Gastrointestinal bleeding
Synonyms in a broader sense
GI bleeding; Gastric bleeding, Intestinal bleeding
Medical: gastrointestinal bleeding, ulcer bleeding
English: gastrointestinal bleeding (haemorrhage)
Definition gastrointestinal bleeding
A Gastrointestinal bleeding is a bleeding of the gastrointestinal tract that is visible to the outside. blood is either vomited or passed with the stool, which then becomes black or bloody bowel movement can lead.

Frequency (epidemiology)
Occurrence in Germany
In Germany around 100 per 100,000 inhabitants are affected by gastrointestinal bleeding every year. An increasing share is attributable to those over 60 years of age.
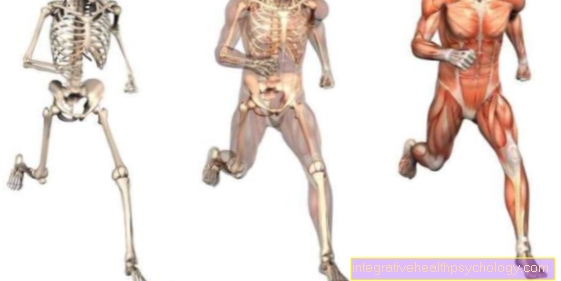
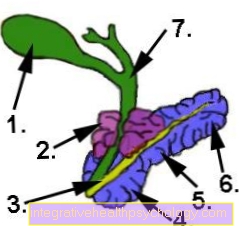
Illustration gastric ulcer
The gastric ulcer can be seen localized at a typical location at the gastric outlet.
In the picture below, the stomach wall is shown in cross section and you can see how deep the stomach ulcer extends.

Layers of the stomach lining
- Mucosa (mucous membrane)
- Gastric ulcer
- Submucosa (layer of connective tissue)
- Blood vessels
If the mucous membrane is damaged, it can reach into the underlying connective tissue, which can lead to gastric bleeding.
Danger of death
While chronic gastric bleeding often goes unnoticed for a longer period of time and only as Incidental finding (Symptoms of anemia, typical blood count) are noticed, acute gastric bleeding, on the other hand, often occurs massive and life threatening, whereby death can occur in 10-20% of cases.
Gastric bleeding is always dangerous when it is in the context of Inflammation of the gastric mucosa and gastric ulcers to injuries or openings of larger gastric vessels (A. gastrica) because they can cause large amounts of blood to be lost in a relatively short period of time (a loss of 20% of the normal blood volume is life-threatening).
Furthermore, congenital vascular malformations in the stomach can cause major bleeding when injured. The so-called "Dieulafoy ulcer " is a rare, congenital disease in which a gastric ulcer can open an enlarged vascular abnormality very close to the mucous membrane and lead to life-threatening bleeding. If gastric bleeding does not stop on its own or if there is major blood loss with shock symptoms due to acute blood deficiency in the circulatory system, rapid endoscopic or surgical hemostasis must be initiated. The administration of blood reserves can also be necessary in the event of high blood loss.
Causes and development (etiology and pathogenesis)
The trigger one gastrointestinal bleeding (Gastrointestinal bleeding) are very diverse:
- Medication, so-called. NSAIDs (non-steroidal anti-inflammatory drugs)
- Portal hypertension (medical: portal hypertension) and the often associated formation of enlarged veins that tend to bleed esophagus (medical: Esophageal varices),
can cause bleeding in the stomach or intestines.
Also through Stomach acid chemical burns and malignant tumors of the stomach (gastric carcinoma / Stomach cancer) represent possible reasons.
As a rule, gastric bleeding can be viewed as a result of various underlying diseases and manifests itself either as acute, life-threatening or chronic complication. In about 50% of patients who suffer from gastric bleeding, so-called Stomach ulcers (Gastric ulcer) in front.
This is a defect in the stomach wall that extends beyond the gastric mucosa and goes through it stress, decreased Mucosal blood flow, chronic use of anti-inflammatory and pain relievers (NSAIDs such as B. Ibuprofen, Diclofenac) or one Gastric infection with the bacterium Helicobacter pylori can be caused.
If gastric ulcers persist for a long time, if left untreated, they can deepen and spread, so that gastric vessels may be destroyed or even too Perforations in the stomach wall can come. In 15% of cases, however, damage is only to the gastric mucosa (erosion) responsible for the gastric bleeding that occurs.
This usually arises from an inflammatory stomach disease (erosive gastritis), which are also caused by taking medication (NSAIDs, Glucocorticoids), Bacteria (Helicobacter pylori) or viruses (e.g. noroviruses), stress, but can also be caused by alcohol or nicotine abuse as well as autoimmune reactions and bile acid reflux from the small intestine.
Excessive and prolonged consumption of alcohol can lead to gastric mucosal inflammation but also to the so-called Mallory-Weiss Syndrome lead through violent Vomit and choking, tears in the stomach lining can occur.
These tears can to 5-10% also cause stomach bleeding. Also dilated gastric vessels (Gastric varices; Fundic varices), which in various diseases of the spleen and the liver are potential sources of bleeding.
One of the less common causes is around 1% benign or malignant stomach tumorswhich can destroy gastric vessels as they grow. On the other hand, vascular malformations in the stomach wall (Angioplasia) lead to bleeding if they open by themselves or are accidentally injured by sharp-edged food components.
Further information on this topic can be found at: Stomach cancer
Stress as a cause
Both short-term, severe stress (e.g. major surgical interventions, Burns, Blood poisoning, shock, Multiple trauma, psychological distress), as well as long-term chronic stress, are major risk factors for the development of Inflammation of the gastric mucosa and Stomach ulcerwhich may lead to stomach bleeding. The reason for this is the increased production and distribution of Stress hormones (Adrenaline, norepinephrine) from the adrenal glands (Adrenal medulla), which takes place in acute stressful situations and i.a. leads to vasoconstriction in the gastric mucosa and increased production of gastric acid that is aggressive to the mucous membrane.
The resulting reduced blood flow and the beginning of self-digestion of the mucous membrane of the stomach can result in an inflammatory change and destruction of the stomach wall. The body usually reacts to chronic stress with a decreased immune system, one permanently high blood pressure, one delayed wound healing, increased tiredness and Poor concentration, physical impairment, Loss of libido such as Stomach and intestinal problems. The latter, however, does not arise from increased stress hormone production, as is the case with acute stress, but rather from increased stress Cortisone release from the adrenal glands (adrenal cortex), which leads to reduced mucus formation in the gastrointestinal tract.
This mucus, which is normally responsible for neutralizing gastric acid, is only produced to a reduced extent or is completely absent, so that the protective barrier of the gastric mucous membrane is lost. Here, too, the result is an increasing destruction of the mucous membrane, which can turn into inflammation, ulcers and bleeding. Furthermore, the gastrointestinal problems are among Constant stress also due to the fact that the gastrointestinal tract is less supplied with blood in order to supply all blood and energy reserves to the organs that are increasingly stressed under stress (Heart, lungs, muscles, brain) to be able to send. The result is decreased gastrointestinal activity, leading to a wide variety of symptoms, such as nausea, Vomit, constipation or even diarrhea can lead.
Alcohol as the cause
In addition to the known damage to the liver and its secondary diseases, increased alcohol consumption over a long period of time can also damage the stomach. Along with nicotine and some medications, alcohol is one of them toxic substanceswhich can irritate and damage the lining of the stomach.
In the course of the disease it can lead to an acute or chronic course Inflammation of the stomach lining or even gastric ulcer formation. Both diseases can lead to the opening of blood vessels due to the progressive destruction of the gastric mucosa or stomach wall, leading to bleeding in the stomach.
In addition, gastric bleeding can also be caused by the so-called Mallory-Weiss Syndrome which occurs more frequently in patients with a long-term history of alcohol consumption and who have already damaged the gastric mucosa. Does it become too strong in the context of excessive alcohol? Vomit and / or choking, the associated increase in pressure in the stomach can lead to tears in the mucous membrane in the transition area between the stomach and the esophagus. If the stomach vessels are injured or ruptured, this can trigger light to heavy bleeding.
Medicinal causes
The Taking some medication or the combination of certain drugs to go with one for a long period of time increased risk of gastrointestinal or gastrointestinal bleeding hand in hand.
Bleeding in the gastrointestinal tract is increasingly associated with so-called NSAIDs (Non-steroidal anti-inflammatory drugs). In addition to an analgesic effect, they also have an anti-inflammatory effect.
Typical representatives from the group of NSAIDs are Ibuprofen®, Diclofenac®and Naproxen®such as aspirin® (Acetylsalicylic acid).
Besides the regular intake also plays the Dosage amount an important role in the occurrence of side effects.
Inflammatory changes in the mucous membrane and Ulcers are among the complications, but also more serious ones like the one mentioned Bleeding or Perforations in the stomach and intestines and Closures these include.
In general, the Ingestion increases the risk of side effects, the serious complications are rare.
In the case of diclofenac, such a side effect has been observed in around 3 patients out of a total of 1000 after taking 150 mg daily.
Mode of action of nonsteroidal anti-inflammatory drugs
The above NSAIDs (Non-Steroidal Anti-Inflammatory Drugs), which are anti-inflammatory pain relievers, include both Aspirin® (Active ingredient: acetylsalicylic acid / ASA), as well as Voltaren® (Active ingredient: Diclofenac).
Their mode of action is identical, both inhibit enzyme, which is mainly responsible for the formation of Tissue hormones (Prostaglandins) is.
These tissue hormones are i.a. significantly involved in the development of pain and inflammation. A major side effect of long-term intake of aspirin / Voltaren in relation to the gastrointestinal tract is that it is also produced by the gastrointestinal mucous membrane Tissue hormone E2 (prostaglandin E2) is inhibited in its education.
This means that the gastric mucous membrane in particular can produce less neutralizing mucus than before aggressive stomach acid protects.
The consequence is a significantly increased risk for Inflammation of the gastric mucosa and the formation of Stomach ulcer (Gastric ulcer), whereby both diseases can lead to gastric bleeding through the destruction of gastric wall vessels. However, the risk of bleeding depends on the dose and length of drug therapy. Increase e.g. 75mg ASA 2 times the risk, 150mg already 3 times the risk.
Gastrointestinal bleeding from ibuprofen
Ibuprofen belongs to the group of non-steroidal anti-inflammatory drugs and has a pain relieving, anti-inflammatory and antipyretic effect.
In addition to this, it also reduces the production of mucus in the stomach and thus increases the risk For Mucosal damage.
The risk within a year serious complication such as gastrointestinal bleeding to suffer is according to a study daily intake of 2400mg ibuprofen at around 1%.
In general, such side effects more common in elderly patients to be watched.
Find out more about Ibuprofen®
Gastrointestinal bleeding from aspirin
aspirin with the active ingredient acetylsalicylic acid also belongs to the group of non-steroidal anti-inflammatory drugs and lowers the risk of cardiovascular diseases such as heart attacks.
It reduces the likelihood of platelets clumping together in the vessels.
According to one study, daily intake of 1200mg ASA is a risk from less than a percentt one Gastrointestinal bleeding to suffer.
At long-term use of aspirin, should, especially when combined with other antithrombotic drugs, always a stomach protection (proton pump inhibitor) be prescribed.
Read about this under
- Aspirin®
- Proton pump inhibitors
Raised pressure in the stomach as the cause
Another cause is that, with a share of 10% in the bleeding of the upper gastrointestinal tract (gastrointestinal tract), it is rather rare Mallory Weiss - lesionin which there is a rise in pressure in the stomach, e.g. with strong Vomit, bleeding tears in the lower esophagus.
Esophageal varices as a cause
The varices account for 20% of the bleeding (Varicose veins) of the esophagus (Esophagus), which arise when blood flows through the liver as a result of which connective tissue is disturbed through excessive consumption of alcohol (medical Cirrhosis of the liver):
Instead of the direct route to the ins heart leading, lower Vena cavaTo take, the blood flows through now more stressed bypasses - the veins of the esophagus (medical: collateral circulation is formed).
The pathologically enlarged veins are called varices and can lead to potentially fatal bleeding.
Among those associated with an increased risk of bleeding Medication belong aspirin (As it causes the formation of blood clotting substances in the platelets, the Platelets, inhibits) and other related drugs that lower pain and fever, i.e. which also belong to the as NSAIDs (= not-steroidal A.nti-R.heumatika), counting preparations.
Also the anticoagulants (medical term for blood coagulation inhibitors) administered specifically to inhibit blood clotting, to which e.g. Phenprocoumon (Trade name: Marcumar), Coumadin (trade name: Warfarin) and the Heparins (e.g. Liquemin, Fragmin) count, can lead to gastrointestinal bleeding, especially in the event of an overdose.
The causes listed above usually lead to one in the upper gastrointestinal tract (gastrointestinal tract), which by definition is not the only one esophagus and stomachbut also the first section of the small intestine is counted, localized bleeding.
Age-related causes
The most common causes of bleeding located in the lower GI (gastrointestinal) tract are age-dependent.
Suffer younger Patients up to 30 years a bleeding of the bowel, so is most likely one than Meckel's diverticulum designated, congenital malformation, responsible for it.
This is an approximately five centimeter protuberance of the small intestine, located 60-90 centimeters in front of the valve that separates the small and large intestines.
(The valve is called ileocecal valve after the intestinal sections separating it; the caecum - old spelling: Coecum - means nothing other than gastrointestinal bleeding, which is better known in the population. The function of the ileocecal valve, also known as Bauhin's valve, is to prevent it of backflow of intestinal contents from the heavily colonized with bacteria Large intestine in the Small intestine).
Most of them located in the upper small intestine Meckel's diverticulum often do not cause discomfort; however, in half of those affected the diverticulum contains (in the context of embryonic development) dislocated Gastric mucosa or other tissue, which in addition to bleeding also leads to long-lasting pain, bloating, Digestive problems and inflammation up to the potentially life-threatening occlusion of the intestine (medical: mechanical ileus).
The bleeding is caused by the production of aggressive hydrochloric acid by the gastric mucosal area.
The acid then corrodes the surrounding tissue and vessels, causing bloody erosions (superficial tissue defects) and ulcers (deep tissue defects that often extend into the muscles).
At Patients up to 60 years are bleeding diverticula of the colon mucosa, i.e. Protrusions of the intestinal mucosa through the outer layer of connective tissue (medical: serosa) that covers the entire intestine, the most common cause of gastrointestinal bleeding (gastrointestinal bleeding).
The exact mechanism of formation of the large intestinal diverticula, which in multiple occurrences of the "diverticulum disease" (medical: Diverticulosis) is unknown.
Presumably, a low-fiber diet and lack of exercise promote the formation of diverticula. Vascular malformations (angiodysplasias) are the most common source of bleeding in people over 60.
See also: Diseases in the blood
Symptoms / complaints
The complaints that occur are usually uncharacteristic:
Kick it;
- nausea
- Bloating and
- Pain in upper abdomen.
In the case of sharp pain in the right upper abdomen or below the costal arches (medical: epigastrium), a perforating injury should be considered as a typical cause.
Further sequelae of gastrointestinal bleeding (gastrointestinal bleeding) are direct consequences of heavy bleeding and their extent is also determined by the level of blood loss.
The lack of volume results in:
- to accelerate the heartbeat (tachycardia) and
- Restlessness
- to headache
- Dizziness and
- Cold perspiration.
In extreme cases, the severe blood loss can lead to (volume deficiency) shock.
Blood losses from approx. 20% of the normal blood volume are life-threatening. Typical of the upper gastrointestinal bleeding is the vomiting of bloody stomach contents, which is known as hematemesis (emesis = vomiting, Greek häma = blood) and never occurs with the lower gastrointestinal bleeding (gastrointestinal bleeding).
The color of the vomit gives the doctor further clues as to the location of the source of the bleeding:
If the blood has come into contact with the hydrochloric acid in the stomach, the vomit takes on a black color, often described as "coffee grounds", as a result of the chemical reaction of the blood pigment heme with the hydrochloric acid to form a product called hematin. If the blood does not come into contact with salt acid, e.g. If you have bleeding from the esophagus, the vomited blood is bright red (if it comes from an oxygenated artery) or dark red (venous blood).
If the blood drains into the intestines from a source of bleeding in the stomach, upper gastrointestinal bleeding can also lead to the passage of bloody stools. Here, too, a distinction is made between stool black due to hydrochloric acid (medical: melena, in German: tarry stool) and red blood deposited on the stool, also known as hematochezia.
Both symptoms occur - contrary to what one might initially assume when blood leaks from the intestine - more frequently in the upper than in the lower gastrointestinal bleeding (gastrointestinal bleeding).
The pervasive smell and sticky, shiny appearance of tarry stools are noticeable, which make it easier for the doctor to distinguish them from other, possibly similar-looking excretions (black-colored stools do not have to be gastrointestinal bleeding - this also occurs when coal or bismuth are ingested - or iron-containing drugs and has even been described after consuming blueberries).
It should be noted that the discontinuation of tarry stools always indicates that the bleeding has started in the past: the blood must have been in the intestine for at least eight hours.
Read more at: Blood in the stool such as Black bowel movements
Pain discomfort
In most cases, as described above, gastric bleeding is not noticed until vomiting of blood (Hematemesis), black colored stool (Tarry stool) or even blood-deficient circulatory disorders (Volume depletion shock) occur.
Lighter and chronic gastric bleeding can even go unnoticed for a long time and is then only discovered by chance during routine medical examinations. The connection between the occurrence of epigastric pain as an alarming sign and the actual existence of bleeding is not always necessarily given.
The reason for this is that the bleeding itself does not cause any pain, so that bleeding cannot only be assumed if symptoms occur in the left or middle upper abdomen. Rather, it is more likely to result from gastric mucosal inflammation (gastritis) and stomach ulcers (Gastric ulcer) to an irritation of the nerves with corresponding painful sensations, whereby both diseases lead to gastric bleeding and can therefore precede it.
Pain in the epigastric region is more likely to be viewed as a symptom of underlying gastric diseases with a potential for bleeding, although the bleeding does not have to be present at the time of pain.
In addition to left-sided or middle upper abdominal discomfort, gastric mucosal inflammation can also be symptomatic of nausea, belching and a feeling of fullness.
Noticeable stomach ulcers are mainly felt as dull and boring pain immediately after eating.
These typical symptoms, both for gastric ulcers and for gastric mucosal inflammation, are described by only about 50% of all patients, while these diseases also go unnoticed in the other half.
It is also important that not every pain in the epigastric region is a direct sign of gastric diseases.
Left-sided and middle upper abdominal pain can also be symptoms of a number of other abdominal diseases, such as diseases of the duodenum (e.g. Duodenal ulcer), on the pancreas (e.g. Pancreatitis), the spleen (Splenic infarction, ruptured spleen) or the kidneys or the urinary system (Kidney stone, ureteral stone, pelvic inflammation).
Classification of gastrointestinal bleeding
Basically one differentiates between one upper and one lower Gastrointestinal bleeding.
The upper gastrointestinal tract is made up of the stomach, the upper sections of the stomach Small intestine, so that Duodenum (medical: duodenum) and the transition to the jejunum, which is called "flexura duodenujejunalis".
The reason for this division into upper and lower gastrointestinal bleeding (GI bleeding) on the basis of the flexura duodenujejunalis is due to the doctor's different approaches to diagnosis and therapy:
To prove a upper gastrointestinal bleeding (GI bleeding) Endoscopes (Tube camera) used by the patient over the mouth (after the administration of a sedating, i.e. calming drug such as midazolam, which belongs to the short-acting benzodiazepines), pushed into the stomach and enables the doctor to look into the patient's digestive system up to this transition point between the two sections of the small intestine (flexura duodenujejunalis).
Is the presumed Source of bleeding at a Intestinal bleeding yet deeper (medical: further distal, towards the anus), the device must over the intestines be introduced. I.e. a reflection of the colon, a so-called Colonoscopy which also reaches the last and third section of the small intestine, the ileum, also known medically as the ileum.
It should be noted that this classification is still useful today, since the upper and lower gastrointestinal bleeding (gastrointestinal bleeding) clearly differ in terms of causes, the age groups affected and also in the choice of treatment method, but the The original origin of the classification is now only of limited validity due to more modern endoscopes with a larger range.
How is gastrointestinal bleeding diagnosed?
The diagnostic procedure depends, as just described, on the type of Gastrointestinal bleeding:
When Tarry stool after questioning the patient about the possible course of events (known previous illnesses or risk factors, medication taken, possible injuries, meals last taken, etc.) to diagnose bleeding in the upper gastrointestinal tract (Gastrointestinal tract) in an emergency endoscope (Hose camera) introduced.
Can gastrointestinal bleeding can be excluded there, the source must be in Large intestine or Small intestine to be found.
Evidence is provided by giving radioactively labeled red blood cells (the process aimed at detecting the emitted radioactive radiation is known as scintigraphy).
Then the selective diagnosis of the affected vesselswhich enables a more precise localization.
The value is controversial one carried out as an emergency, i.e. without appropriate preparation of the bowel Colonoscopy (Colonoscopy), since the informative value of a bowel that has not been previously cleaned with laxatives is limited and the examination is technically difficult.
The procedure for Vomit of blood (Hematemesis) is similar to settling tar stools; in the case of massive bleeding, however, an immediately emergency surgery displayed.
Is that passed stool, red arterial blood (Hematochezia), is often used with the digital rectal diagnosis (Examination of the anus with a finger) started because the examiner's finger can feel palpable neoplasms (Neoplasms) and tissue injuries (ulcerations) as well as hard blood clots hemorrhoidscan quickly determine.
If this measure does not lead to success, the following examination procedures include endoscopy (in this case a Endoscopy of the rectum, also known as the rectum, one speaks of a rectoscopy) and the visualization of the vessels with contrast media (angiography) or radioactively marked substances (scintigraphy).
Read more about the topic here Angiography