Periodontal disease and periodontal disease
introduction
Periodontics is a relatively young branch of dentistry. It deals with the causes, course, prophylaxis and therapy of diseases of the periodontium. Today it is an independent subject, after having previously been part of the conservation department.
The term periodontal disease is incorrect and out of date. The term "periodontitis" is correct.

History of periodontal disease
In the media and in advertising, periodontosis is unfortunately still spoken of and the term is popularly known. This term, which was originally introduced for all periodontal diseases, has become firmly established over the years and has become an integral part of the vocabulary.
From a medical point of view, however, periodontal disease describes a form of diseases of the tooth supporting system that does not exist in reality. There is no such thing as periodontal disease, but periodontal disease. It is by far the most common of all periodontal diseases. So whenever periodontosis is mentioned, periodontitis is meant.
Why is there a need for discussion because of these different word endings? Periodontitis and periodontosis are two very different diseases that have different causes, courses and therapies.
While dentists used the term periodontal disease until the second half of the 20th century, it is now clearly certain that there is no such thing as periodontal disease and instead it is called periodontal disease. Therefore, the term should not be used in advertising or by patients or (dental) medical staff.
"Periodontal disease"
The outdated term periodontosis, as can be seen from the ending -ose, is a progressive, degenerative process without inflammation. However, since in reality there is no periodontal disease without an inflammatory cause, the term periodontal disease no longer makes sense.
In medicine there is constant further research, so that one often has to discard accepted theories when new scientific findings have emerged; so also in the case of the alleged periodontal disease, which is actually periodontal disease.
Periodontal disease
The ending –itis in periodontal disease shows that it is an inflammatory process. Colloquially, periodontitis can be referred to as inflammation of the gums or gums.
Gingivitis, or inflammation of the gums, can develop into periodontitis without treatment. The fundamental difference between inflammation of the gums, in which no permanent damage to the periodontium is to be expected, and periodontitis is the irreversible breakdown of bone that occurs in periodontitis.
If the inflammation starts from the gumline, it is called Marginal periodontal disease designated. Bacterial plaque that has not been removed for more than 2 weeks leads to local inflammation on the gum line. The bone resorption usually takes place horizontally.
In contrast to this, periodontitis can also start from the tip of a nerve tooth, which is then referred to as Apical periodontitis. In this case, the bone is broken down vertically.
The bacterial plaque is always responsible for the inflammatory reaction. The bacteria contained therein trigger an inflammatory reaction in the tissue, which without treatment progresses further and further towards the tooth root and finally also affects the jawbone and leads to its progressive destruction. The breakdown of bone and loss of the connective tissue that anchors the tooth in the tooth socket leads to the loosening of the tooth and even tooth loss.
Now the importance of the correct term for inflammatory-destructive periodontal disease becomes clear: inflammatory stimuli from dental plaque that has not been removed cause the disease. The risk of developing periodontitis drops rapidly with correct and regular teeth cleaning.
The dentist will be happy to demonstrate and explain the correct brushing technique to you.
Also read: Proper dental care - find out more!
Symptoms of Periodontal Disease
The symptoms are clear. When brushing your teeth or spontaneously, there is bleeding gums, but not always pain. At this stage there is no periodontal disease, but rather gingivitis. Without treatment, bacteria invade the tooth socket and destroy the fibers that connect the tooth to the bone.
These are so-called facultatively living bacteria, i.e. the pathogens can exist both in the presence of oxygen and in the absence of oxygen. Besides other bacteria, the A. actinomycetemcomitans plays a crucial role. The swelling of the inflamed gums creates gum pockets in which food residues and plaque collect.
Read more on the topic: Gingival pocket
This is often the cause of bad breath. The deposits in the pockets can become calcified, which leads to the formation of calculus, a type of tartar, on whose rough surface other deposits can easily adhere. If the process continues, the bone is also attacked and broken down. The tooth now loses its hold and ultimately falls out.
Often those affected do not know anything about their disease and are only surprised at loose teeth that "suddenly" fall out.
This process can drag on as a chronic course over a long period of time. It usually runs in spurts, so that the destruction of the holding apparatus comes to a standstill again and again, depending on how high the bacterial load from the dental plaque is and the state of the immune system.
In contrast, there is also an aggressive course in which teeth are lost very quickly. This form of periodontitis occurs predominantly in young people, while the more slowly progressing diseases are found in older people. Only a single tooth can be affected or entire groups of teeth can be generalized.
diagnosis
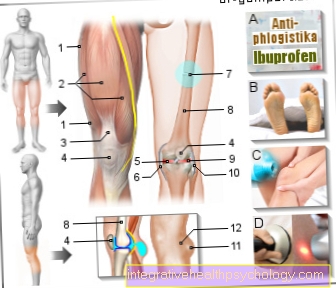
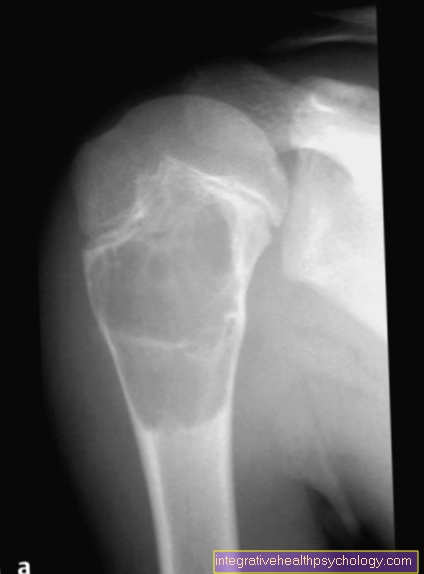
The Diagnosis is based on the measurement of the pocket depth using a special periodontal probe. This allows the loss of the attachment, i.e. the bone adhesion, to be determined. The collection and determination of Periodontal indices is another way to determine the severity of the disease. Furthermore, one can see from the degree of mobility of the teeth that it is a periodontal process and how far it has progressed. Finally, an X-ray provides clear evidence.
Therapy / treatment

Treatment of the Gingivitis and the Periodontal disease begins with the careful removal of plaque and concrements to eliminate the bacteria. In the early stages, this can still be done with home oral hygiene. But if the process is already advanced, a professional cleaning by the dentist must take place. This is especially true if it is already used Pocket formation has come.
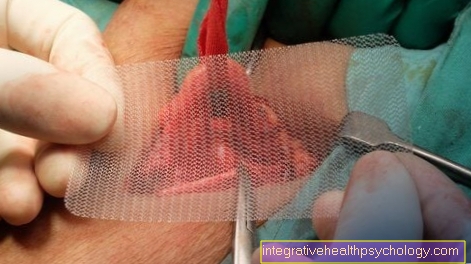
The treatment of the pockets up to a depth of 5mm can be rehabilitated by a curettage without direct view by removing all deposits and concretions. With a pocket depth of more than 5mm, the pocket is cleaned under visual conditions. The bag must be opened. In addition to clearing out the pocket, the root of the tooth is also cleaned and smoothed. In order to remove the last remnants of the bacteria you can rinse - for example with Chlorhexidine digluconate - respectively. When the tooth socket is cleaned, the periodontal disease comes to a standstill. Unfortunately, the old condition cannot be fully restored, but progression is stopped and the tooth can be preserved.
To the Bone defect to fill up again with individual teeth, one has the possibility to close the gap with suitable fillers. However, it is not possible to restore the connecting fibers. Treatment also does not cause the bone to grow back up.
prophylaxis
Before and after the renovation of a Periodontal disease a constant follow-up check should be carried out by the dentist. The cooperation of the patient is very important. They must perform careful oral hygiene to remove the plaque that keeps building up. To do this, he receives the necessary instructions from the dentist. If the patient follows the instructions, it should be possible to avoid further occurrence of periodontitis and thus reduce the risk of recurrence.
Effects
In the Periodontal disease the inflamed tissue is in connection with the whole organism. This means that pathogens can be carried from the gingival pocket to other parts of the body. Scientific research has shown that there is a link between periodontal disease and Heart disease, in particular Heart attack, gives. In this context there are other risk factors such as smoking, Diabetes and Obesity. For these reasons, too, treatment of periodontitis is urgently necessary. In order to avoid the risk of spreading germs, it is advisable to undergo treatment during the surgical rehabilitation of gingival pockets Antibiotics to undertake.
Periodontal disease and smoking
It used to be assumed that the cause of an inflammatory disease of the gum tissue is the build-up of plaque under the gumline. Poor or ineffective oral hygiene has been identified as the leading cause of these diseases.
Periodontitis should therefore be prevented by learning special tooth-brushing techniques and the use of dental floss and / or interdental brushes.
This assumption cannot be dismissed out of hand, but many other factors that favor periodontal disease (risk factors) are known today.
However, one of the most important risk factors for periodontal disease is the consumption of tobacco products (smoking). Accordingly, smoking not only has a harmful effect on the lungs and other organs, the consumption of nicotine can also have extremely harmful consequences in the oral cavity.
Studies assume that up to 50% of periodontal diseases in young adults can be attributed to smoking. Active smokers are 3 to 6 times more likely to suffer from periodontal disease than non-smokers. Former smokers still have a 2-3 fold increased risk in the first 10 years after quitting.
To understand this fact, one has to know that smoking produces a substance called carbon monoxide. This carbon monoxide binds many times over (about 200 times) stronger on the red blood pigment hemoglobin, the urgently needed oxygen is displaced and thus no longer or only insufficiently reaches its destination.
An optimal blood and oxygen supply to the organs and also to the oral cavity can no longer be guaranteed. However, since important antibodies, which lead to bleeding gums in the early stages of periodontal disease, are transported to the oral cavity with the blood, this early warning signal is mostly absent.
Illness is only noticed very late. In addition, smoking decreases the body's absorption of vitamins and minerals. However, both vitamins and minerals are essential for a strong immune system. The deficiency caused by smoking ultimately leads to a weak immune system, which makes it easy for the bacteria to cause inflammation and cause lasting damage to the tooth support system.
The progressive damage leads to degradation processes of the jawbone, but the body cannot counteract this due to the mineral deficiency.
Summary
"Periodontal disease" as a disease of the tooth bed does not exist and the misleading use of the term to describe periodontal disease should disappear from the media and advertising.
Periodontitis can be brought to a standstill by professional therapy and the cooperation of the patient, but it cannot be cured. Unfortunately, it is not possible to restore the original condition.











.jpg)