OP of a herniated disc of the cervical spine
introduction
Further extensive information on this topic can be found on our main page Herniated disc of the cervical spine
General information about the herniated disc
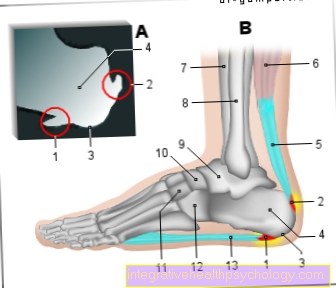
The Cervical spine consists of seven cervical vertebrae. The Band washers each lie between two vertebral bodies of the spine and are responsible for the mobility of the spine. It consists of two parts of an outer zone, the Annulus fibrosus and a gelatinous core, the Nucleus pulposus.
In the context of a herniated disc, the core of the disc shifts (Nucleus) in the direction of the spinal canal or a nerve root and breaks through the outer zone of the intervertebral disc. Of the leaked core can the Spinal cord constrict and thus lead to the typical symptoms of a herniated disc.
The cause is usually the aging of the intervertebral disc with increasing age. In addition, there is an additional one in old age due to bony additions to the vertebral bodies Narrowing of the cervical canal, in which the spinal cord is located.
Most frequently the herniated disc occurs on the cervical spine between the vertebral bodies C5 and C6.

Symptoms of a herniated disc of the cervical spine
Depending on the height of the herniated disc, different areas on the upper arm and hand can be affected. Muscle paralysis and numbness can occur.
At the most frequent level C5 / C6 there is characteristically pain or sensitivity disorders in the area of the upper arm, the thumb-side part of the forearm and the thumb as well as failure of the biceps brachii and the Brachioradialis muscle.
A herniated disc at C6 / 7, in contrast to a herniation at the C5 / C6 level, results in a (partial) failure of the triceps muscle and pain in the index, middle and ring fingers. Any sensory disturbances also occur in these areas.
Read more on the subject at: Symptoms of a herniated disc of the cervical spine
Before the operation
Diagnostics before the operation
There is definitely one before an operation Imaging of the cervical spine required. An operation is only useful if the location of the herniated disc and the clinical symptoms match. A CT (Computed Tomography) or an MRI (Magnetic resonance imaging). While CT can show bony structures of the spine well, MRI is used to show soft tissues, including the intervertebral discs and the spinal cord.
Indications for an OP
Before surgery should be recommended for a herniated disc, it is treated conservatively. The focus is next to one Pain therapy (for example with Ibuprofen) also physiotherapy or physiotherapy with exercise and special Exercises for a herniated disc of the cervical spine. In most cases, a herniated disc can be successfully treated with these measures.
Should be conservative therapy no improvement within 6 weeks bring or lie neurological symptoms, like paralysis (Paresis) up to the onset of paraplegia, sensory disorders, bladder or bowel disorders, an operation should be performed. Another indication for surgery is that Exacerbation of existing symptoms.
The operation of a herniated disc of the cervical spine
Surgical procedure
For the operation of a herniated disc on the cervical spine, two different procedures are usually possible:
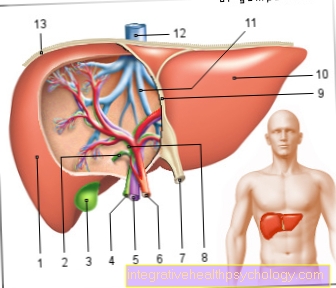
- Anterior Discectomy with Anterior Fusion: This is done using a microsurgical technique that requires access from the front through the neck. Here, the patient is placed on his back on the operating table. Access is through a small incision in the neck area. After opening, the muscles and surrounding structures (vessels, nerves, the windpipe or the thyroid gland) are carefully pushed aside to reveal the spine. The affected intervertebral disc is sought out and completely removed, bony attachments of the vertebrae that narrow the spinal canal can also be removed.
- Dorsal foraminotomy with nerve root relief: This is done via an access from the back. Access from behind via the back is mainly done to the side (laterally) in the case of herniated discs. In the case of additional bony attachments on the vertebral body, this technique is inferior to the approach from the front.The operation is performed in the prone / side position of the patient. After making a small incision in the neck area, the muscles of the neck are carefully pushed to the side to expose the cervical spine. Then parts of the vertebral arch and the affected disc are removed.
Depending on the type of herniated disc, the surgeon selects the appropriate procedure. In complex cases, a mixture of the two surgical procedures may be necessary. The standard procedure is the discectomy with an access from the front via the neck, since with an access from the rear the spinal cord is always in front of the vertebral body. Both procedures are performed under general anesthesia as part of an inpatient stay.
As Replacement for the intervertebral disc becomes either a so-called Titanium cage or one Intervertebral disc prosthesis used. However, the prosthesis is only used in young patients without bony attachments or pronounced degeneration of the vertebral bodies. The advantage of the intervertebral disc prosthesis is permanent mobility in the operated segment, as the prosthesis is based on a real intervertebral disc. It is made up of an inner soft core and a firmer outer structure. For whom this prosthesis is suitable and makes sense must always be decided individually for each patient together with the treating doctor.
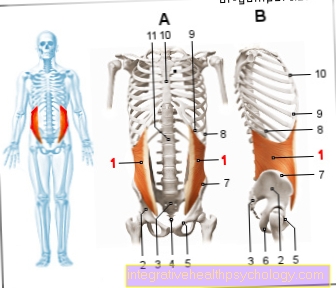
Instead of the cage, a Bone chip from the iliac crest of the patient. Nowadays, however, this technique is only used less frequently because patients with cage fittings can mobilize earlier postoperatively. The disadvantage of the cage, however, is the stiffening of the affected vertebral segment, so that there may be limited mobility in this area.
In addition, under certain circumstances the stabilization of the spine can be achieved via a Screw-rod system or one plate may be necessary to counteract instability in the spine.
Complications and risks of surgery
As with any operation, this procedure also involves risks. First of all, the general risks of an operation must be mentioned: It can be postoperative too Bleeding in the operating theater, Infections or but Wound healing disorders come. In the case of surgery on the cervical spine, in addition to Injury to the spinal cord or nerves come. This manifests itself in sensory disturbances or disturbances of movement up to paralysis. However, overall nerve injury is very rare. Furthermore, surrounding structures such as muscles, windpipe, thyroid or blood vessels can be injured. Temporary hoarseness can occur after the operation, but this usually disappears again. Also can painful swallowing occur the first few days after surgery. Overall, however, complications are rare.
Duration of the operation
The operation is performed as part of an inpatient stay. Usually the patient is admitted to the ward the day before the operation. The operation itself usually takes time an hour up to 90 minutes. Complications are rare but possible. After that it closes inpatient stay of 2 to 7 days on. The length of stay varies depending on the hospital, but also depending on the patient's recovery or the occurrence of complications.
After the operation
How long is the recovery time after the operation?
The length of illness after the operation varies depending on how long the hospital stay is and whether it is followed by rehab. Overall should be with a recovery time of about 3 to 6 weeks be expected.
Rehabilitation (REHA)
After the inpatient hospital stay is one Rehabilitation measure (Rehabilitation) not absolutely necessary, but can follow. This can be done as an inpatient or outpatient from home. If there are no neurological deficits, rehab is not absolutely necessary.
The aims of the rehabilitation measure are among others Pain relief, the muscular stabilization of the operated segment, structure and Strengthening the back muscles including back training and demonstration of special back exercises. Furthermore, the patients should be informed about the illness, coping with everyday life and the prognosis of the illness at a rehab. Professional reintegration and advice can also be topics.
In addition to rehab, a Physiotherapy or physiotherapy treatment to be started. Therapy with Pain medication be useful. Depending on the surgical technique and the hospital, wearing a Ruff to stabilize the spine for a few weeks after surgery.
forecast
With advanced symptoms can through surgery unfortunately no guarantee for the complete resolution of the symptoms can be given, but one can Improvement of the symptoms enter.
















.jpg)


.jpg)