Risks of a dental implant
introduction
Basically, there are hardly any risks when using dental implants - nevertheless, many patients are very concerned about possible risks and therefore find it difficult to decide whether to have a dental implantation.
The insertion of dental implants is a surgical procedure that is usually, but not always, performed under local anesthesia. If the dental implants are to be implanted under general anesthesia, there are general risks of general anesthesia. During and for a short time after the anesthesia, the cardiovascular system and breathing can be impaired. In addition, there is always the risk of secondary bleeding or wound infections in the operating area.
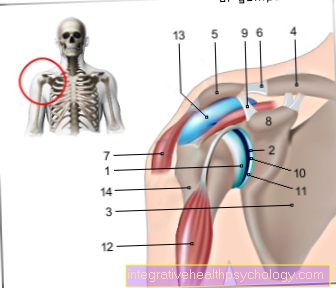
In the special case of the insertion of dental implants, there is a risk of nerve damage; the major submaxillary nerve is particularly affected here (Inferior alveolar nerve).
In rare cases, wound healing disorders can occur.
Find out more on our main page: Wound healing disorder on the tooth

Within the first few days after the operation, the patient usually feels slight to moderate pain in the treated jaw section, and in most cases there is swelling and bruising.
In addition, chewing with the dental implant places significant additional stress on the temporomandibular joint. This is because a "normal" tooth does not grow firmly into the jawbone, but rather on small fibers (Sharpey fibers) is suspended. These Sharpey fibers ensure that the tooth remains under pressure (for example when chewing) cushioned and the jawbone is less stressed.
This reduction in load is also noticeable in the temporomandibular joint.
In the upper jaw, there is also the risk that the maxillary sinus is opened during the implantation of the dental implants, which then has to be covered with plastic.
Probably the greatest risk is the loss of the dental implant. It may be necessary to remove the dental implant again, which is especially the case if the dental implant does not properly heal or if inflammation develops.
For more information, see: Remove the dental implant
Inflammation after implant placement
In the event of inflammation after an implant has been placed, several causes can be considered. Bacteria are mostly bacteria whose metabolism only takes place in the absence of oxygen (Anaerobes). Micro-contamination on the implant is extremely rare, as the industrially manufactured implants are subject to strict quality management during their manufacturing process.
Unclean, non-sterile work by the surgeon and his team can also be a cause.
Furthermore, a hypersensitivity or intolerance reaction to the implant material (very rarely!) Can lead to typical inflammation symptoms.
Also z. B. an open healing method carries risks. “Open” means that the mucous membrane has not been sutured over the implant, which means that the upper part of the implant protrudes into the oral cavity and there is also in contact with all of the germs in the oral cavity. The implant thus provides direct access to the jawbone.
Incorrect therapy can also cause an implant to trigger inflammation. This is the case, for example, when a patient takes bisphosphonates to treat osteoporosis and the bone structure is unsuitable for implants. In this case no implant should be placed. Both possibilities can be avoided by taking a careful and extensive anamnesis (questioning the patient), whereas the healing method is left to the choice of the surgeon.
But once an inflammation has developed around an implant, one speaks of one Peri-implantitis. Here, after prior germ determination and ozone vaporization with subsequent antibiotic treatment, an attempt can be made to stop the process.
Read more on the topic: Inflammation on the dental implant, peri-implantitis
The implant does not grow in
Should it ever happen that a dental implant does not grow in properly, there can be a variety of reasons.
One of the many causes is, for example, osteoporosis. The bone structure is then loosened and offers the implant neither the necessary support nor the necessary bone-building cells that are required for the bone to grow into the implant thread.
Immediate loading of the implant insert is also discussed. While some implantologists advertise that the patient leaves the practice with a fixed set of teeth, others prefer to rely on the conventional method of 3-6 months of healing and only then stress.
A rejection reaction can also occur in patients who were treated with bisphosphonates during their cancer illness. Bone necrosis (death of the bone) around the implant can be the serious reaction here.
Read about it too: Shelf life of dental implants
What is peri-implantitis?
At a Peri-implantitis it is an inflamed area around the implant, usually with greater bone involvement, as it is rarely discovered in the beginning.
The aim after implantation is for the implant to heal in the bony. This means that the bone grows directly up to the microstructure of the implant surface and adheres to it. If this healing is disturbed, for example by peri-implantitis, there is often, if at all, only connective tissue healing, which is less stable.
The pathogens are mostly Anaerobes, that means they have a metabolism that does not involve oxygen. Also so-called gram negative bacteria or the well-known skin germ Staphylococcus aureus can be the culprits.
This inflammatory process is exacerbated by smoking, diabetes, osteoporosis, crunching or even genetic predispositions. However, errors when placing the implant due to the development of heat in the bone and later a malfunction of the corresponding crowns can have an unfavorable effect on perimplantitis. For this purpose, e.g. that remains of the cement that was used to fix the crowns was not completely removed.
In order to be able to treat successfully after removal of the remains, a germ test to determine the pathogen, an ozone therapy (ozone is trivalent oxygen, there is a reaction on the implant that kills the pathogen) and an antibiotic tailored to the pathogen found helps.
In rare cases the implant must be removed (Replantation) and a reconstruction with artificial bone and, after a corresponding waiting period of months, a new implantation.
Learn more about: When does a dental implant need to be removed ?, peri-implantitis
How does smoking increase the risks?
Every smoker, just like a diabetic, has a greatly increased risk that implants will not heal because the Micro blood circulation disturbed is.
That means the number and quality of the smallest blood vessels that Capillaries, are reduced: the superficial tissues are not adequately supplied. However, this is absolutely necessary, among other things so that the cells of the immune defense are able to migrate to the site of the inflammation and fulfill their task in the event of invading germs.
In addition, the ingredients of the smoke endanger the entire oral mucosa.
So smokers are at greater risk of wound healing. This applies to the mucous membrane as well as to the bones. Also one Peri-implantitis (Inflammation around the implant) is found much more frequently in smokers, and the rate of implant losses in smokers is significantly higher than in non-smokers.
You might also be interested in: How to quit smoking
Allergy to the dental implant
An allergy to the dental implant is rare because the materials from which implants are made are highly biocompatible, i.e. tissue-friendly.
They consist e.g. made of ceramic (such as zirconium oxide) and are used in the visible anterior region for aesthetic reasons. Alternatively, they are made of titanium oxide for use in the posterior region. Titanium implants can have micropollutants of either nickel or tin, whatever in sensitive patients can lead to intolerance.
also read: Symptoms of an allergy
Despite all this, titanium has the highest tolerance level and, like zirconium oxide, heals perfectly into human bones. If there is a suspicion that a patient may have an allergy to the substances to be used, this can be found out in advance by an allergist via a test.
Injury to other teeth during implantation
During the implantation, a so-called drilling template is usually not used by eye. Therefore, if all the manufacturing rules for the template are observed, other teeth cannot be injured.
In the meantime, special imaging processes are even used to guarantee exact precision. These can be of computed tomographic (CT) or digital volume tomographic (DVT) origin, both of which are radiological procedures.
The has had a special development in the last year ultrasound-assisted pilot system lived through by Prof. Derycke. With this system, implants are implanted in real time via a screen and deviations from the projections are indicated with a warning signal.
Bleeding after implant placement
After the implant has been inserted, bleeding usually only comes from the mucous membrane covering the implant, since there are more blood vessels than in the bone. The oral mucosa regenerates completely within a few days, so the bleeding should not be a cause for concern. However, there are exceptions with heavy bleeding that you should contact the dentist.
Treatment of the patient with anticoagulant agents, such as e.g. Marcumar®. This also includes, for example, patients who suffer from prolonged headaches Aspirin® are not allowed to take this until 14 days before the implantation, otherwise the platelet aggregation (sticking together of the blood platelets) would be disturbed.
Fistula after implant placement
If the inflammation is localized inside the bone, the resulting pus looks for a drainage channel: a fistula arises.
A fistula is a tubular, pathologically created duct (this means that it developed during disease and does not belong to the normal healthy anatomy). It leads from a cavity, e.g. B. an abscess or a natural hollow organ to the body surface.
Find out more about: Fistula on the tooth
A risk of fistula formation that should not be underestimated is too little distance to the neighboring teeth or neighboring implants. This should not be less than 2mm, as otherwise no vascularization (new vessel formation) can occur.
The bone portion can die off due to the insufficient supply of blood, which then leads to Bone necrosis (Death of the bone) with the accompanying inflammatory reactions such as pus formation.











.jpg)