Diagnosis and therapy of appendicitis
Synonyms in a broader sense
Appendicitis therapy, appendicitis treatment, diagnosis of appendicitis
introduction
Diagnosing appendicitis can be challenging even for an experienced doctor. The symptoms are not always that clear and there are some diagnoses that present themselves with similar symptoms (differential diagnoses). The variable position of the appendix (appendix) also represent a diagnostic problem.
Once the diagnosis is established, appropriate therapy can be considered.

Diagnosis of appendicitis
The physical exam
In the doctor-patient conversation (anamnesis) it should be asked whether there has been the typical displacement of the pain from the middle abdomen to the right lower abdomen.
Most important, however, is the findings of the physical examination, in which some examination methods can be groundbreaking.
- Pressure pain in the right lower abdomen is the most important key finding. With the pain maximum in the McBurney point and / or Lanz point. The McBurney point is located in the outer third between the right anterior upper iliac spine (spina iliaca anterior superior) and the navel. The Lanz point is in the right third of the line between the two front upper iliac spines.
- The Blumberg sign is pain in letting go of the left (contralateral) side of the abdomen. The left lower abdomen is slowly pressed in and then quickly released again.
- If you wipe the colon in the direction of the cecum, you can provoke pain, which is called the rovsing sign.
- If the peritoneum is already involved, you can notice increased muscular defense tension (Défense musculaire) when you feel the abdomen.
- A knocking pain (percussion pain) in the triangle between the right anterior iliac spine (anterior superior iliac spine), the navel and the pubic symphysis, the so-called Sherren's triangle, is of particular importance.
- When listening (auscultation) of the abdomen with the stethoscope, vivid intestinal noises are initially noticeable when the inflammation begins. The intestinal noises become silent as the peritonitis develops, reflex intestinal paralysis with threatened intestinal obstruction (ileus) can develop.
- In the further course of a complicating peritonitis, there is occasional pain when palpating the rectum with the finger (rectal digital examination). This phenomenon suggests an abscess or inflammatory fluid build-up in the pelvis.
- Body temperature should be measured both in the armpit (axilla) and in the rectum. 50% of the patients show an axillary-rectal difference of 1-0.8 ° C.
- The psoas signs appear when the appendix lies on the ileopsoas muscle, that is, behind the appendix (retrocecal). In this case, bending the leg in the hip joint against resistance is painful.
- With Chapman's sign, the patient is in pain when straightening up from a sitting position.
Read more on the topic: Tests to detect appendicitis
Illustration of appendicitis

- Appendix -
Caecum - Colon, ascending part -
Ascending colon - End part of the ileum -
Ileum, pars terminalis - Free tape strip -
Taenia libera - Appendix -
Appendix vermiformis
Appendix inflammation -
Appendicitis
A - Catarrhal stage
(The appendix is
swollen, reddened
and painful)
B - Seropurulent stage
(Transition stage between A and C)
C - Destructive stage
- Ulcerophlegmonosa appendicitis -
The mucous membrane shows ulcers.
Beginning of tissue destruction
- Appendicitis empyematosa -
Pus forms in the appendix
- Appendicitis gangrenosa -
The appendix slowly dies.
Gangrene develops
(Tissue destruction)
You can find an overview of all Dr-Gumpert images at: medical illustrations
Laboratory values
In the blood test you should pay particular attention to the Inflammation values respect, think highly of. These values include the white blood cells (leukocytes), which increase in the body when an infection occurs ( >12.000 Cells / µl blood (Leukocytosis). The degree of leukocytosis does not always correlate with the urgency of the disease. The white blood cell count can rise particularly rapidly in small children and it can be very low or even absent in older people.
This serves as an additional parameter C-reactive protein (CRP value). The CRP produced by the liver is a so-called one Acute phase protein and increases sharply in viral and especially bacterial infections.
To a urological cause (e.g .: Cystitis), which can be associated with similar symptoms, should always be excluded Urine test strips (Urostix) deploy.
Read more information on the topic: Levels of inflammation in the blood
Sonography
With sonography (ultrasound), abdominal organs can be assessed non-invasively (without physical harm) and without exposure to radiation. First, the transducer sends ultrasonic waves that are absorbed or reflected by the various types of tissue it encounters. On the other hand, the transducer receives these reflected waves again, which are converted into electrical impulses and displayed on a screen in different gray levels. The depiction of the appendix in sonography is particularly difficult and belongs in the hands of an experienced examiner. Today's devices have a high resolution, which makes it possible to diagnose appendicitis in a very high percentage. The examination is sometimes difficult because the appendix has a particularly variable position and is often overlaid by intestinal gases that are located in the appendix and small intestine. The examiner has to "push away" the air overlay with constant pressure and a lot of patience. A healthy appendix has a diameter of approx. 6 mm and is three-layered. An inflamed appendix appears swollen and is larger than 8 mm. If the appendix diameter is between 6 and 8 mm, repeated sonographic controls should be carried out in order to quickly detect any deterioration in the findings. Further indications of inflammation are a fluid border around the appendix, increased blood flow to the appendix wall, pain on pressure and an incompressible appendix with targeted pressure. The most characteristic sign, however, is the "cockade" (the appendix acts like a target in cross-section), which appears more and more washed out and less hypoechoic (darker) as the disease progresses. The reliable diagnosis of a perityphilitic abscess is particularly important. The intestinal wall appears destroyed (destroyed) and hypoechoic cavities appear.
Read more on the topic: Ultrasound of the abdomen
roentgen
If you have sudden severe abdominal pain (Acute abdomen) an x-ray of the abdomen cannot directly diagnose inflammation of the appendix, but it may rule out complications. However, an X-ray can show certain signs of appendicitis. So one can be strong more aerated appendix (Toothy meteorism) With Liquid levels be an important clue in the right lower abdomen. If the appendix is located behind the appendix (retrocecal position) and Co-ignition of the Shell (Fascia) of Muscle Ileopsoas can he Psoas edge shadow in the X-ray compared to the opposite side. If the peritonitis is very advanced and diffuse, the appearance of intestinal paralysis (Paraytic IIeus) present, with highly aerated intestinal loops and fluid levels. These mirrors are created by standing liquid in the intestinal loops, over which a aerated cavity arises. The cavities appear like dark semicircles in the X-ray image. If there is already a abscess has formed, one can possibly guess a level of fluid inside the abscess that is not surrounded by the intestinal wall (extraintestinal).
Therapy for appendicitis

The only causal therapy for appendicitis is this surgical appendix removal (Appendectomy). The most important thing is to confirm the diagnosis quickly or at least to have a well-founded suspicion so that the operation can be performed within 48 hours of the onset of symptoms. The doctor will first get one Food leave (Zero diet) and the nutrition about the vein (parenteral). The cooling of the lower abdomen with a "Ice bubble " can provide relief and the the gift of Antibiotics (Drugs that kill bacteria before surgery reduce the risk of bacteria spreading.
There are two options for surgical appendix removal:
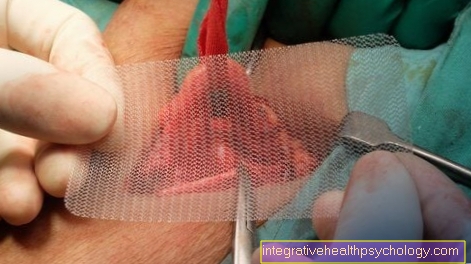
1. Open appendectomy:
The most common approach for an appendectomy is Alternate cut. This cut runs diagonally from the top right to the bottom left in the right lower abdomen.
After the skin incision, the appendix is first found and the appendix is shown. The appendix is like that Small intestine, on one small mesentery (Mesenterioum) attached to the posterior wall of the abdominal cavity. In this maze they run Appendix-supplying Vesselsthat are tied off during the operation (ligatures) and then separated. Then the appendix itself is tied off and cut off. The one that emerged afterwards Appendix stump is by means of Purse-string seam or Z seam sunk in the appendix.
2. Laparoscopic appendectomy:
Hirunter understands the removal of the appendage with the help of the smallest construction cuts and the use of an operation camera (Minimally Invasive Surgery; Keyhole surgery). The first incision is made under the navel (infraumbillical), and over this one Mini camera inserted into the abdominal cavity. In this way the abdominal cavity is inspected. Working instruments are introduced through two further incisions (mostly in the left and right lower abdomen). The inflamed appendix is then removed through these working channels. The advantages of the laparoscopic procedure are the low tissue damage and the good overview of the abdominal cavity through the camera.
If appendicitis has not been surgically confirmed, it is still justifiable preventive (prophylactic) Appendectomy perform. However, the abdomen should be searched intensively for other causes of the discomfort. The small intestine should always be systematically searched for Meckel-Diverticulum to be examined. In women, the examination of the female inner Genitals of particular importance, since common causes of pelvic pain are found here (see above).
If there is another cause for the symptoms than appendicitis, the appendix should be left in place.
After removing the appendix, the pathologist should examine the specimen under a microscope fine tissue (histologically) to be examined. It should be excluded that a previously undiscovered carcinoma or carcinoid is stuck in the inflamed appendix.
Some complications can also arise after the operation. This includes Wound infections, Abscesses, Intestinal paralysis With Intestinal obstruction (Ileus) and a leak in the appendix stump (fistula). A more mechanical Intestinal obstruction (Ileus) can be found after a few days after the appendix removal early intestinal paralysis (early ileus) at Bonding arise from wound healing. But even years after the operation you can get through Adhesions (Brides) in the abdomen Late ileus arise.
The postoperative mortality is 0.2% for uncomplicated courses and increases to 10% for diffuse peritonitis.
Exclusion diseases
If the symptoms of appendicitis are unclear, other diseases with a similar constellation of symptoms must also be considered (differential diagnoses).
in the Toddler age must as differential diagnoses to a telescopic Intestinal invagination (Intussusception) or rotation of Intestines including intestinal mesentery (Volvolus) should be thought. But also a diabetes mellitus can manifest with unspecific abdominal pain.
Schoolchildren, on the other hand, may have similar symptoms in one Intestinal flu (Enteritis) or at Worm diseases Offer.
With the puberty and in boys Adulthood come diseases like DiseaseCrohn or Urinary tract infections added. Come with women gynecological Diseases like Endometriosis in the intestine, Fallopian tube inflammation (Adnexitis) and Ectopic pregnancy (Tubal pregnancy). In addition, particularly pronounced Menstrual pain (Dysmenorrhea) show a similar symptom picture.
For abdominal pain in people im middle age there are still diseases like Kidney stones (Urolithiasis) and more painful in women Ovarian cysts (Ovarian cysts) in question.
Elderly people are more likely to suffer from diseases such as intestinal protuberances (Diverticulum) in the cecum, a Cecal carcinoma, one ischemic Colitis or at one Bowel infarction.
Certain differential diagnoses show little regardless of age, how Meckel's diverticulum, Inguinal hernia (Inguinal hernia), Carcinoids the appendix and Salmonella infections (typhus, Paratyphoid).
Conservative therapy / surgery
Appendicitis (appendicitis) is caused by the immigration of germs via the blood into the Appendix (commonly referred to as the appendix) or by relocating intestinal contents (Feces) with bacteria / germs in the appendix.
Usually there is severe pain in the right lower abdomen within a few hours, nausea and Vomit.
If the symptoms get worse by the hour, it is usually acute appendicitis, i.e. a rapidly progressing inflammation of the appendix (appendix).
Here it is important to act quickly and the doctor usually has no choice but to carry out an operation to avoid breaking through the intestinal tissue and the inflamed and germ-colonized contents from entering the open abdominal cavity.
In principle, however, there is also the possibility of treating appendicitis conservatively, i.e. without an operation. This is rarely suggested by the doctor, but it cannot be done if the inflammation is severe.
Especially patients who are under a chronic appendicitis sufferers, i.e. recurring symptoms, can use this method, but the term chronic appendicitis is not really defined, which is why the conservative method is only used very rarely.
However, if the patient wants a therapy without an operation, the patient must keep absolute bed rest in order not to put unnecessary strain on the stomach and a Rupture of the intestinal wall not to provoke.
In addition, the patient must not eat anything for the entire duration of the inflammation (Food leave).
In order to drive the healing further, the appropriate ones should also be used Antibiotics (depending on the bacterium) can be taken.
In addition, the patient should be strictly monitored clinically in order to be able to operate as soon as possible if the signs get worse.
Generally speaking, appendicitis (appendicitis) always a clinical emergency and should therefore always be operated on.
Especially since the operation is now a routine procedure with few risks.
With conservative therapy, however, one provokes an aggravation of the disease.
Operation appendicitis
Appendicitis (appendicitis) is a fairly common condition that occurs mainly in young people under the age of 23.
More precisely, however, the appendix is not (Caecum) inflamed but only the appendix (Appendix vermiformis) of the appendix.
Nevertheless, one speaks of appendicitis in common parlance.
Correspondingly, the surgical removal of the appendix is also called appendectomy, but doctors speak of an appendectomy (surgical removal of the worm head).
An operation is always necessary for acute appendicitis. It is important that quick action is taken in the event of appendicitis.
The patient should be operated on at the latest 36 hours after the first symptoms to avoid a breakthrough of the inflamed tissue, as the inflamed tissue can otherwise penetrate into the open abdominal cavity.
A definite diagnosis should be made before the operation, usually through an ultrasound scan.
During the operation, the patient must first be anesthetized so that he is pain-free (analgesia) and sleeps during the operation.
General anesthesia is usually used.
There are basically two types of surgery for appendicitis. On the one hand, there is the open operation, in which the abdominal wall is completely opened with the help of a scalpel.
The advantage of this method is the very good overview of other organ systems.
The disadvantage is the larger scar and the longer follow-up treatment.
Most of the time, this method is only used today if the appendix has ruptured, as in this case the doctor has to rinse out the abdomen to remove the inflamed secretion in the abdomen.
The second surgical technique is laparoscopy in which the doctor uses a small endoscope and a small camera to examine the appendix ("appendix") Can remove.
In addition, carbon dioxide is pumped into the abdomen to detach the intestine from the surrounding structures.
The appendix is then removed using a stapler. The surgeon has a poorer overview with this technique, but the patient can be discharged home much faster after the operation and does not have a large scar, instead only three small points remain in the area of the abdomen through which the surgeon operated.
Both operations are usually performed with self-dissolving sutures to avoid pulling sutures after the operation.
The patient can take liquid food again just one day after the laparoscopic operation. With open surgery, it usually takes longer before the patient can walk and eat normally again.
Further information on this topic can be found at: Appendectomy
Therapy of chronic appendicitis
In the case of appendicitis, a basic distinction should be made between acute appendicitis and chronic appendicitis. Acute appendicitis is actually always an indication for an operation (rare exceptions are patients who are at great risk from operations because they cannot tolerate anesthetics, for example).
Chronic appendicitis has a gradual course, the symptoms are sometimes worse and sometimes less severe.
Often it is just one Appendix irritation.
Many authors therefore avoid the term chronic appendicitis and speak exclusively of irritation of the appendix.
Here, too, an appendix removal can help as a therapy because the symptoms that often occur disappear afterwards.
However, you can also use a conservative therapy carry out. It is important here with the first Signs of appendicitis from pain in the right lower abdomen to forego any food and absolute bed rest to keep. In addition, it is best to be monitored by a doctor and also to receive antibiotics against the germ in question.
Since the patient shouldn't be drinking either, it is important to have one infusion to be placed and possibly also to have a feeding tube placed. If the symptoms do not get better within the next day, however, you should see a doctor immediately and undergo appendectomy, otherwise there is a risk of a breakthrough.
Antibiotics for appendicitis
Acute appendicitis is always an indication for emergency surgery, otherwise the appendix threatens to break through.
In some cases, for example in patients who have had an operation, for example because of Intolerance to anesthesiaIf you don't want to, you can first try to prevent the operation and instead treat the patient conservatively with antibiotics.
Opinions as to whether such a treatment makes sense or whether antibiotic therapy only delays the time of the operation vary widely.
However, since a patient who opts for conservative antibiotic therapy must be permanently monitored in hospital and artificially fed during the treatment, surgery is usually preferred.
Especially in chronic appendicitis (sometimes referred to as appendix irritation) one tries to avoid surgery with the help of antibiotics.
The antibiotic is used here depending on the pathogen and depending on Resistance of the pathogen elected.
Some studies show that if a child is given antibiotics intravenously for 24 hours (so through the blood into the vein) and then swallow the antibiotic for another week (ingests orally) that these children are fit again much faster than children who have had to undergo an operation.
In Germany, however, conservative antibiotic therapy for appendicitis is viewed as critical.
If the appendix breaks through (perforation), the patient must then be treated with a high dose of antibiotics, as the bacteria are then located in the free abdominal cavity and must be rendered harmless by the antibiotic in order to avoid blood poisoning (sepsis), for example .
Chronic appendicitis
The diagnosis of chronic appendicitis is often controversial. One speaks of chronic appendicitis when repeated, almost symptom-free flare-ups of inflammation of the appendix have occurred, but these have receded on their own. The symptoms are often very discreet but recurring. The operation is not infrequently a solution to the embarrassment, but it does provide permanent relief for the majority of those affected. The histological preparation of the specimen often shows adhesions and inflammatory infiltrates.