Myelography
Synonyms
Contrast agent display of the spinal canal (syn. Spinal canal).
definition
Myelography is an invasive (injurious to the body) diagnostic X-ray procedure for the clarification of back pain if there is a suspicion that the cause of the complaints is related to a pressure (compression) of the spinal cord (myelon) or the spinal cord / spinal nerves and other modern ones Imaging tests, such as magnetic resonance imaging (MRI) of the back, are not sufficient to make the diagnosis.
The principle of myelography consists in injecting an X-ray contrast medium into the spinal canal (subarachnoid space) to show the spatial conditions for the spinal cord and the spinal cord nerves / spinal nerves.
Please also read our page Back pain diagnosis.

indication
Various diseases of the Spine can give cause for myelography to be performed. What they all have in common is that there is a suspicion of nerve damage in the spinal canal. Mostly these are diseases in the context of the general aging process (degenerative spinal diseases) of the spine, which is comparable to the signs of wear and tear of the large body joints (Knee osteoarthritis, Hip osteoarthritis) you can see.
Read about it too Diagnosis of spinal disease.
Bone extensions, intervertebral disc material and ligament structures in the spinal canal can lead to an increasing narrowing of the spinal canal (Spinal stenosis). Up to a certain degree of constriction, the nerve fibers get used to the restricted space. At some point, however, the space is so tight that pressure-related nerve damage occurs, which is noticeable in pain, weakness and discomfort in the arms or legs.
In other cases, there may also be an isolated narrowing in the area of one or more nerve root exit holes (neuroforamen stenosis). The spinal cord tube is not pressured as a whole, but only individual spinal cord nerves / spinal nerves. Depending on which spinal cord nerves are affected, there may be symptoms of back pain that is transmitted to the leg or arm (Lumboischialgia, Cervicobrachialgia).
In all of these cases, myelography can provide further diagnostic help, if despite one Magnetic resonance examination of the lumbar or cervical spine (MRI) should still remain unclear. Myelography is often used to plan the extent of surgery in spinal surgery (Spinal fusion, Decompression).

- Spinal cord
- Spinal stenosis
- Vertebral bodies
- Intervertebral disc
preparation
Before one Myelography some preparation is necessary. The doctor is obliged to thoroughly inform the patient about the type and necessity of the examination. He must also inform him of the general and intervention-specific risks. The patient, in turn, must give written consent to myelography at least one day before the examination. Blood is also taken no later than the day before the examination and, above all, controls those blood values that are important for normal blood clotting. All blood thinning drugs (e.g. ASS 100 ®, Plavix ®, Godamed ® must be discontinued in good time (approx. 7 days) in order to avoid an increased risk of bleeding.
Most often, a normal x-ray of the spine is available prior to performing the myelography. This enables the doctor to determine the best access to the spine for the injection of the X-ray contrast agent.
In the medical history of the patient must look for thyroid disorders such as one Hyperthyroidism (Hyperthyroidism), because an iodine uptake from the iodine-containing X-ray contrast medium would otherwise lead to a dangerous metabolic derailment of the thyroid can come.
It is also important to clarify in advance whether a allergic to iodine because an allergic reaction to the contrast medium is severe Circulatory shock can cause (anaphylactic shock).
For reasons of hygiene, the patient is given on the day of the Myelography put on a surgical shirt. In addition, an intravenous access is established. This is mainly used to be able to give medication and fluids quickly via the vein in the event of allergic reactions or other circulatory reactions.
The implementation of the myelography itself is carried out in the X-ray department of the clinic.
Procedure of myelography
Myelography is usually done in the lumbar spine area.
The patient sits or lies down. In a sitting position, he is asked to bend forward and stretch the lower part of his back towards the doctor. In the lying position, the feet should be drawn up in order to also achieve a hunched back position. This type of storage spreads the vertebral bodies apart in the rear area. This makes it easier for the doctor to get into the spinal canal between the spinous processes of the vertebrae.
The height of the puncture is then determined. The doctor orients himself here on the x-ray of the lumbar spine, the palpable findings of the spinous processes and on typical anatomical conditions (landmarks), such as the iliac crest height. The skin is then thoroughly disinfected.
Prepared in this way, the puncture itself is not perceived as painful by the patient. If desired, the puncture site can be numbed through a very thin needle with a local anesthetic before the puncture.
After the puncture, the doctor pushes the myelography needle (cannula) towards the spinal canal (spinal canal). The doctor recognizes that the spinal canal is reached by a backflow of nerve water (liquor). A small amount of nerve water is often given to the laboratory for further investigation.
An injury to the spinal cord itself is not to be expected during the puncture. The spinal cord as a structural unit ends at the level of the 1st-2nd Lumbar vertebrae. Underneath, the individual spinal cord nerves, floating freely in the nerve water of the spinal cord (cauda equina), continue in the direction of the nerve exit holes in the lower lumbar spine area intended for them. When the spinal cord tube is punctured, the spinal cord nerves are easily displaced by the needle. There is no injury to the nerves.
Then 10-20 ml of a water-soluble X-ray contrast medium are injected. This is distributed in the spinal cord tube (dura tube) and flows around the spinal cord nerves until they leave the spine through their nerve exit holes. The exit of the spinal cord nerves is also flowed around for a short section. Wherever there are bony, intervertebral disc or other constrictions, the contrast medium flow is diverted or interrupted.
After the injection of the contrast medium, the X-ray images are taken:
- Classic x-ray of the lumbar spine from the front (a.p.) and from the side: the distribution of the contrast medium shows the width and space of the spinal cord space. The spinal cord nerves appear as contrast medium recesses.
- Oblique x-rays of the lumbar spine lying on the right and left: The outflows of the spinal cord nerves from the spinal canal can be clearly seen on these images.
- Functional images of the lumbar spine in forward and backward flexion (lateral images): These x-ray images allow a statement to be made about the extent to which the forward and backward flexion of the upper body has an influence on the space available in the spinal canal. For example, during prevention (anteflexion / inclination) an intervertebral disc can bulge clearly visibly in the direction of the spinal cord space and cause nerve pain, while in a straight position it appears completely inconspicuous. In the clinical picture of spinal canal stenosis with spinal instability, on the other hand, the full extent of the spinal canal narrowing and nerve crowding becomes apparent, especially when the patient is bent back (retroflexion / reclination).
- Myelo - CT: This is a computed tomography (CT) following the myelography. This cross-sectional image process, in combination with contrast agent injection, provides the most detailed images for assessing spinal canal stenoses and nerve pressures. Due to the strong contrast after the injection, nerves can be separated from other types of tissue with millimeter precision. A three-dimensional image can also be created using Myelo-CT.
- Myelo - MRT: Here, following the myelography, an MRI of the lumbar spine is performed.
Following the myelography, the patient is brought back to the ward. In order to avoid persistent headaches due to the temporarily changed pressure conditions in the nerve water space (liquor space), bed rest must be maintained for 24 hours. In addition, you should drink a lot so that the loss of nerve water is compensated for as quickly as possible.
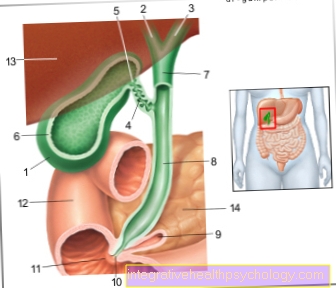
- Nerve root branch L4
- Nerve root branch L5
- Nerve root exit S1
- Spinal cord tube with nerve fluid and spinal cord nerves / spinal nerves
Myelography of the cervical spine
Myelography is used to clarify many different complaints in the area of the spinal canal. When examining the cervical spine (Cervical spine), these complaints often manifest in the area of the upper extremities (arms, shoulders). The patient often complains of radiating pain, paralysis and numbness. A common cause of these symptoms are masses (spinal canal stenoses) in the area of the cervical spine. This compresses and irritates the surrounding structures (especially nerves). These masses often occur in the course of herniated discs, tumors and other spinal cord injuries. Bony changes in the area of the spine can also pinch the nerve roots and narrow the nerve exit openings. With the help of the injected contrast agent in myelography, these masses can be clearly demarcated from the surrounding structures and diagnosed. In rare cases, during myelography of the cervical spine, the contrast agent is injected directly into the neck area instead of the lumbar area.
Lumbar spine myelography
In addition to examining the cervical spine, myelography can also be used to diagnose complaints in the lumbar spine area. The patients often report similar symptoms (radiating pain, paralysis, numbness), but this occurs mainly in the Lower extremity (legs) and pelvic area. In this case, too, the causes of these complaints are often masses in the area of the spinal canal, which compress and irritate the surrounding nerves. By administering a contrast agent, these masses can be clearly distinguished from the surrounding structures and diagnosed. Possible space occupations can arise from herniated discs, tumors, bone changes or further spinal cord injuries.
Performing myelography

A Myelography is mostly used in the Lumbar spine carried out.
The patient is with the Sitting or lying down myelography. In a sitting position, he is asked to bend forward and stretch the lower part of his back towards the doctor. In the lying position of the Myelography the feet should be drawn in to achieve a hunchback position as well. This type of storage spreads the vertebral bodies apart in the rear area. This makes it easier for the doctor to get into the spinal canal between the spinous processes of the vertebrae.
The height of the puncture is then determined. The doctor orients himself here on the X-ray of the Lumbar spine, the palpable findings of the spinous processes as well as typical anatomical conditions (landmarks) such as the iliac crest height. The skin is then thoroughly disinfected.
Prepared in this way, the puncture itself is not perceived as painful by the patient. If desired, the puncture site can be numbed through a very thin needle with a local anesthetic before the puncture.
After the puncture, the doctor pushes the myelography needle (cannula) towards the spinal canal (spinal canal). The doctor recognizes that the spinal canal is reached by a backflow of nerve water (liquor). A small amount of nerve water is often given to the laboratory for further investigation.
Having an injury to the spinal cord itself is associated with the Myelography not to be expected. The Spinal cord as a structural unit ends at the level of the 1st-2nd Lumbar vertebrae. The individual spinal cord nerves run underneath, floating freely in the nerve water of the spinal cord (Cauda equina), continue in the direction of the designated nerve exit holes in the lower lumbar spine area. When the spinal cord tube is punctured, the spinal cord nerves are easily displaced by the needle. There is no injury to the nerves.
Then 10-20 ml of a water-soluble X-ray contrast medium are injected. This is distributed in the spinal cord tube (Dural tube) and flows around the spinal cord nerves until they leave the spine through their nerve exit holes. The exit of the spinal cord nerves is also flowed around for a short section. Wherever there are bony, intervertebral disc or other constrictions, the contrast medium flow is diverted or interrupted.
Still the contrast agent injection will be the X-rays prepared:
- Classic x-ray of the Lumbar spine From the front (a.p.) and from the side: The width and spatial conditions of the spinal cord space are shown on the basis of the distribution of the contrast medium. The spinal cord nerves appear as contrast medium recesses.
- Oblique x-rays of the lumbar spine lying on the right and left: The outflows of the spinal cord nerves from the spinal canal can be clearly seen on these images.
- Functional images of the lumbar spine in forward and backward flexion (lateral images): These x-ray images allow a statement to be made about the extent to which the forward and backward flexion of the upper body has an influence on the space available in the spinal canal. For example, during prevention (anteflexion / inclination) an intervertebral disc can bulge clearly visibly in the direction of the spinal cord space and cause nerve pain, while in a straight position it appears completely inconspicuous. In the clinical picture of spinal canal stenosis with spinal instability, on the other hand, the full extent of the spinal canal narrowing and nerve crowding becomes apparent, especially when the patient is bent back (retroflexion / reclination).
- Myelo - CT: This is a Computed Tomography (CT) following myelography. This cross-sectional image process, in combination with contrast agent injection, provides the most detailed images for assessing spinal canal stenoses and nerve pressures. Due to the strong contrast after the injection, nerves can be separated from other types of tissue with millimeter precision.
Following the Myelography the patient is brought back to the ward. In order to avoid persistent headaches due to the temporarily changed pressure conditions in the nerve water space (liquor space), bed rest must be maintained for 24 hours. In addition, you should drink a lot so that the loss of nerve water is compensated for as quickly as possible.
- Nerve root branch L4
- Nerve root branch L5
- Nerve root exit S1
- Spinal cord tube with nerve water and Spinal nerves / Spinal nerves
Can myelography be performed on an outpatient basis?
Myelography is usually done on an inpatient basis. This is because patients need to be monitored for at least 4 hours after the examination and bed rest is required. Depending on the patient, a one-day follow-up treatment may also be necessary.
Nevertheless, more and more clinics are offering myelography as an outpatient diagnosis. In this case, the patient must be informed about possible risk factors and information in a preliminary meeting. Anticoagulant drugs should be discontinued a few days before the examination in most patients. In addition, the patient should come to the appointment sober. After the examination and four-hour monitoring, the patient is prohibited from driving a car or using machines.
Pain
Myelography is a low-risk, routine procedure. Only injecting the contrast agent in the lumbar region (between L3 and L4) can pose risks to the patient.
A rare complication is the occurrence of pain during the examination. This occurs as a result of an injury to nerve fibers during the puncture with the myelography needle. Patients often report headaches and back pain. In addition, the damage to the nerve can also cause sensory disturbances and paralysis. Depending on the patient, the symptoms can persist for a few days after the examination, but in most cases they subside completely.
Headaches can also result from the additional withdrawal of liquor fluid during the examination. The reduced CSF content compensates for the expansion of the vessels that supply the meninges, which causes headaches in the patient.
Contrast media
Myelography is typically done using x-rays. To better separate the spinal cord from the surrounding liquor space, an iodine-containing contrast agent is injected into the latter. This creates a stronger contrast between the spinal cord and the liquor space. Possible spatial demands can thus be better represented.
Carrying out a myelography is therefore not possible with a known allergy to substances containing iodine. There is a risk of severe allergic reactions. In addition, the functionality of the thyroid gland should always be checked before the examination, as iodine is an important starting substance for the production of thyroid hormones.
Complications
Complications from myelography are very rare. The most common "complication" is the temporary headache. Serious complications can occur:
- Post-bleeding: In the worst case, if a blood vessel is injured, bleeding into the spinal canal is possible (epidural hematoma), which can damage the spinal cord nerves.
- Nerve injury: Incorrect placement of the myelography needle can injure outgoing spinal cord nerves. These cannot avoid the needle because they no longer swim in the nerve water. Pain, sensory disturbances and paralysis can result.
- Infection: The spread of germs (bacteria) can cause both a superficial and a deep infection of spinal structures (intervertebral discs, vertebrae, spinal cord). In the worst case, it can lead to an inflammation of the spinal cord (meningitis).
- Continuous loss of nerve water: If the puncture site of the spinal cord membrane (dura) does not close by itself, as is usual, nerve water can continuously seep outwards. Surgical intervention with closure of the hole is then often necessary.
- Allergic reaction: An allergic reaction to the contrast medium can, in extreme cases, lead to an allergic shock (cardiac arrest).
- Thyroid dysfunction: The uptake of the iodine in the X-ray contrast medium into the thyroid gland can lead to dangerous hyperthyroidism in certain cases.