Lymphocytes - What You Should Know!
definition
Lymphocytes are a highly specialized subgroup of leukocytes, the white blood cells that belong to the immune system, the body's own defense system. Their name is derived from the lymphatic system, as this is where they are particularly common.
Their main task is primarily to defend the body against pathogens such as viruses or bacteria. For this purpose, certain cells specialize in only one pathogen, which is why one speaks of the specific or adaptive immune system.
But they also help to eliminate mutated body cells, so-called tumor cells, which can lead to cancer. A distinction is made between B and T lymphocytes, as well as natural killer cells, each with different functions.

Function of the lymphocytes
If a pathogen gets into the body, it is first absorbed and broken down by unspecific defense cells such as macrophages ("giant eating cells"). The macrophages in turn show fragments of the pathogen, so-called antigens, on their surface and thus activate T helper cells, which serve as mediators between the different specific immune cells, the lymphocytes. The lymphocytes ensure that the immune system is very adaptable and can react in a finely regulated manner to different threats.
The following reaction is divided into the humoral and the cellular immune response:
The humoral (= the body fluids) immune response is based on the antibodies, a certain form of proteins, which are produced and released by plasma cells. It is mainly designed for pathogens that can multiply on their own, e.g. bacteria, but also other single-celled organisms. The antibodies can, for example, stick to the surface of bacteria and clump them together due to their special shape (agglutination). This in turn makes it easier for the unspecific immune cells to find the pathogen and eliminate it. Antibodies can also fulfill a number of other functions (see B lymphocytes).
The cellular immune response is mainly focused on viruses, but also on certain bacteria, which cannot live on their own and therefore have to attack body cells. If a cell is attacked, it can show fragments of the parasite on special receptors on its surface. Killer T cells destroy the infected cells and thus prevent the further spread of the pathogen.
Read more on this topic: immune system as T lymphocytes
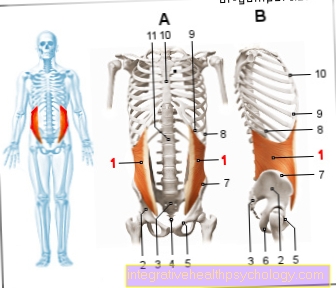
Anatomy and development of the lymphocytes
Lymphocytes are very variable in size at 6-12 µm and are particularly noticeable because of the large, dark nucleus that fills almost the entire cell. The rest of the cell can be seen as a thin cytoplasmic border in which there are only a few mitochondria for energy production and ribosomes for the production of proteins.
It is assumed that the larger forms of the lymphocytes, which also have a lighter (= euchromatic) cell nucleus, were activated by bacterial or viral attack. Smaller inactive lymphocytes, which are also called naive, are much more common in healthy people and are about the same size as the red blood cells (erythrocytes).
Read more about: Erythrocytes
Lymphocytes arise via the intermediate stage of lymphoblasts from hematopoietic stem cells (hematopoiesis = blood formation), most of which are located in the bone marrow in adults. Here the precursor cells (progenitors) of the lymphocytes differ from those of the other (myeloid) cells in that some of them continue to mature in the thymus (also called sweetbreads). These are later called T lymphocytes ("T" for thymus). The maturation in the thymus pursues the purpose of sorting out all those T cells that react to the body's own structures or are otherwise restricted in their function (positive and negative selection).
For more information, see: T lymphocytes
The B lymphocytes and NK cells (natural killer cells), on the other hand, complete their maturation like the other blood cells in the bone marrow ("B" for "bone marrow" or historically Bursa fabricii, an organ of birds). After the B-lymphocytes have left the bone marrow as mature, naive (= unspecialized) cells, they enter organs such as the spleen, tonsils or lymph nodes, where they can come into contact with antigens (foreign structures). For this purpose, the cell carries certain antibodies on its surface, which serve as B-cell receptors. So-called dendritic cells, another type of immune cell that does not belong to the lymphocytes, present antigen fragments to the naive B lymphocytes and activate them with the help of the T helper cells. If a B cell has been activated, it divides several times and transforms into a plasma cell (clonal selection).
The different types of lymphocytes look very similar, but can be differentiated from one another using special marking and staining methods (immunohistochemistry) under the microscope.
B lymphocytes
When activated, the majority of mature B cells develop into plasma cells, the task of which is to form antibodies against foreign substances. Antibodies are Y-shaped proteins that can bind to very specific structures, so-called antigens. These are mostly proteins, but often also sugars (carbohydrates) or lipids (fatty molecules). The antibodies are also called immunoglobulins and are divided into 5 classes based on structure and function (IgG, IgM, IgD, IgA and IgE).
The antibodies now help in various ways to fight the infection: For example, poisons such as tetanus toxin can be neutralized or the entire pathogen can be marked. A pathogen marked in this way can now be absorbed and digested by certain immune cells, the macrophages and neutrophils. However, the pathogen can also be destroyed and dissolved by natural killer cells, as well as macrophages and granulocytes by substances that are poisonous for the pathogen. Some antibodies can also clump the target cells to make them easier to detect and to make them more receptive.
Another way is via the activation of the complement system, which is made up of several unspecific proteins that dissolve marked cells in a kind of chain reaction. However, these proteins are permanently present in comparable concentrations in the blood and are part of the innate immune system. In addition, mast cells are activated by antibodies, which release inflammatory substances such as histamine, which increase the blood flow to the affected tissue and thus make it easier for other immune cells to reach the focus of inflammation.
You might also be interested in: histamine
Another subgroup of B-lymphocytes develops into B-memory cells when activated, which can survive for several years. If the body is exposed to the same pathogen again during this time, these cells can develop into plasma cells much faster in order to stop the infection from spreading more efficiently. This creates vaccination protection that lasts for a long time and can last for years.
For detailed information, see also: What are B lymphocytes?
T lymphocytes
There are two main groups of T lymphocytes, T helper cells and T killer cells, as well as regulatory T cells and, in turn, long-lived memory T cells.
The T helper cells strengthen the effect of the other immune cells by binding to antigens that are presented on other immune cells and then release cytokines, a kind of attractant and activator for other immune cells. Depending on the type of defense cells required, there are further specialized subgroups. They play a special role in activating plasma cells and killer T cells.
Killer T cells are also called cytotoxic T lymphocytes because, unlike most immune cells, they destroy their own cells instead of those that are foreign to the body. This is always necessary when a cell in the body is attacked by a virus or another cell parasite or when a cell is changed in such a way that it could become a cancer cell. The T killer cell can attach itself to certain antigen fragments that the infected cell carries on its surface and kill them through various mechanisms. A particularly well-known example is the introduction of a pore protein, perforin, into the cell membrane. This causes water to flow into the target cell, causing it to burst. You can also induce the infected cell to self-destruct in a controlled manner.
Regulatory T cells have an inhibitory function on the other immune cells and thus ensure that the immune reaction does not continue to build up and can quickly subside again. They also play a major role in pregnancy, as they ensure that the cells of the fetus, which are ultimately also foreign, are not attacked.
Like the B memory cells, T memory cells are preserved for a long time and also ensure a faster immune response if the pathogen reappears.
Natural killer cells
Natural killer cells or NK cells play a similar role as the T killer cells, but unlike the other lymphocytes, they do not belong to the adaptive but to the innate immune system. That means they are permanently functional without having to be activated beforehand. However, it is difficult to regulate their response. Nevertheless, they belong to the lymphocytes, as they arise from the same progenitor cells.
Read more on the subject.
- immune system
- How can you strengthen the immune system?
Normal values of the lymphocytes
The concentration of lymphocytes fluctuates throughout the day and depends on the time of day, stress, physical exertion and other factors. One speaks of a pathological increase only if the lymphocytes are above the limit values.
To determine the number of lymphocytes, you need a differential blood count, which is part of the large blood count. The proportion of lymphocytes in the total leukocyte count (leukocyte = white blood cells) should be between 25 and 40%, which corresponds to a concentration of 1,500-5,000 / µl. If the value is above this is called lymphocytosis, if it is below it is called lymphocytopenia (also called lymphopenia). In small children, the concentration of leukocytes can be significantly higher and the proportion of lymphocytes can be up to 50%.
Read more about: Blood count
What can be the cause if the lymphocytes are increased?
Infections as a cause of an increase in lymphocytes
In most cases, an increased number of lymphocytes (= lymphocytosis) indicates a viral infection, as lymphocytes are particularly suitable for combating them. Basically, with all virus infections, at least a slightly increased lymphocyte concentration can be expected.
In addition, certain bacterial infections such as pertussis (whooping cough, stick cough), tuberculosis (consumption), syphilis, typhus (enteric fever, parental fever) or brucellosis (Mediterranean fever, Malta fever) trigger a characteristic increase in lymphocytes. The number of lymphocytes remains increased even with chronic, i.e. long-lasting courses. Other parasites such as Toxoplasma gondii can also lead to a short-term increase in lymphocytes.
Read more about: Infectious diseases
Autoimmune diseases
However, there are also inflammatory diseases without infection that lead to an increased number of lymphocytes, such as B. the intestinal diseases Morbus Crohn and ulcerative colitis, as well as autoimmune diseases like Morbus Graves, in which the lymphocytes form antibodies against thyroid cells, whereby these are overly excited, which in turn disturbs the hormonal balance. Sarcoidosis (Boeck's disease), a special type of inflammation that particularly often affects the lungs, can also lead to an increase in the number of lymphocytes.
More information can be found here: Sarcoid
Thyroid disease
However, a disturbed balance of thyroid hormones, as in the case of an overactive thyroid (hyperthyroidism) or Addison's disease (primary adrenal insufficiency), can also lead to an increased lymphocyte count.
You might also be interested in: Addison's disease
Rise in leukocytes due to tumor diseases
Particularly severe lymphocytosis can develop in certain malignancies, i.e. malignant tumor cells:
In chronic lymphocytic leukemia (ALL), it is the precursor cells of the lymphocytes that have developed into cancer cells due to mutations. It is the most common form of leukemia in the western world. Since it occurs particularly frequently around the age of 50, it is also referred to as "age leukemia".
Acute lymphoblastic leukemia also arises from lymphocyte precursor cells, but is usually accompanied by rapid degeneration of the bone marrow, which can lead to anemia, as the other blood cells cannot properly develop. As a result, in some cases no change or even a decrease in total leukocytes can be determined. The abnormally increased number of lymphocytes can only be seen in the differential blood count.
Since the mutated lymphocytes are usually functionless in both diseases, a reduced performance of the immune system can be assumed despite the increased number.
Furthermore, other malignant (malignant) tumors that affect other cells of the lymphatic system can trigger lymphocytosis, for example Hodgkin's lymphoma (Hodgkin's disease, lymphogranulomatosis, lymphogranuloma), but also certain non-Hodgkin's lymphomas.
Also read: Hodgkin lymphoma as leukemia
What can be the cause if the lymphocytes are low?
Lymphocytopenia often occurs as a result of therapy and is not considered pathological in this context: This is particularly common when treating with corticoids, especially cortisone, and when administering antilymphocyte globulin. Both are used specifically to suppress inflammatory reactions. Other forms of therapy that can cause lymphocyte deficiency are radiation and chemotherapy, both of which are used for cancer therapy, but can also affect rapidly dividing body cells such as the precursors of blood cells. In addition, this phenomenon was observed when the drug ganciclovir was administered, which is mainly used to treat cytomegalovirus (CMV, human herpesvirus 5, HH5). During treatment with long-wave UV light (UVA), the natural substance psoralen is often co-administered due to its photosensitizing effect, which can also have a reducing effect on the leukocyte count.
Another possible reason for lymphocytopenia is low-protein malnutrition or persistent stress, which can permanently increase the cortisol level (see cortisone therapy). In addition, there are also clinical pictures with an organic cause such as Cushing's disease, which stimulates the adrenal medulla to produce increased cortisol due to a malfunction of the pituitary gland (adenohypophysis). Certain autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus (butterfly lichen) and exudative (gastro) enteropathy (Gordon syndrome) can also lead to lymphopenia.
In uremia, due to a kidney malfunction, substances accumulate in the blood, which in healthy people are discharged through the urine. In addition to a number of other symptoms, this also leads to decreased leukocyte function.
Since an infection with the HI virus (human immunodeficiency virus, triggers AIDS) particularly affects and destroys the T helper cells, a sharp drop in the number of lymphocytes is also to be expected here.
There are also congenital causes that mostly affect the development of lymphocytes (lymphocytopoiesis) and are triggered by mutations in the genes for certain enzymes. These include the adenosine deaminase deficiency and the purine nucleoside phosphorylase deficiency, as well as the Wiskott-Aldrich syndrome, which primarily affects the thrombocytes (blood platelets) due to the disturbed formation of the cell skeleton, and lymphocytopenia and immunodeficiency usually only develop in later years of life.
In addition, certain Hodgkin lymphomas (Hodgkin's disease, lymphogranulomatosis, lymphogranuloma) and individual non-Hodgkin lymphomas, i.e. cancer of the entire lymphatic system, can impair the development of lymphocytes and consequently reduce their number.
Also read: Myastenia gravis or HIV
How do the lymphocytes change with a cold?
The everyday terms cold and flu-like infection stand for a number of different, mild diseases of the respiratory tract, which are mostly caused by viruses, but occasionally also by bacteria.
It is typical for bacterial infections that the total number of leukocytes increases (= leukocytosis), which usually also affects the lymphocytes. In viral infections, the total number of leukocytes tends to be reduced (= leukopenia), which is often due to the fact that the immune system cannot keep up with the production of defense cells, but certain viruses can also inhibit the immune system directly. It is characteristic, however, that the number of lymphocytes remains stable or even increases, since these are particularly suitable for combating viral infections and therefore develop preferentially from the common stem cells.
How do the lymphocytes change in HIV?
The HI virus (human immunodeficiency virus) attacks cells that have a specific surface protein, the CD4 (cluster of differentiation). These are primarily the T-helper cells, which are destroyed by the replication of the virus, which drastically reduces the number of lymphocytes (lymphopenia). The loss of functional T helper cells exceeds the amount of infected cells, so that indirect inhibition mechanisms must also play a role, which for example affect the maturation of the lymphocytes. In addition, macrophages (giant phagocytes) are also attacked, although these are not lymphocytes and only a comparatively small proportion die.
In the very first phase around 1-4 weeks after infection (primary infection), patients often show symptoms similar to colds for around a week. However, the number of leukocytes usually increases slightly here, while the number of lymphocytes decreases. This is often followed by a symptom-free period in which the number of lymphocytes only decreases very slowly, remains stable or even normalizes. This condition can last for several years and often goes unnoticed until, if left untreated, it eventually develops into AIDS.
More information about HIV can be found here.
Lifespan of the lymphocytes
The lifespan of lymphocytes can be very different due to the different tasks: Lymphocytes that never come into contact with antigens (foreign body structures) die after a few days, while activated lymphocytes, e.g. plasma cells, can survive for about 4 weeks. The memory cells survive the longest, as they can survive for several years and thus contribute to immunological memory.
According to more recent findings, there are also long-lived plasma cells that still produce appropriate antibodies even after the infection has subsided and thus ensure a stable antibody titer (= dilution level).
Lifelong immunity is usually only achieved with live vaccines, whereby it is to be expected that an extremely small, harmless portion of the vaccine will remain in the organism.
What is the lymphocyte transformation test?
The lymphocyte transformation test (LTT) is a method for the detection of special T lymphocytes, each of which has specialized in a certain antigen (foreign body fragment). It has recently been used primarily in immune function diagnostics, but also in allergology for the detection of allergies to certain drugs or metals, which manifest themselves only after a delay. It is currently recommended primarily as a supplement to the patch test. This test is a provocation test to check for contact allergies. In addition, the informative value as a detection test for certain pathogens such as Lyme disease is currently being discussed controversially.
In the first step of the lymphocyte transformation test, the lymphocytes are separated from the other blood cells by several washing processes and centrifugation (a process that breaks down the blood components according to their mass). The cells, together with the test antigen, are then left to their own devices for a few days under optimal growth conditions. A control sample remains without antigen. 16 hours before the evaluation, radioactively labeled thymine, a component of DNA, is added. After the time has elapsed, the radioactivity of the lymphocyte culture is then measured and a so-called stimulation index is calculated from this. This provides information about whether and how sensitive the T lymphocytes are to the antigen.
The test makes use of the fact that activated T cells, which increasingly arise from sensitized memory T cells, convert or transform themselves in response to the corresponding antigen. As a result, they also share, for which reason they have to build up DNA and therefore increasingly incorporate the radioactive thymine.
Lymphocyte typing
Lymphocyte typing, also known as immune status or immunophenotyping, is a process that examines the formation of various surface proteins, usually so-called CD markers (Cluster of Differentiation). Since these proteins differ in the different lymphocyte types, a so-called expression pattern of the surface proteins can be created through the use of artificially produced, color-coded antibodies. From this, conclusions can be drawn about the distribution of the different types, but also about the degree of differentiation of the cells. This method is therefore particularly suitable for the classification of leukemia, but it is also used, for example, to monitor HIV infections.
You might also be interested in: Leukemia or HIV infection.
Lymphocytes in the urine
The increased number of lymphocytes in the urine is called lymphocyturia, which occurs particularly often in viral infections, lymphomas and rejection reactions after kidney transplantation without an increase in the other immune cells.
In most cases, however, only the number of all leukocytes is considered in the context of the urine status, whereby one would only think about a pathological cause from a concentration of more than 10 / µl. Such leukocyturia often occurs in connection with a urinary tract infection, but can also have other causes such as prostate inflammation, a rheumatic disease or pregnancy. One then speaks of sterile leukocyturia, since no bacteria could be found besides the increased number of leukocytes.
Lymphocytes in the CSF
The cerebrospinal fluid, i.e. the fluid in which our brain swims, is comparatively poor in cells, of which, however, T lymphocytes make up the majority. A concentration of 3 / µl is normal here. In addition, there are also isolated monocytes, the precursors of macrophages ("giant phobia"). The presence of other blood cells is already considered to be pathological.
If the blood-cerebrospinal fluid barrier, which controls which substances are allowed to pass from the blood into the cerebrospinal fluid, remains intact, only these two cell types increase accordingly. This is the case, for example, with meningitis (meningitis), borreliosis or syphilis, but also with infection-free diseases such as multiple sclerosis or special brain tumors, as well as with certain brain injuries.