Epididymis
introduction
The epididymis (Epididymis) is used for sperm cell maturation and storage of the mature sperm cells. It is also part of the executing seminal ducts.
It is divided into three parts and lies on the testicle.

Development of the epididymis
The development of the epididymis is directly related to the development of the testes and kidneys. It develops in the embryonic period from the Wolff gait, after the genetic determination of the sex has taken place.
Function of the epididymis
The epididymis is Place of sperm maturation and serves as Stores of mature sperm cells.
In addition, the epididymis is also Part of the executing seminal ducts, as the sperm are transported from the testes through parts of the epididymis and the epididymal duct.
Structure of the epididymis
The epididymis lies above the testicle and is slightly shifted backwards (craniodorsal).
It is over an upper and a lower band (Ligamentum epididymis superior and inferior) connected to the testicle.
The testicles and epididymis are covered by various muscle fasciae.
There is a small gap between the two structures, which is called Epididymid sinus referred to as.
The epididymis is formed by many small executive ducts (Efferent ducts) and the epididymal duct (Ductus epididymidis) built up. These are very tightly bundled together, in the extended state the epididymis is approx. 5 m long, a small ductus efferens approx. 20 cm long.
The epididymis is divided into three parts:
- The epididymal head (Caput epididymidis) lies on top of the testicle and contains 10-20 small ducts (ductuli efferentes) as well as the beginning of the epididymal duct.
- The body of the epididymis (Corpus epididymidis) rests on the testicle mainly from behind (dorsal). Sperm storage takes place in this part.
- The tail of the epididymis (Cauda epididymidis) is also the place of sperm storage.
Through contractions of the muscles of the epididymal duct, the sperm cells are then transferred into the subsequent sperm duct (Deferens duct) submitted.
The diameter and lumen of the epididymis decrease downwards (caudally).
The mucous membrane of the epididymal duct consists of a two-row epithelium and branched Sertoli cells; the wall also contains smaller myofibroblasts, which serve to contract the duct.
Microscopically, the smaller efferent ducts show an irregular, undulating lumen. These are also surrounded by a shell made of contractile myofibroblasts.
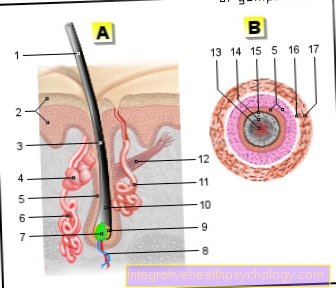
Illustration of the testes and epididymides

Testicles and epididymis
- Testicles - Testis
- Epididymis - Epididymis
- Scrotum - scrotum
- Epididymis -
Cauda epididymidis - Epididymis -
Corpus epididymidis - Vas deferens -
Deferens duct - Urinary bladder -
Vesica urinaria - Tendril vein plexus -
Pampiniform plexus - Testicular artery -
Testicular artery - Epididymis -
Caput epididymidis - Connective tissue cover -
Tunica albuginea - Testicular walls -
Septula testis - Testicular lobe -
Lobuli testis
You can find an overview of all images by Dr-Gumpert at :medizinische images
Ducts
The arterial supply of the epididymis occurs through the Testicular artery, the venous blood outflow takes place via the Pampiniform plexus. This is a plexus of veins that is formed by the small testicular veins.
From there the blood continues to flow over the Testicular veins (V. testicularis dexter and sinister) in the lower great vena cava (Inferior vena cava).
The nerve innervation takes place like with the testicle over the Celiac plexuswhose fibers run together with the arterial vessels. These fibers form a network of nerves near the kidney and from there they come to the testicles and epididymis.
The parasympathetic fibers pull as vegetative fibers to the epididymis. There all nerve fibers together form the Testicular plexus and innervate the testes and epididymides.
Diseases of the epididymis
Inflammation of the epididymis
With epididymitis, too Epididymitis called, there is an inflammatory process within the epididymis due to various possible causes. This disease occurs preferentially in men over 30 years of age and is the cause of a so-called "acute scrotum" in children only in about 2% of the cases enter the urethra mainly as a result of urinary tract infections or during sexual intercourse. In addition to ascending causes, the inflammation can also develop via the blood, lymph, epididymal tubules, post-traumatic, immunological or viral (especially mumps). In children there are usually anomalies of the urogenital system, such as urethral valves , False mouths or a "neurogenic bladder", reason for the disease.
Epididymitis is an acute event that usually worsens significantly within a single day and thus becomes symptomatic. Above all, increasing pain in the scrotum (scrotum), which can radiate into the groin, abdomen and flank. This usually leads to reddening and swelling of the scrotum (scrotum). Often a so-called positive "Prehn’s symbol" determine. This means that the pain will decrease as the affected testicle is raised. Often fever and fatigue are also possible. In the case of acute pain in the scrotal region, a urologist should be consulted quickly in order to rule out "testicular rotation". Epididymis is treated primarily by lying up, cooling, strict bed rest and applying an ointment. In addition, antibiotics and / or local painkillers can be injected.
Read more on the subject below: Epididymitis
Causes of a swollen epididymis
Since the epididymis rests directly on the testicle and is in connection with it, it is important to define whether the testicles, the epididymis or both are affected when pain or swelling is present. This can often be difficult to assess and should be clarified by a doctor. The most common reason for swelling in the epididymis is the epididymitis described above. This can also occur in connection with an inflammation of the testicles and is then called "Epididymo orchitis" designated. Other possible causes besides inflammation are cysts (Spermatocele), Abscesses, varicose vein hernia (Varicocele), Water break (Hydroceles), Thromboses, tumors, hernias, a twisted testicle or sperm granulomas. A sperm granuloma is a hard, nodular change in the spermatic cord that is caused by the leakage of spermatozoa into the surrounding tissue.
Read more on the subject below: Inflammation of the testicles
There are several criteria that can be used to differentiate between these various causes. If pain occurs in addition to swelling, it is most likely an inflammatory process, an abscess, a thrombosis, a tumor or a gangrene (Tissue necrosis). In addition, a further differentiation is possible by precisely feeling the swelling. The most important thing is where the swelling is located, how far it extends or whether it encompasses the whole testicle or only part of it and what consistency the swelling has. However, only a urologist is able to provide an exact diagnosis and should be consulted whenever a change is found.
Read more on the subject at: Epididymides are swollen - what's behind it?
Epididymal cyst
An epididymal cyst, also known as a spermatocele or "retention cyst", is caused by an obstruction to drainage within the epididymis. Since this is used for the transmission and maturation of the sperm at the transition from the testes to the spermatic duct, there is an accumulation of protein-containing sperm. Such an obstruction of outflow is usually caused by different or unusual course of the epididymal tubules, but can also be triggered as a result of surgical interventions or a past epididymis. Such an obstruction to the drainage and congestion of sperm is very common and can be found in around 80% of men. However, since it is only very small in the majority of cases, it usually does not cause any problems and is therefore discovered at most by chance. With a small proportion (5%), however, there is a strong increase in size, in which the cyst can also reach a diameter of over 10 cm. As the size increases, symptoms such as pain and pressure in the epididymis also appear. If an epididymal cyst is discovered by chance and appears symptom-free, no further therapy is necessary. However, if a spermatocele is noticeable because of pain or a feeling of pressure, surgical removal is indicated.
Read more on the subject at: Epididymal cyst
Epididymis pain
Epididymal pain is a very common symptom, which can often be acute, but also chronic. As with swelling of the epididymis, it is sometimes difficult to differentiate between testicles and epididymis, which is why a disease of the other organ can also be a cause. The most common cause of painful epididymis in adults is the epididymitis mentioned above. In children, the most common reason for a painful, acute scrotum is testicular torsion, which is an emergency and must be treated as quickly as possible. Other possible causes are abscesses, tumors, thromboses, external injuries or tissue necrosis. A reasonably good way to differentiate between inflammation and twisted testicles is the so-called "Prehn" test. In the case of inflammatory processes, when the affected testicle is lifted, pain relief is usually achieved (positive Prehn's sign). In addition to pain in the epididymis, there are often other accompanying symptoms, such as swelling, redness, rash, feeling of pressure or heaviness, as well as fever and weakness. A urologist should be consulted as quickly as possible in order to rule out a urological emergency or treat it in good time, especially in the case of pain that intensifies rapidly and / or occurs suddenly.
What happens if you remove the epididymis?
Surgical removal may be necessary in the case of chronic and recurring epididymis or a water breakage (hydrocele). Further reasons for a surgical resection are tumors, recurring inflammations and other rather rare causes, which are assessed individually by the respective urologist. When removing the epididymis (Epididymectomy) part of the vas deferens is often also removed in order to reduce the likelihood of postoperative complications (Epididymovasectomy). During the operation, the epididymis is removed with the help of a small incision in the scrotum. Since usually only one side is affected by the inflammation or the water break, there is compensation by the healthy side, which is why fertility and erection are not restricted. However, postoperative complications such as wound healing disorders or infections occur again and again during this procedure. There is also the risk of "descending" inflammation, which can mean that an additional removal of the testicle may be necessary afterwards.
Epididymal tumor
Epididymis cancer is a very rare disease compared to testicular cancer (about 10 times more common). This leads to a nodular change / swelling within the scrotum, which is usually noticed by the patient himself. Epididymal tumors tend to be slow growing, mostly painless tumors, which is why they can go unnoticed for a long time. To confirm the suspicion, an ultrasound is first performed. If a mass is found, the testicle and epididymis are exposed and a microscopic tissue examination is carried out in order to make an exact diagnosis and differentiation between benign and malignant possible.
Lump in the epididymis
A palpable nodular change in the epididymis can have many causes. Most often it is a cyst, abscess, or inflammation. In rare cases it can also be a tumor or a thrombosis. An important distinguishing feature is the existing painfulness, which is more indicative of inflammatory or thrombotic processes. However, a resilient, painless swelling is most likely to indicate a cyst (Spermatocele). In any case, a urologist should be consulted.
Summary
The Epididymis (Epididymis) is Part of the efferent seminal ducts and serves the Maturation and storage of the sperm cells.
It rests on top of the testicle and, together with the testicle, is bounded by various muscle fascia.
It is connected to the testicle by two ligaments. The epididymis consists of numerous small ducts (ductuli efferentes) and a larger excretory duct (Epididymis, Ductus epididymis).
It serves for the maturation and storage of sperm cells and passes them on to the sperm leader by contraction of the epididymal duct.
The vascular supply and nerve innervation take place together with the testes.