S1 syndrome
definition
The S1 syndrome describes a complex of symptoms that arise from irritation or damage to the S1 nerve root.
The most common cause of S1 syndrome is a herniated disc in the area of the fifth lumbar vertebrae and the first sacral vertebra.
The S1 syndrome is associated with pain, impaired sensitivity and paralysis in the nerve root supply area, which extends from the buttocks to the little toe.
Generally these complaints are known as the typical "sciatic pain".
Read more about the topic here: Pain in the tailbone- these are the causes

root cause
There are various causes that can trigger S1 syndrome.
In principle, any process in the spine that can lead to a reduction in space and constriction of the nerve roots is a possible cause of an S1 syndrome.
Basically, an S1 syndrome occurs when the S1 nerve root in the spine is compressed.
In most cases this is a herniated disc between the 5th lumbar vertebra (L5) and the beginning of the sacrum (S1).
Both a simple protrusion of the intervertebral disc and the emergence of the gelatinous nucleus from the fibrous ring can exert pressure on the nerve root and cause discomfort.
Other possible causes of an S1 syndrome are benign and malignant tumors and cysts in the area of the spine or fluid accumulation, so-called edema, as a result of inflammation.
Another possibility is a tightness in the area of the neuroforamina.
This is a bony opening in the vertebral body through which the nerve fibers run.
A narrowing of these structures can be congenital or degenerative.
Often, narrowed neuroforamina are a natural symptom of wear and tear.
You can find out more about the topic here: Herniated disc at level L5 / S1
Herniated disc L5 / S1
The intervertebral discs are located between the vertebral bodies and serve to buffer the load and the mobility of the spine. In the case of a herniated disc, parts of the intervertebral disc are displaced, usually backwards and to the side. As a result, one or more nerve roots become trapped and emerge from the spinal cord there. In the case of a herniated disc at the L5 / S1 level, the nerve root of S1 is usually affected. Depending on the amount of tissue displaced and the direction of displacement, the L5 nerve root (L5 syndrome) or both nerve roots can also be affected. This is then expressed in a specific pattern of the resulting symptoms.
For further information please visit our page: Herniated disc at level L5 / S1
Appointment with a specialist for a herniated disc?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
A herniated disc is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
Therefore, treating a herniated disc requires a lot of experience.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
Symptoms
An S1 syndrome causes characteristic complaints such as pain, impaired sensation and paralysis in the area supplied by the S1 nerve root.
A major symptom is pain.
These can run from the lower back and buttocks over the rear thighs and lower legs, affecting the lateral edge of the foot and the little toe.
The pain is often described as suddenly shooting in and occurs in many sufferers depending on stress.
In addition, abnormal sensations such as tingling, pins and needles or numbness can often be noticed in this area.
In addition, the calf muscles (triceps surae muscle), the hamstring muscle (biceps femoris muscle) and the lower legs can be paralyzed.
This manifests itself in a weakness in the lowering of the foot and an inability to stand or walk on tiptoe.
Typically, the Achilles tendon reflex is extinguished because it is caused by a muscle twitch of the triceps surae muscle.
Pain in the leg
S1 syndrome is often associated with pain that extends from the lower back and buttocks into the leg.
The pain is localized on the outside and back of the thigh and lower leg.
You can pull from the side of the foot to the little toe.
The pain is usually described as suddenly shooting in and occurs during physical exertion.
If there is permanent compression of the nerve root, for example in the context of a narrowed neuroforamen or a tumor, the pain is usually permanent.
Heel pain
The nerve root S1 supplies areas from the buttocks to the little toe and runs from the back of the lower leg over the heel to the lateral edge of the foot.
The heel is therefore supplied by the S1 nerve root and can become symptomatic in the S1 syndrome.
Heel pain is a possible symptom of this condition.
diagnosis
In order to diagnose S1 syndrome, the precise questioning by the doctor and the physical examination are decisive. The main focus of the questions is on the precise classification of the pain as well as inquiries about other symptoms, previous stresses, accidents and known diseases.
During the examination, the doctor pays particular attention to abnormalities in the gait and static image and especially to the toe walk. He also checks the sensitivity of the skin for diminution or, if necessary, paresthesia and tests the Achilles tendon reflex. Additional imaging can be used to detect and accurately assess a herniated disc.
Localization left / right
In principle, the body and especially the extremities have a very symmetrical construction plan.
This also applies to the spinal nerve roots, which emerge from the spinal cord on the same side and pull to the right and left to their respective supply area.
The side comparison can, however, represent an important diagnostic criterion and provide further information about the exact localization and severity of the cause, especially a herniated disc.
If the symptoms are one-sided, only the nerve root on the same side is affected by the narrowing or irritation.
The comparison with the symptom-free side can be used during the examination to determine the extent of the complaints and to narrow them down more precisely.
For example, are touches perceived equally on both sides or are the sensations on the affected side weakened?
If the symptoms occur in the same way in both extremities, the S1 syndrome is probably based on a very pronounced, large herniated disc or larger space-consuming processes such as tumors or edema.
Lasegue test
The Lasègue sign is used to examine the L4, L5, S1, S2 and S3 nerve roots as well as the sciatic nerve.
The sciatic nerve, also known as the sciatic nerve, arises from the nerve roots L4 to S3.
To perform the test, the patient lies on their back and the doctor bends the patient's extended leg at the hip.
This flexion causes the sciatic nerve to stretch.
A positive Lasègue sign is a shooting pain that occurs before and / or during the examination at around 70 to 80 ° flexion.
A positive Lasègue sign can indicate
- a herniated disc of the lumbar spine
- a nerve root inflammation
and or - a meningitis
be.
Another test: Bragard test
treatment
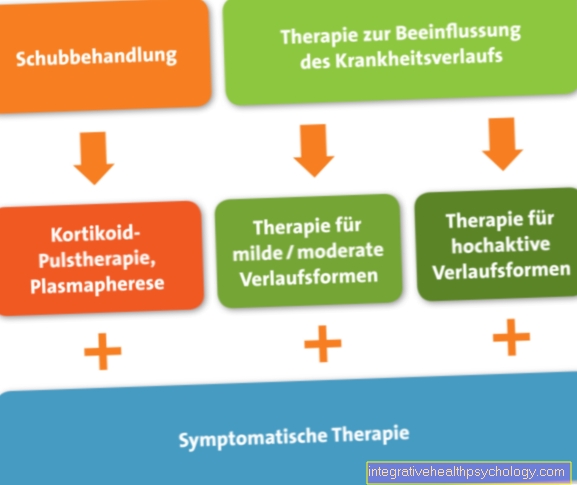
For the therapy of the S1 syndrome, a multimodal treatment principle, i.e. a combination of several therapy options, is usually sought.
The S1 syndrome is often based on a herniated disc.
This is usually treated conservatively.
The focus of this therapy is, of course, first and foremost on pain relief.
In addition to the administration of painkillers, procedures such as acupuncture, massages, heat applications or minimally invasive interventions such as periradicular therapy (see below) are used for this purpose.
However, just as important as acute pain relief is strengthening the back muscles to stabilize and relieve the spine and to prevent recurring complaints.
Physiotherapy as well as movement and behavior training are particularly suitable for this.
It is important to note that rest or bed rest tend to worsen the symptoms rather than improve them.
In more severe cases, operations may be necessary in which the affected vertebral segment is exposed and the restricting structures, such as intervertebral disc tissue or bony parts, are removed or the entire intervertebral disc is replaced.
However, a herniated disc rarely requires surgery.
An operation is urgently indicated if paralysis occurs or a narrowing of the neuroforamina is the cause of the symptoms.
It is therefore advisable to start physiotherapy and exercise therapy when back problems begin to prevent the symptoms from worsening and becoming chronic.
These exercises can help
Exercising the back muscles can help alleviate the symptoms, especially if a herniated disc is the cause of S1 syndrome.
It is advisable to specifically strengthen the back muscles in order to prevent poor posture caused by pain and chronic symptoms.
In addition to exercises, pain therapy should be carried out.
Possible exercises in S1 syndrome are arm support with arm and leg raises, forearm support (plank exercise) and rowing.
Ab exercises like sit ups can help stabilize your core.
It is important to start exercising gently and gradually increase at a slow pace.
If you train too quickly with too much commitment, you can damage your back.
One should be especially careful when training with weights.
Furthermore, yoga exercises, such as the cat, dog and cobra, are very good for stretching the back.
More exercises
We recommend exercises that the patient can do alone at home after detailed instructions from the doctor or therapist.
Ultimately, it is good to mobilize the spine in all directions of movement and to hold each position for at least 30 seconds.
However, you should not go beyond the pain point, but only move to the position where you do not feel any pain.
The movements include bringing the shoulders and knees closer together (a flexion), bending the back into a "hollow back" (an extension), tilting sideways and rotating while flexing at the same time.
The latter can be achieved by turning the pelvis to the side while lying on your back with your knees drawn up.
Periradicular Therapy (PRT)
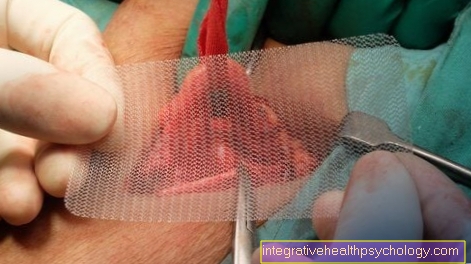
Periradicular therapy is the application of a drug directly to the affected nerve root. For this purpose, an imaging (MRT / CT) is first carried out in order to be able to assess the affected vertebral body and the nerve root precisely and to plan the stab guide. Then, with the help of a targeting laser, the thin injection needle is brought as close as possible to the nerve root and the drug is injected.
Usually a combination of a locally active anesthetic and a steroid, e.g. Cortisone. These have a pain-relieving effect on the one hand, and decongestant and anti-inflammatory effects on the other, thus counteracting the irritation of the nerve roots.
Read here on our site: periradicular therapy
Duration
The duration of the complaints can be very different. An acute severe episode usually lasts a few days. Depending on the cause and the necessary treatment, it can take 1-2 months until the symptoms are completely resolved.
Sufficient exercise and stress that is gentle on the back should also be maintained beyond that in order to counteract recurring complaints.
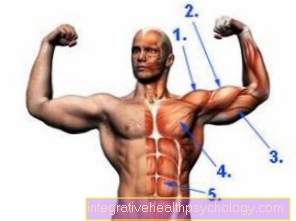
Identification muscles
The nerve roots of the spinal cord form the starting point for all nerves that control and transmit both the movement of the muscles and the sensations on the skin. Certain nerves can therefore be assigned to each nerve root. For each nerve, in turn, its respective target area, in the sense of individual muscles and skin areas, is known very specifically.
These muscles, which, if they fail, indicate damage to a particular nerve root, are called identification muscles. For the nerve root of S1, these are on the one hand the fibula muscles (Mm. Peronei) on the lower leg and on the other hand the rear calf muscles (M. triceps surae). Both muscle groups are used to lower the foot and to tip the toe. These movements are weakened in S1 syndrome or even fail completely.