMV) and Measles virus.
The most important bacterial pathogens, which, however, only play a greater role in advanced childhood, are Streptococcus pneumoniae, Mycoplasma pneumoniae and Chlamydia pneumoniae. The former poses a health threat to all child age groups because it is very common.
Of all ages of babies and toddlers the must have neonatal (neonatal = newborn) pneumonia differentiated and viewed most sensitively. The child can develop pneumonia within the first three days shortly after birth Neonatal infection train or only after several days. The time it takes for the disease to break out depends on the length of the cycle the pathogen has to go through. The division of the transmission mechanism is based on the delivery. The pathogen can pass through the fetal lungs aspiration (Inhalation and swallowing) infected amniotic fluid and through Pathogen in placental blood transmitted before birth.
After the birth, there is the possibility of infection directly during the act of delivery through pathogens in the woman's birth canal, but also after delivery nosocomially by the mother or the staff. For example, are transmitted in the mother's womb rubella, CMV, Treponema pallidum and Listeria monocytogenes. Perinatal (“during childbirth”) are Streptococci (Group B), Escherichia coli, Staphylococcus aureus and Klebsiella important species.
In addition, atypical pathogens or Mushrooms be the cause of pneumonia. With today's standards in the industrialized countries, however, this is very seldom the case and represents a medical rarity. If the child is not immunocompromised, an outbreak almost never occurs in normal surroundings. Small-scale outbreaks of this type only occur in countries in which hygiene standards and medical care are extremely poor. Fungal species that break out in such areas are for example Histoplasma capsulatum and Coccidioides immitis.
Signs (symptoms)
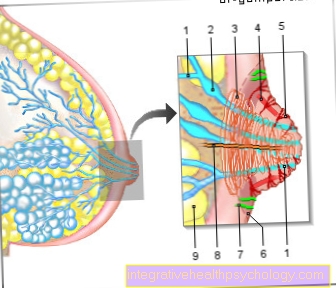
In babies, the most typical form of pneumonia is one Bronchopneumonia. Not only are deep parts of the lungs affected by the inflammatory infection, but also the bronchi, i.e. higher sections. The inflammation is limited in contrast to the Lobar pneumonia, which is the main form only from older children, not only on one flap, but also forms several foci of inflammation in the entire lung or in the entire lung. The pathogens spread in a circle from the bronchi into the lung tissue.
The Signs pneumonia can vary greatly between babies and young children. Often the disease is just getting started recognized latebecause no symptom construct can be put together to form a uniform clinical picture. In addition, a distinction must be made between various pathogens that have specific differences in the symptom structure that they cause.
There are several signs that one can look out for that are more common in bacterial pneumonia. The general condition of most patients, whether young or old, is reduced and a feeling of illness is described. This can affect babies constant screaming, but also through extreme drowsiness (lethargy) demonstrate. The child very likely has high fever and coughs. In the event of a febrile infection without a known origin, pneumonia should always be excluded in childhood. In addition, the principle applies that there is a bacterial cause behind a high fever. Breathing is also severely restricted - breathing pauses and an increased breathing rate (Tachypnea) are signs of a bacterial pneumonia in infants. In newborns there is often one in addition to pneumonia sepsis, one Blood poisoning. Masses of bacteria can be detected in the blood. The skin of the baby is pale and in addition to the lung problems there is an increased one Heart rate (Tachycardia) and a decreased desire to drink.
If pneumonia is suspected, the seasonal activity of various respiratory viruses should always be included in the diagnosis. A viral infection is then much more likely than a bacterial one, especially in babies and toddlers. Important with one viral pneumonia is that the clinical picture in most cases without a fever represents. It comes to noticeable Retraction in the chest area. This means that the tissue between the ribs sinks in during the breathing process. This is a sure sign of a complicated and clear one restricted breathing, as well as that Overinflation of the lungsthat occurs in affected infants. The pulmonary alveoli are greatly enlarged in representations of imaging procedures.
What are typical signs of pneumonia in babies?
An infection in the baby shows up Not in the same way as in the adult. Often times, there are other signs that indicate infection, such as pneumonia.
There are also differences depending on how old the child is. In newborns, the signs of pneumonia can be great unspecific be. The babies can get through Unwillingness to drink or Refusal to eat stand out. Also a apathetic behavior can be an indication of pneumonia.
High fever such as to cough are typical, but the latter in particular is extremely rare in babies. A increased heart rate (tachycardia) is also a sign of pneumonia in babies, but it must be said that the heart rate in newborns and babies is anyway higher than it is in adults. Pneumonia in babies is also typical Breathing disorders like that Nostrils. This is the erection of the nostrils when you inhale, which widens the airways.
Also one shallow and rapid breathing may indicate pneumonia.
Temperature fluctuations are also possible. A Blue discoloration of the mucous membranes and the skin indicates a decrease in oxygen saturation in the arterial blood and is also typical of pneumonia in babies. When exhaling, a so-called "Knorksen" be heard, which occurs when breathing difficulties in the context of pneumonia.The "creaking" also occurs during the normal breathing process, especially in premature babies, and as such is not yet a sound indication of pneumonia.
You might also be interested in: What to do if your baby has a fever
How contagious is pneumonia in babies?
The risk of contracting pneumonia in the baby depends on the baby Type of pathogen as well as the immune situation of the contact persons.
Most of the pathogens (bacteria and viruses) that cause pneumonia are caused by the Sneezing and coughing transfer. However, many of these pathogens are not so dangerous for adults because they have formed a large number of antibodies in the course of their lives. The natural immune system can thus protect itself against the germs, so that pneumonia in adults or older children usually does not occur.
However, other babies are at risk of becoming infected because you Immune system not yet fully developed is. Therefore, infectious diseases infants should not come into contact with healthy infants. The Risk of contagion is here relatively high. General statements cannot be made, however, since the risk of infection varies from pathogen to pathogen.
You might also be interested in: Herpes in babies - how dangerous is it?
Pneumonia in the baby after birth
Pneumonia in the baby can also be immediate after birth occur. It is a so-called Neonatal infectionwhich have different causes.
As part of a Amniotic Infection Syndrome the baby can already be infected with germs in the maternal uterus. The pathogens usually rise from the maternal vagina into the uterus and lead to an infection there. When the child is born it can be so within the first 72 hours of life to symptoms like Fever, apathy, unwillingness to drink, difficulty breathing and Circulatory disorders come.
Mostly these are bacteria, which are known as Group B streptococci designated. In principle, any organ can be affected by such an infection, but pneumonia is common. In any case, there is an immediate intensive medical care of the baby and immediate antibiotic therapy, as otherwise serious, life-threatening consequences can result. Even after the first 72 hours of life, an infection can develop, leading to pneumonia. There are very many risk factorsthat promote pneumonia such as complications during childbirth, wounds on the child, medical measures such as inserting catheters or accesses in the blood system and much more.
You might also be interested in: Fever baby
Diagnosis

The diagnosis of pneumonia in babies or toddlers can be very difficult. The age of the child, the geographical location of the place of infection and the time of year must be taken into account when identifying the pathogen. The examination of a blood culture is the method of choice in adults, but often does not lead to a positive result in young children. The blood can still be checked for its inflammation parameters and for the white blood cell count. Although this gives indications of an infection, it does not say anything about where it is located. Finally, to identify the pathogen, a PCR, one Polymerase chain reaction, be performed. Specific components of the pathogen genome are reproduced and then detected.
sputum, a sample of the mucus that is ejected, is difficult to get from babies because they are not yet able to react randomly to instructions. Other methods that are used in older patients are too dangerous for babies and do not achieve a satisfactory level of risk-benefit ratio. Thus also falls Decrease in bronchoalveolar lavage (Withdrawal of fluid from the alveoli) or a Lung puncture (fluid is removed from the lungs from the outside with a long needle). While a smear of the nasopharyngeal secretion (smear of the secretion of the pharynx) is already useless in school children, it is excellent for infants to get information about the pathogen. Often times, pneumonia in babies is caused by a superinfection of the respiratory system. The viruses first settle in the patient's throat and then migrate downward into the lower parts of the lungs due to the deficient immune system.
Imaging procedures are not used as an initial diagnostic measure due to the radiation exposure. If the patient shows no reaction to an existing antibiotic therapy, if the course is atypical or particularly difficult, then it is usually within the scope of damage limitation Chest x-ray (Chest) performed. The typical for babies and young children Bronchopneumonia appears in the picture as all-over lightened change This is done by the infiltrate, which is located in the lung tissue and also makes it impermeable to X-rays. A rare one in babies Lobar pneumonia is limited to what is shown in the picture as a rag sharply delimited brightening represents. The benefits of X-ray diagnostics are controversial. The child is stressed by the radiation and in the end the picture often gives no indication of the pathogen.
Shadows in the image can lead to a confirmation of suspicion, but can also be misinterpreted. This increases the rate of unnecessarily prescribed antibiotics. An alternative to the X-ray is the Pulmonary ultrasound dar - the ultrasound scan of the lungs. Superficial foci of inflammation can be identified more specifically as such and pleural effusions, which arise in the context of pneumonia with pleural involvement (pleura = pleura), are more easily recognized. Sonography is clearly inferior to X-ray when it comes to deeper-lying inflammations.
treatment
When deciding how and where the child should be treated, the severity of the baby's pneumonia plays a decisive role. Is it a light or moderate infection, the baby can be outpatient, so treated at home become. The criterion of Hypoxia, of the decreased oxygen levels in the blood, decide on one Hospitalization. A sufficient supply of oxygen to the organs must be guaranteed in order to protect the infant from permanent damage. Will in the child severe shortness of breath noticed, the speed of breathing is permanently increased or it is more dangerous because of the disease Restriction of drinking behavior, the child should also despite adequate oxygen saturation stationary be included. It is always advisable to opt for hospitalization for newborns and babies up to 3 months of age.
Treatment of pneumonia in babies may involve the use of Antibiotics support or optimize it. Since the latter should be aimed for, the child's condition can be positively influenced. If the oxygen saturation is below 93%, the patient must wear oxygen glasses or, if the nose is relocated, a mask or a Head box, be ventilated. Because of the fever and the rapid breathing extremely passed a lot of fluids some babies get into a state of Dehydration. This must be done by means of a Nasogastric tube or one infusion be counteracted. The feeding tube should be as small as possible so as not to restrict breathing any further. When giving infusions, the Electrolytes controlled in the infant's blood to maintain balance. Painkiller can increase the child's will to move. This helps in coughing up accumulated secretions and can promote the course. A antipyretic therapy alleviates the patient's suffering, but has no therapeutic effect on pneumonia per se.
The right antibiotic must be selected based on age and the pathogen. Since, as a rule, drug therapy is not waited until the pathogen has been detected, the choice of drug is based on geographical and seasonal concentrations, as well as on the standard pathogens for pneumonia in infancy. Attention must be paid to any existing penicillin allergy that requires the use of other groups of antibiotics. Oral administration of the medication should always be aimed for and the duration should be 7 to 10 days. Viral therapy is usually limited to treating the symptoms. The use of antivirals is almost never necessary. In a proven influenza pneumonia can be different Neuraminidase inhibitors may be resorted to, however, infection with a annual vaccination be bypassed. Fungal infections are through Antifungal drugs treated, however, sometimes have considerable side effects even in adults. Drug treatment of pneumonia should therefore always be carried out under the supervision of a specialist.
Read more on the topic: Vaccination against pneumonia
When does pneumonia in babies become dangerous?
Pneumonia in babies is always one serious illness.
Infants always will stationary treated as they fight germs Antibiotics by vein get administered. It must also be the condition of the baby closely monitored so that no complications arise.
Should a baby be noticed by one changed behavior like for example Reluctance to drink, lethargy or one quick and shallow breathing, it is essential to consult your pediatrician at an early stage. Symptoms like Cough, nostrils, a distended stomach or one general restlessness of the baby can indicate pneumonia.
If you have pneumonia, you must immediately get a therapy can be initiated, so it should not be long before a pediatrician is visited. If pneumonia is suspected, he will immediately refer the baby to a clinic, which can take appropriate action. In Germany the treatment options are very good, so pneumonia in babies is usually within one to two weeks heals without consequences. Since pneumonia has serious complications such as a Sepsis (blood poisoning) medical care of the baby is essential.
Read more on the topic: Blood poisoning in children, Bacteria in the blood - how dangerous is it?
forecast
Basically, pneumonia does not have to be dangerous for a baby. With medication and other therapy, there is a clear improvement within the next 2 to 3 days. The child's exhaustion is slowly disappearing, but there is one general weakness not uncommon in the period after recovery. This too will pass with complete restoration of physical vitality.
Dangerous for the baby can Complications favored by the existing pneumonia. This includes, for example Pleural effusion. If the inflammation spreads to the baby's lungs, the Pleura (Pleura) also inflamed (pleurisy). Not only does this cause pain when you breathe, but it can also cause pain Fluid build-up lead in the pleural space. The liquid can be composed of inflammatory infiltrate and / or blood. Due to the volume that the liquid takes up, the baby's lungs are increasingly deprived of space for complete expansion and breathing continues to be restricted. Another complication is one Lung abscess. A focus of inflammation is encapsulated, which can make existing drug therapy ineffective. Most abscesses drain into the bronchi during the healing process and do not require an operation.
prophylaxis
The pathogens that can cause pneumonia in babies are mostly transmitted via droplet and smear infections. Depending on the strain, they are highly contagious and easily transmitted from infants through oral restraint. The risk of infection can be reduced through preventive measures. This includes proper hand hygiene and all other conventional hygiene Hygiene measures. In addition, a vaccination against the most important classic pathogens - Haemophilus influenzae type B, Bordetella pertussis and Pneumococci - be performed. A vaccination against influenza viruses is necessary every year because the strains are very versatile. A one-time vaccination does not prevent you from being infected the following year. Every child should also be vaccinated against measles virus, which can also cause pneumonia in babies. The vaccination coverage, however, leaves a lot to be desired worldwide and also in Germany. Children belonging to special risk groups should always be given all possible protective measures. For example, here is one Administration of RSV-specific monoclonal antibodies possible. However, the antibodies only protect the patient temporarily.