Liver cancer therapy
Note
All information given here is only of a general nature, tumor therapy always belongs in the hands of an experienced oncologist (tumor specialist)!
introduction
Liver cell carcinoma (Liver cancer) represents a serious disease of the cells and tissue of the liver. The cause of this uncontrolled cell proliferation is in most cases due to various previous diseases of the liver.
80% of hepatocellular carcinomas are based on cirrhosis of the liver, the cause of which is excessive alcohol consumption or previous liver inflammation (hepatitis) lies. The metabolic disease hemochromatosis (Iron storage disease) can lead to liver cell carcinoma.
The new disease rate in Germany is 5-6 patients per 100,000 population. The age of onset is between 50 and 60 years. Men are affected more frequently than women. This disease occurs earlier and more frequently in the population of tropical areas in Africa and Asia.

General
The symptoms develop late and range from epigastric discomfort, bloating, nausea and weight loss to stomach bleeding.
A common sign of liver cancer is jaundice, a yellowing of the eyes and skin caused by the liver not doing detoxification.
The classification of liver cell cancer forms is based on the one hand on the distribution in the liver, the histological type, and the TNM classification typical of cancer diseases.
Liver cancer therapy
The type of therapy for liver cancer depends on the one hand on the amount of liver foci found and on the other hand on whether the primary tumor is in the liver or as a secondary tumor (metastasis) migrated from another organ.
In primary hepatocellular carcinoma, the foci of which are already widespread in the liver or have already grown through larger blood vessels, there is no curative therapy, only life-improving (palliative therapy) possible. This usually consists of the administration of a chemotherapeutic agent (5-fluorouracil) together, but this has no life-prolonging effect.
If another tumor has metastasized, no more than 50% of the liver should be involved and no cirrhosis of the liver should be known when 5-fluorouracil is used. Treatment with a drug that inhibits an enzyme called multikinase - sorafenib - may also be considered.
Another possibility of palliative treatment is the local injection of an alcohol solution directly into the metastasis / tumor focus of the liver. Alcohol injection is most successful when the tumor is less than 3 cm in size. In this case, the hoped-for tumor necrosis occurs in 70% of cases (Tumor death).
5 years after alcohol injection treatment, 30-60% of patients are still alive. The disadvantage of this type of treatment is the frequent relapse rate (33% -43%) and the resulting repetitive therapy sessions. Furthermore, there are also icing (Cryotherapy) or heating is used locally directly on the tumor in the liver.
If the tumor is minor, curative therapy can be tried. It includes the surgical removal of the affected liver segment (Partial liver resection). Since humans are able to live with a small part of their liver, this therapy option is a sensible consideration.
It is important that it is at an early stage of diagnosis (T1-T2) and the tumor may only be limited to one lobe of the liver. Surgical removal of liver metastases is only possible if individual, maximum 4 metastases in 4 segments are found, no other organ is affected and the primary tumor is also operable.
During the operation, a transverse or mid-abdominal incision is made.A cut along the costal arch or a laparoscopic procedure is also possible. Nowadays so-called ultrasonic knives are used in this operation, which are intended to make it easier to reach the liver and to reduce blood loss during the operation.
Depending on the location of the liver tumor, a so-called peripheral resection is chosen. Here the tumor is on the edge of the liver, the surgeon does not have to adhere to anatomical conditions. A wedge is cut out and a safety distance of approx. 1 cm is observed, i.e. 1 cm must be cut into healthy tissue that has not been affected by the tumor.
If the tumor is limited to a specific liver segment, the entire segment (Segment resection) removed from the liver. If affected, the entire half of the liver may be removed (Hemihepatectomy). Palliative operations are also possible and are intended to remove bottlenecks caused by the tumor.
What are the therapy options?
There are a number of therapies for treating liver cancer. The therapeutic procedure with the best prognosis is surgical removal of the cancer. This usually requires removing part of the liver. In many cases, however, this is not possible.
In these cases, a liver transplant is an option. However, a long waiting time is to be expected with liver transplantation, so that various methods have been developed to prevent tumor growth until transplantation.
The last treatment option for patients with hepatocellular carcinoma without metastases is liver transplantation. Due to the shortage of organ donors, however, it is not a very common measure because, due to lack of time, a transplantation can usually no longer take place.
A liver transplant can only be carried out if the so-called Milano criteria are met (1 tumor must be less than 5 cm in size or a maximum of 3 tumors, each 3 cm in diameter). If the tumor is already connected to the blood vessel system or if findings occur outside the liver, this excludes a liver transplant.
In addition, the patient must meet certain guidelines: does his liver disease also have an alcohol problem? So he must have been demonstrably abstinent recently in order to allow him to be shortlisted for donor organ applicants. If the patient meets the criteria for a liver transplant and is placed on the waiting list, bridging therapy measures should be considered.
Another therapeutic option is radio frequency ablation. Here, electricity is used to generate heat in the tumor tissue in order to destroy it. This procedure can be used to bridge the gap to liver transplantation or as curative therapy. However, the risk of recurrence, i.e. the risk that cancer will develop in the liver again, is very high at 70%. Does the patient have fluid in the abdomen (Ascites), or if the tumors are in the vicinity of large biliary tracts, this type of therapy should be avoided.
Laser-induced thermotherapy (LITT) can also be used in the treatment of metastases. In this case, a computer tomograph (CT) punctured the tumor focus and then later introduced the laser. Magnetic resonance imaging, i.e. an MRI of the liver, can be used to track the success rate of the treatment with the help of temperature-dependent images.
Liver metastases, the organs of which are to be found in the stomach, pancreas or lungs, are not treated with LITT, since a systemic event must be assumed here.
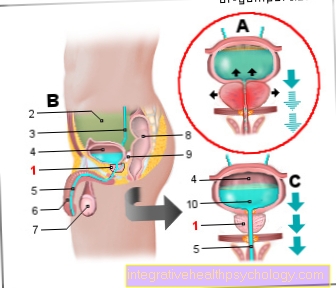
Another option is transarterial chemoembolization. Here, chemotherapeutic agents are applied locally to the cancer via the vessels in order to reduce its growth and to cut off its blood supply. One makes use of the fact that the hepatocellular carcinoma is mainly supplied arterially.
During the treatment, the artery of the leg (Femoral artery) of the patient and a catheter through the main artery (aorta) into the vascular branch supplying the liver (Celiac trunk) placed. The vessels are better represented by the administration of contrast medium. Another catheter is now pushed through the first directly to the liver tumor. The closer the catheter is to the tumor, the lower the risk that healthy areas will be embolized with it.
If the position is correct, a number of drugs are now delivered directly to the tumor via the catheter. Lipidol Emulsion - vessels that supply the liver are closed and increase the duration of the chemotherapy drug's effect.
Plastic particles are injected into the tumor area, slowing the blood flow rate and causing the vessels that supply the tumor to become blocked. As chemotherapeutic agents, doxorubicin, carboplatin and mitomycin, etc. are used. This embolization is then repeated.
This treatment must not be carried out in patients with cardiac or hepatic insufficiency, a contrast agent allergy or blood clotting disorders.
In advanced stages, in which the cancer has already infiltrated surrounding vessels or spread to other organs, only palliative therapy for liver cancer with the drug sorafenib is carried out. Your goal is no longer to heal the person affected, but to improve the quality of life.
The type of therapy carried out for liver cell carcinoma (Liver cancer) is distributed among the patients as follows: 73% of the patients do not receive any therapy because the time of diagnosis is too late and the disease is too advanced. 12% received surgical therapy with removal of liver parts or metastasis removal. 6% receive chemotherapy. 9% of the patients receive another, not further classified therapy.
Operative treatment of liver cancer
Surgical removal of liver cancer is the therapy with the best chance of recovery. The liver can be divided into four lobes. One, two or even three flaps are usually removed during an operation. However, there are many cases when this therapy is not possible.
Factors that speak against an operation are, on the one hand, infiltration of the entire liver or poor liver function of the tissue not affected by the cancer, e.g. due to cirrhosis of the liver. Liver cirrhosis is a connective tissue-like remodeling of the liver, which is associated with a deterioration in its function. In these cases, liver transplantation is an option.
In those cases in which it is not certain whether the remaining tissue is sufficiently functional, a special operation can be performed. In this surgical procedure, the first step is to clamp off the blood vessels that supply the part of the liver that is to be removed. Then a check is made to see whether the remaining liver tissue is functioning properly. In the second step, the liver part can then be removed or reconnected to the blood supply. In addition, patients can no longer be operated on if the cancer has metastasized or infiltrated into blood vessels.
Liver transplant
Liver transplantation is the only option for many when liver function is poor. The problem with liver transplants lies in the long waiting times because there are far too few organs. At the moment the waiting time is between 6-18 months.
Since the cancer cannot be left untreated during this time, various methods are used to prevent the cancer from growing during this period. Two common methods for so-called bridging are the radioablation method and chemoebolization, which are explained in the chapter “Which therapy methods are there?”.
However, to be eligible for a liver transplant, a number of conditions must be met. The tumor must not infiltrate any vessels and there must be no metastases. The tumor is between 2 and 5 cm in size or there are 1 to 3 tumors between 1 and 3 cm. If all criteria are met, patients are placed on the waiting list.
The urgency is assigned according to the severity of the disease. For this one orientates oneself on the liver value bilirubin, the kidney value creatinine and on the blood coagulation. A score is calculated from these values. Patients with a tumor can receive additional points. In principle, there is also the possibility of a living donation. The same conditions must be met for this.
For more detailed information on this topic, see: Liver transplant
Chemotherapy for liver cancer
In the western world, chemotherapy hardly plays a role in the treatment of liver cancer, since liver cancer is often associated with liver cirrhosis. In other countries, chemotherapy is used to treat liver cancer. Local chemotherapy procedures are used in the western world. As a rule, however, these have no intention of healing, but are used for so-called bridging - i.e. to combat tumor growth while waiting for a new liver.
The procedure is called transarterial chemoembolization (TACE). A catheter is pushed through the groin into the hepatic arteries. Chemotherapeutic agents can then be administered locally via this catheter. In addition, small plastic particles are placed in the vessel that supplies the tumor. This clogs this vessel and the cancer cells are no longer adequately supplied with nutrients and oxygen and die.
Chemo-embolization is also often combined with drug therapy in patients who are being treated palliatively, since studies have shown an increase in lifespan. However, TACE should only be used in patients who still have good liver function.
Radiation treatment of liver tumors
There are two different ways of irradiation. On the one hand, there is classic radiation therapy, in which external radiation is applied to the liver cancer. This procedure is used when the tumor cannot be removed by surgery.
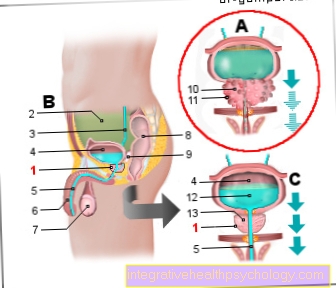
Another radiation method is selective internal radiotherapy (SIRT), also transarterial radioembolization (TARE) called. With SIRT, the cancer cells are irradiated from within. Here, small spheres that emit rays are positioned in the vessels of the tumor. As a result, the cancer cells are exposed to a higher dose of radiation and the vessels that supply the tumor are closed.
What are the side effects of therapy?
The side effects vary depending on the therapy. Liver transplantation is associated with a certain risk of rejection. Rejection mostly occurs in the first year after the transplant. There are different reactions to rejection. In some cases the graft needs to be removed as a result.
In all cases, a lifelong suppression of the immune system with medication is necessary after a transplant. This makes you more susceptible to infections. In addition, the various medications can lead to other side effects that vary from person to person.
With transarterial radioembolization, there is a risk that the globules emitted by the rays slip in their position and, under certain circumstances, get into the vicinity of other abdominal organs. Here they can cause considerable side effects, as they lead to the death of cells.
The drug sorafenib, which is used when the tumor can no longer be surgically removed or treated with other methods, can cause diarrhea, rashes, bleeding and other symptoms.
What is the prognosis?
In order to be able to make a statement about the prognosis after the diagnosis of liver cancer, the tumor stage, liver function (Impaired liver function suggests an advanced stage of the disease with a worsening prognosis), the general state of health and the potential influence of therapeutic measures must be taken into account.
Without appropriate therapy, the prognosis is poor. Since the disease leads to symptoms relatively late and liver cell carcinoma is only diagnosed at an advanced stage, there is often only the option of palliative therapy. Here the median survival rates are only 6-12 months.
If curative treatment is attempted, the 5-year survival rates for liver transplantation are 40-70%, after partial liver removal 20-50% and after local tumor removal 20-50%. After liver surgery, mortality during the operation and up to a maximum of 3 months afterwards is 10%.
If liver cell carcinoma is treated as having been treated, there is of course always the risk of relapse (Relapse). If the tumor has already found connection to the blood vessel system and both lobes of the liver were affected by the tumor, the probability of a relapse is quite high. The size of the tumor must also be taken into account when calculating the probability of a relapse.
This is how liver cancer is diagnosed
In addition to the anamnesis, in which he asks about the beginning and course of the complaint, the doctor should also conduct a physical examination with palpation and listening of the abdomen. Sometimes he can diagnose an enlarged liver, the thickened tumor or flow noises of the blood vessels.
The ultrasound examination can often make a malignant tumor visible and differentiate it from a metastasis of another primary tumor. With a blood test and tumor marker determination of alpha-fetoprotein and CEA (Carcinoembryonic antigen) the course of liver cell carcinoma can be observed. A biopsy should not be performed for diagnosis, as there is a risk of the tumor spreading.
Is that curable?
In principle, liver cancer can be cured. As with other cancers, the chances of recovery depend on the stage of the cancer. Early stages of cancer can usually be treated better and therefore have a significantly better prognosis. In liver cancer, the functioning of the liver also plays an important role and can limit treatment options.
Many patients with liver cancer also suffer from cirrhosis of the liver. In cirrhosis of the liver, connective tissue is remodeled so that the function of the liver is impaired. If the function of the liver is too severely restricted, it is not possible to remove the liver tissue affected by the cancer as part of an operation, since the liver tissue of the remaining liver tissue would no longer be sufficient. The human would perish.
In such cases, the chances of recovery decrease because the other therapeutic methods have a worse prognosis than surgery. A treatment option with a good prognosis in this case would be a liver transplant. But due to the small number of organs available for transplant, there are long waiting times.
What novel treatments are coming?
Research into the development of drug therapies for the treatment of liver cancer is currently ongoing. With sorafenib, which was approved about ten years ago, a promising first step has been taken. Sorafenib inhibits growth signals in the cells and thus inhibits tumor growth. However, sorafenib cannot cure cancer, but it can significantly extend its lifespan.
Research is being carried out on other similar drugs, and some are already approved for treatment. Immunotherapy with PD1 / PDL1 inhibitors is another source of hope. These drugs are intended to help the body recognize and kill tumor cells. These drugs can also extend life. How effective they actually are remains to be seen in the next few years.
Liver cancer prophylaxis
An important preventive measure is to prevent diseases that result in hepatocellular carcinoma (Liver cancer) - e.g. cirrhosis of the liver, hepatitis. If there is an alcohol problem, abstinence must be achieved immediately, especially if liver cirrhosis has already been proven.
To avoid one of the numerous inflammations of the liver, vaccination (Hepatitis A, hepatitis B) be considered.
Since there is no vaccination against hepatitis C, precautions should be taken with the sources of transmission (Protected sexual intercourse, disposable syringes for heroin addiction) get noticed.
Patients with known liver cirrhosis or hepatitis infection should have a check-up every six months - ultrasound and tumor marker determination - go to the doctor.
Recommendations from the editorial team
Further general information can be found at:
- Liver cancer
- Liver cancer symptoms
- Palliative therapy for liver cancer
- End-stage liver cancer