Operation of a lowering of the uterus
introduction
The decision on surgical treatment of a uterine subsidence is made based on various criteria. Among other things, the patient's level of suffering and the extent of the reduction play a role.
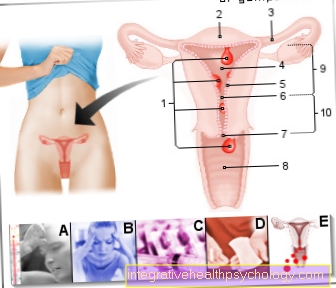
The most frequently used surgical method is the so-called vaginal hysterectomy with anterior and posterior pelvic floor surgery and perineal surgery. In most cases, this operation will also remove the uterus. Thus, this operation is only performed on women who have already completed their family planning.
If incontinence occurs due to the lowering of the uterus, this is also treated in the same operation.

When do you need an operation?
As a rule, the uterine subsidence is first treated with conservative measures. These include various preparations that contain the hormone estrogen, as well as structured training of the pelvic floor muscles or a normalization of body weight. If these measures do not achieve long-term success or if the uterine lowering is already too advanced, an operation may be necessary.
Read more on the subject at: Uterus subsidence
What are the different surgical methods?
The most common surgical method is removal of the uterus followed by a pelvic floor surgery. However, there are alternatives to this method. If the patient wishes to have children, the uterus must remain and only a pelvic floor surgery is performed. This operation is also performed if the uterus is slightly subsided or if the patient does not consent to the removal of the uterus.
If the vaginal stump subsides again after removal, a so-called abdominal sacrocolopexy is performed. In this surgical procedure, the vaginal stump is fixed to the bones of the sacrum with a mesh. This is to reduce the risk of a renewed sinking. In addition, there are numerous surgical methods that are used when the urinary bladder or the rectum sags.
OP with mesh
The transvaginal mesh insert is a newer surgical procedure, which is a promising alternative to the standard method. A mesh is inserted between the vagina and the urinary bladder through a surgical access in the vagina. This runs laterally to the outer edges of the pelvic floor muscles and thus offers a new support surface for the pelvic organs.
Over time, the network grows together with the surrounding structures. The operation to insert the mesh is short and has few complications. Since the mesh is a foreign body, there is a risk of repulsion, but this is low.
What preparations have to be made before the operation?
The operation is usually performed under general anesthesia. Only in exceptional cases is it carried out alone with a local anesthetic. Before a general anesthesia, there is always an informative conversation with an anesthetist, in which, among other things, the risks of the anesthesia and the medical history are discussed.
Immediately before the operation you have to be sober for the anesthesia. This means that you are not allowed to eat or drink anything a few hours beforehand. This will also be discussed with the anesthetist in the preliminary talk. Since the operation is carried out in the company of a hospital stay, the responsible gynecologists on the ward discuss the risks of the operation with the patient in advance of the operation and obtain their consent.
Procedure of the operation
In the most common surgical method, the uterus is removed through a vaginal access. This means that an incision in the abdominal area is not absolutely necessary. Excess vaginal tissue is then removed and the vaginal stump closed. This is fixed to the sacrum. This is followed by the pelvic floor plastic surgery (colporraphy).
The anterior pelvic floor surgery is mainly used when the urinary bladder is lowered in addition to the uterus. For this purpose, an incision is made in the anterior vaginal wall and it is detached from the urinary bladder. The ligaments that are in contact with the urinary bladder are gathered so that it comes to rest a little higher.
In the posterior pelvic floor surgery with perineal surgery, the posterior vaginal wall is detached from the rectum. This allows the tissue around the vagina to be gathered. In the next step, the muscles of the pelvic floor are connected to the muscles of the perineum. With these gatherings and connections, the stability of the holding apparatus should be increased again and thus prevent further subsidence.
Since this surgical procedure has a high risk of causing renewed subsidence, nets are used in newer surgical methods that are inserted into the pelvis. In women who want to have children, the uterus is left in place and only the holding apparatus and the pelvic floor muscles are gathered in order to achieve new stability.
Read more on the subject at: Operations on the uterus
How long does the operation take?
The duration of the operation depends very much on the surgical method and the scope of the operation. Nevertheless, it is a rather short operation that takes an average of 30 to 60 minutes. If the urinary bladder is also operated on to restore continence or if the uterus is completely removed, the operation time is extended.
What should I consider during follow-up care?
The hospital stay after a uterine dissection is usually no longer than a few days. Some complications of the operation, such as stress incontinence, may only arise later after the operation. Therefore, follow-up care after certain time intervals is very important.
In addition, in the follow-up care it can be examined whether it has come down again or whether an unnaturally prolonged discharge from the vagina can be observed.
How long do you lie in the hospital?
The hospital stay after the operation of a lowering of the uterus is usually short. On average, you can be discharged from the hospital three to five days after the operation. Of course, only if the patient feels well and there have been no complications in the course of the operation.
Above all, attention is paid to whether the patient has problems with urinating after the operation. This is a well-known complication of the operation, as the operation is also carried out in the immediate vicinity of the urinary bladder and this may cause problems with continence.
What are the risks?
The operation to lower the uterus is a procedure with few complications. A possible risk of the operation is the triggering of what is known as stress incontinence. This happens when the urinary bladder is positioned too high up during the anterior pelvic floor surgery. This makes the angle between the floor of the bladder and the urethra too steep so that the urine can no longer be held by the urinary bladder sphincters. Since incontinence can be very stressful for those affected, it is essential that this is recognized in the follow-up care and that the patient receives appropriate support.
Urination can also be difficult after the operation. In addition, pain during sexual intercourse can occur even after the surgical wounds have completely healed. General risks of an operation, such as rebleeding or infections, are possible, but rarely with the procedures. If the lowering of the uterus is based on a weak connective tissue, there is a risk, even after the operation, that the uterus could lower itself again or that the uterus or vaginal stump could be removed. The surgery only treats the symptoms, but cannot fix the weakness of the tissues.
Also read the article on the topic: Stress incontinence
What can the long-term consequences be?
Surgery to lower the uterus only treats the symptoms, not the cause. The pelvic organs that are affected by the depression can be raised and fixed again, but the weakness of the tissue remains. Thus, it cannot be ruled out that renewed reductions may occur. Newer surgical methods that work with the inlay of a net are intended to reduce the risk of a renewed lowering, but cannot completely eliminate it.
Another long-term consequence can be incontinence, which is caused by overcorrection of the urinary bladder. This can be treated in a variety of ways, both with conservative measures and with further operative measures. However, there may be cases in which incontinence persists as a long-term consequence. If the uterus was completely removed during the operation, the obvious consequence of this is that no more children can be conceived and the menstrual period suddenly stops. In addition, the sensation during sexual intercourse can change and an earlier onset of menopause may be possible.
Can the operation also be carried out on an outpatient basis?
An outpatient operation to lower the uterus is not a common procedure, although it cannot be ruled out that there are isolated clinics that perform this operation on an outpatient basis. The standard is a short stay in the clinic of a few days, which makes sense because you can react quickly to incontinence or other complications of the operation. There is also a risk of bleeding after an operation in the pelvic area. Although this is low, it cannot be completely ruled out and can best be monitored in a stationary environment.
How long will you be on sick leave?
The length of the sick leave depends on the individual healing process after the operation. As a rule, however, there are few complications, so that work can be resumed just a few days after discharge.
However, care should be taken to ensure that no heavy objects are lifted in the first few weeks after the operation and that long periods of standing should be avoided. If the job includes such activities, a longer sick leave may be necessary in order not to negatively affect the healing process.