Spinal anesthesia
Definition of spinal anesthesia
Spinal anesthesia (SPA) is one of the regional anesthesia and is used to eliminate pain perception in certain areas of the body. Spinal anesthesia is mainly used when surgery is to be carried out in this region of the body.
Read more on the topic: Conduction anesthesia

In spinal anesthesia, the anesthetic (the so-called local anesthetic) is injected into the immediate vicinity of the spine using a needle. Anatomically, the exact location is called the spinal space. This space extends the length of the entire spine and also contains the nerve water (Liquor). The area in which the sensation of pain is switched off depends on the anatomical puncture point on the back: To eliminate the sensation of pain in the lower abdomen, an injection at the level of the (middle) thoracic spine and for numbing the legs an injection in the area of the Lumbar spine necessary.
Areas of application
Spinal anesthesia is preferred in orthopedics and gynecology. But urological interventions (urology) can also be carried out using SPA.
Frequently performed operations using spinal anesthesia are mainly:
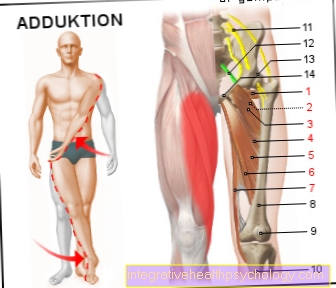
- Operations on the lower extremities
- Operations in the hip area
- Operations in the groin region
- Operations in the lower abdomen
- Caesarean section and natural childbirth
- Operations on the urethra and bladder
Spinal anesthesia at birth
Spinal anesthesia is playing an increasingly important role in childbirth and is increasingly replacing the PDA. Spinal anesthesia is used to relieve pain during childbirth or before a caesarean section. Their advantage over general anesthesia is that the patients are awake even during the caesarean section. This is often requested by the expectant mothers, as they are reluctant to oversleep the birth process and want to hold their child in their arms immediately after the birth.
The application of spinal anesthesia is considered less painful compared to the PDA because a thin needle is inserted. If the spinal anesthesia takes effect, the patients feel neither their lower abdomen nor their legs. In addition, the muscle tone is lowered, so that the legs cannot be moved at will. Some patients find this very unusual and uncomfortable at first. However, the effect diminishes a few hours after the anesthesia and the sensitivity gradually returns. In summary, spinal anesthesia is currently the most useful non-invasive anesthetic for childbirth, as it is also associated with relatively few risks.
Spinal anesthesia during a caesarean section
Since spinal anesthesia is a widely used anesthetic method in operations on the lower abdomen or the groin region is also the operation Caesarean section in Germany a common indication for the The patient is free of pain by means of spinal anesthesia to make sure. Together with the Epidural anesthesia (PDA) it is the most commonly used anesthetic method for caesarean sections planned caesarean section as well as the so-called hasty caesarean sectionwhere the child within half an hour should be born, often performed under spinal anesthesia. Only the Emergency caesarean section with a possible threat to the life of the child or mother is due to the usually faster readiness for operation Indication for general anesthesia represent.
The Spinal anesthesia during caesarean section compared to other anesthetic procedures some advantages. Due to the technique of this procedure, the effects of freedom from pain and muscle relaxation occur Relaxation of muscles, faster than with PDA or general anesthesia. Also, they are more pronounced what fewer complications means. In addition, the Depth of spinal anesthesia very good too beyond the end of the operation control and one needs less local anesthetic than with a PDA.
In addition, other advantages come into play when used specifically during a caesarean section. For one thing, the mother gets it birth of your own child. This may sound secondary, but for most women, childbirth is one of them most important and impressive moments of their lives The 9 month long wait comes to a conclusion and for them Mother-child bond is the first time the mother holds her child in her arms Key moment. Besides, the child gets no burdensome doses on Anesthetic drugs administered. Not to be underestimated is the fact that at regional anesthetic procedures As with spinal anesthesia, the likelihood of complications in the child or mother is lower than with general anesthesia. This is due to the small amounts of systemic drugs and last but not least because the Patient awake is breathes independently and the the body's own protective reflexes are present are. Overall, spinal anesthesia is a popular method of anesthesia used in caesarean sections. As a rule, the anesthesia takes place problem-free and offers good freedom from pain with fewer side effects and complications.
How is spinal anesthesia performed?
Spinal anesthesia is usually applied shortly before the operation. For the puncture, the patient can take a lying or a sitting position. The patient is asked to provide a so-called "Cat hump“To do, so to bend your back as much as possible; This is intended to increase the distance between the individual vertebral bodies.
To make the puncture site sterile, a disinfectant is sprayed on the back. Palpation of the vertebral bodies enables the doctor to find the correct puncture site on the back. Before the puncture needle is inserted, the relevant skin area is locally anesthetized with a much thinner needle. Thus, the application of the spinal anesthesia is usually not perceived as painful.
The puncture needle is advanced a few centimeters below the skin level into the spinal space. This is where the local anesthetic, i.e. the drug that makes it pain-free, is injected.
In contrast to the introduction of a catheter that remains for a longer period of time, this technique is called "Single shot". The introduction of such a thin plastic catheter, as is the case with the installation of a periduarial catheter, is used to continuously supply the local anesthetic during longer surgical procedures. Another advantage compared to the single shot is that the continuous administration of the medication ensures freedom from pain even in the days after the operation.
Overall, the installation of a spinal anesthesia usually takes no longer than ten minutes.
The time from the injection of the local anesthetic to the onset of action only takes a few minutes. In order to check whether the spinal anesthesia is working correctly, the patient is asked to assess a cold stimulus. This is usually set by spraying disinfectant on the legs. Since temperature sensation and pain sensation are switched off equally by the local anesthesia, failure to sense the cold stimulus automatically means that this region is also insensitive to pain.
When combining spinal anesthesia and general anesthesia, the SPA is performed first because the patient can give the doctor information about the temperature sensation in the event of a cold stimulus.
Duration of spinal anesthesia
If performed routinely, the installation of a spinal anesthetic only takes a few minutes. The effect of the anesthesia sets in immediately after the injection of the local anesthetic and possibly an opioid and is initially noticeable through a sensation of warmth in the legs and buttocks.
The duration of the spinal anesthesia depends primarily on the choice of medication which is introduced into the CSF space, in which the spinal cord and spinal nerves are located. These in turn depend on the duration of the procedure, the scope in which the spinal anesthesia is carried out and can be varied. The anesthetist can numb the relevant parts of the body for 1.5 to over 3 hours.
sobriety
sobriety of the patient is one important requirement for performing spinal anesthesia. Did the patient 6 hours before the procedure In any case, the doctor should refrain from spinal anesthesia if he has consumed anything.
The reason for this is that there can always be complications during spinal anesthesia and the patient must be anesthetized. Are under anesthesia some body functions shut down, so too peristalsis in the digestive tract. In addition, the sphincter muscle between the stomach and esophagus is relaxed, so that stomach contents can get back into the esophagus while lying down. The stomach acid can cause inflammation there.
The gastric juice can also flow through the esophagus into the trachea. Since the patient cannot cough during anesthesia, this body's own protective reflex is missing so that the corrosive stomach acid and the food particles can easily reach the lungs. Here, too, the low pH value of the acid causes inflammation. Such post-narcotic pneumonia occurs in only one in 10,000 cases of fasting patients. In patients who have eaten or smoked before the anesthetic, the probability increases many times over.
Do you need a urinary catheter?
Whether a urinary catheter has to be inserted as part of the spinal anesthesia mainly depends on the planned procedure and the habits of the doctors. For example, a urinary catheter is very common for caesarean sections, whereas a catheter can often be dispensed with in orthopedic or trauma surgery operations on the lower extremity. In any case, the urinary catheter will only be inserted after the spinal anesthesia has started to work, so that hardly anything of the system itself should be noticeable.
A special case is a complication of spinal anesthesia - in some cases, urinary retention can occur as a side effect of the anesthesia. Although this is usually reversible within a few hours to a few days, the temporary installation of an indwelling catheter is necessary in order to enable the urinary bladder to be emptied.
Read more on the topic: How is urinary retention treated
dosage
There is no uniform dosage for spinal anesthesia. That's because everyone reacts differently to the medication. This can be due to different physical stature or individual reaction patterns.
However, anesthetists are great endeavors to keep the dosage as low as possible to counteract dangerous side effects. The most commonly used local anesthetics are:
- Bupivacaine (4-20 mg)
- Lidocaine (50-75 mg)
- Ropivacaine (10-15 mg)
Opioids are still given today in addition to local anesthetics. The reason for this is that you can still achieve longer-lasting painlessness with lower doses of local anesthetics. Typical opioids for spinal anesthesia are:
- Fentanyl (20-25 µg)
- Sufentanil (2.5-10 µg)
Are there alternatives to spinal anesthesia?
Spinal anesthesia is closely related to epidural anesthesia in terms of its implementation and effect. All interventions in which pain relief is achieved through spinal anesthesia can also be performed using epidural anesthesia.
With pain therapy in the days after the operation, however, there is a higher risk of loss of brain water with SPA. The risk of infection spreading through the spinal cord is also higher. Therefore, an epidural anesthesia should be used for continuous pain therapy.
All operations and examinations for which spinal anesthesia can be used can also be carried out under general anesthesia, provided there are no special contraindications. See also: Anesthesia
Spinal anesthesia vs. PDA
In order to be able to compare both forms of anesthesia, one must consider the procedure and the desired effect. Both procedures have in common that, unlike under general anesthesia, the patient is still awake. This has the advantage that on the one hand the dangerous risks of general anesthesia can be avoided and on the other hand that the patient can cooperate more easily.
Spinal anesthesia is indicated for minor operations on the lower half of the body. One makes use of the fact that the patient no longer feels any pain locally after such an anesthesia and also cannot arbitrarily contract his muscles. This makes the operation much easier and reduces the risk of injury to the patient.
The epidural anesthesia, on the other hand, is a common means in pain therapy. Depending on the dosage of the anesthetic, the level of anesthesia can be influenced. With low concentrations of anesthesia, mainly thin nerve fibers are blocked, which are responsible for the transmission of pain. Only with higher doses can the doctor achieve temporary paralysis of the muscles with this anesthetic technique. This is because motor nerve fibers are much thicker than sensory ones.
The procedure itself also distinguishes spinal anesthesia from epidural anesthesia. With spinal anesthesia, the anesthetic is released into the nerve water ( Liquor) injected. The nerve water surrounds all the nerve fibers of the spinal cord, so that the anesthetic can spread quickly and the effect sets in accordingly quickly. This can be done in just a few minutes.
While in spinal anesthesia the hard meninges ( Dura mater) has to pierce in order to get to the nerve fluid, the anesthetist gives the anesthetic in the so-called epidural anesthesia Epidural space. This surrounds the dura mater and mainly contains blood vessels. In contrast to spinal anesthesia, anesthesia reaches the nerve fibers much more slowly, so that the desired effect only sets in with a delay. As a rule, the time span is no longer than 15 minutes. In addition, the doctor rarely paralyzes the lower extremities, as this effect only occurs with highly concentrated anesthetics.
You can find a lot more information under our topic: Epidural anesthesia
Spinal anesthesia vs. general anesthetic
These two types of anesthesia are often recommended to patients for procedures on the lower half of the body. But which one should he choose? Both methods have advantages and disadvantages that result from the different approaches to anesthesia.
In spinal anesthesia, the anesthetic is injected into the nerve fluid in the lumbar spine area ( Liquor) given. This flows around the nerve fibers of the spinal cord, so that the anesthesia starts quickly and ensures local freedom from pain and the inability to move. It is important with spinal anesthesia that the patient remains completely awake. This has the advantage that the patient can, if necessary, cooperate during the operation and simply communicate his or her state of health. At the same time, however, this is also a disadvantage, since most patients are reluctant to experience an operation on their own body. In severe cases, this can lead to psychological consequential damage.
With general anesthesia, the patient does not notice the operation. In this method, the patient is given an anesthetic before the procedure, either intravenously or through a gas into the lungs. This ensures painlessness, sleep and amnesia. This means that the patient forgets everything that happened shortly after the operation. This makes the procedure a lot easier, especially for anxious people.
Since the body slows down breathing considerably during general anesthesia, the patient must be ventilated during the operation. This is usually done via a thin tube (tube) that is inserted into the windpipe through the mouth or nose. A remedy is often given beforehand to relax the larynx. This prevents injuries to the vocal cords or the upper airways. However, intubation can injure gums, teeth or the vocal cords. During the operation, the anesthetist continuously monitors the status of the anesthesia, as well as pulse, blood pressure and oxygen levels. Depending on the situation, he can react to irregularities with different drugs. Shortly before the end of the procedure, the anesthetist reduces the dose of anesthetic so that the patient slowly wakes up. Due to the amnesia, the patient is not aware of the removal of the tube and the operating room.
In summary, spinal anesthesia is the variant that is afflicted with far fewer complications. However, for many patients the fact that they are still awake during the procedure and are actively witnessing the operation is reason enough to opt for general anesthesia.
How painful is spinal anesthesia?
Since the spinal anesthesia to the spinal anesthetic procedures heard, she is different ways of avoiding and controlling pain consider. At the puncture site on the back, all will descending nerve fibers anesthetizedso that they can no longer guide the pain. Also the motor fibers become paralyzed. The patient feels, even though he is awake and fully conscious during the procedure, no pain.
Which of course light pain caused is that Puncture in the back, which, however, also after local anesthesia is carried out. If pain occurs in the anesthetized area during the operation, the anesthetist can at any time Inject the required dose of anesthetic. Because of the direct accessibility of the nerve fibers occurs an effect very quickly and the pain will decrease again. Even after the operation Spinal anesthesia offers convincing freedom from pain, as there is the possibility of re-injecting.
However, the spinal anesthesia is also not entirely free from side effectswhich sometimes also cause pain. This includes Back pain as well as the rare so-called postspinal headache. Should it come to undesirable effects, can usually quickly counteracted become. Added to this are the classic risks that every invasive procedure entails, such as Infection of the injection site or the Formation of bruises. Pain also occurs here, but that too self-limiting are.
Some people are under regional anesthesia skeptical opposite, as they can not imagine how, for example, one in the waking state Appendix surgery can experience without pain. In general, it must therefore be pointed out that the spinal anesthesia is applied to the desired body regions no pain under the puncture can arise. Studies have even shown this anesthetic procedure also beneficial for postoperative pain is. Patients have reported less pain after this type of anesthesia compared to general anesthesia and were able to recover more quickly.
So the spinal anesthesia is one safe and easy to control methodthat in many interventions routinely is used.
Complications
Since spinal anesthesia also paralyzes nerve fibers that control vegetative functions in the body, problems usually arise here. Often, blood vessels in the anesthetized parts of the body can no longer contract properly, which leads to a drop in blood pressure. To counteract this, the anesthetist gives liquid by means of an infusion and gives supportive vasoconstricting medication. If the anesthetic effect subsides, this problem disappears again. In addition to hypotension, the bladder is often unable to empty properly, which can lead to a build-up of urine in the bladder, which requires the temporary insertion of a urinary catheter. Most of the time, this problem resolves itself over time. Cardiac arrhythmias, nausea and vomiting can also occur .
A significantly more dangerous complication is bleeding in the area of the spinal canal. This occurs more often in patients who have a tendency to bleed or after taking blood-thinning medication. Such bleeding can form hematomas, which compress the nerve fibers and thus lead to pressure damage. In extremely rare cases, this complication can even lead to paraplegia.
Read more on the topic: Xarelto®
As with all invasive procedures, a needle stick during spinal anesthesia can lead to infection. In fact, infections are a rarity in spinal anesthesia.
Neurological complications in the sense of damage to the spinal cord or nerves are - although feared - also very rare.
On the other hand, the rather unpleasant so-called post-puncture headache and back pain after the puncture are more common.
Read more on the topic: Spinal anesthesia complications
What pain do I have afterwards?
Depending on the anesthetics used, spinal anesthesia eliminates pain in the parts of the body at the level of the puncture site and below it for a period of about 1.5 to 6 hours. Only the sensation of pressure and the movement of the body parts should still be intact. Nonetheless, spinal anesthesia can also have painful side effects.
Back pain after anesthesia around the puncture level is quite common. The pain can be radiated into the legs or higher back. These can last for some time, but are ultimately self-limiting - after a few days the pain usually subsides without leaving any lasting discomfort. In most cases, back pain after spinal anesthesia is harmless, but should still be mentioned during the next visit.
Another typical complication after spinal anesthesia is headache.These are referred to as post-spinal or post-puncture headaches and, similar to post-puncture back pain, usually improve after a few days without leaving any permanent damage.
a headache
Headaches after spinal anesthesia are unfortunately a typical problem of the procedure. Medical professionals speak of postspinal headaches, which, depending on the definition, are described in 0.5 - 18% of patients and occur on average two days after spinal anesthesia. Young women often suffer from headaches.
The origin of headaches can be explained by the anatomical conditions in the spine and around the brain. In spinal anesthesia, the hard meninges (dura mater), which also covers the spinal cord in the spine, are pierced. The cerebral water is located within the space that is surrounded by the hard meninges (Liquor). The puncture may injure the dura to such an extent that it has not healed in a few days. When more CSF escapes than the body produces, the pressure in the CSF space drops. The CSF loss syndrome occurs, which is assumed to be the cause of the headache after spinal anesthesia.
These are different mechanisms that cause headaches. The negative pressure causes stretching of sensitive nerve fibers and structures, which causes pain. For this purpose, the brain can slide downwards within the skull, which is why venous vessels are compressed. As a result, the blood can no longer drain off sufficiently and thus cause increased intracranial pressure. This also causes a severe headache. This also explains why the pain is better when lying down than when sitting or standing. A regulatory widening of the vessels is also discussed. A combination of all mechanisms is probably responsible for the headache.
Now it must be said, however, that post-spinal headaches have an extremely good prognosis and usually go away on their own without leaving any permanent damage. Treatment usually consists of the administration of classic headache medication (ibuprofen, paracetamol, ...) as well as bed rest and adequate fluid intake.
If the headache persists, it can be assumed that the leak did not close by itself. In this case, it is possible to close the CSF leak with a blood patch made from a few milliliters of autologous blood. The coagulation of the blood closes the hole in the skin of the spinal cord, so that sufficient new water can form and the pain can subside.
Using special needles can reduce the likelihood of headaches after spinal anesthesia. It is important that you should ask the anesthetist during the consultation before the spinal anesthesia whether you have suffered from this type of headache before, as it is then likely to recur and another anesthetic method may be chosen.
For more information, read on: The CSF loss syndrome.
Back pain
Unfortunately, back pain is a common side effect of spinal anesthesia - up to 10% of patients suffer from these symptoms. Because of this, anesthetists may decide against the procedure if the patient is suffering from chronic back pain.
The cause of the complaints has not yet been fully clarified and an exact allocation to the anesthesiological procedure, the operation or the position during the procedure is usually not possible. The good news, however, is that back pain typically only lasts a few days and then subsides.
Back pain after spinal anesthesia can also occur in combination with post-puncture headache. They can also be a symptom of the so-called “transient neurological symptoms” (TNS) - a rather rare complication of local anesthetics, which have a toxic effect on nerve fibers. The pain occurs within a few hours after applying the spinal anesthesia and subsides within days without any consequences. Neurological failures and fever are classic accompanying symptoms of TNS.
Finally, back pain after the puncture can also indicate an infection at the puncture site. Other signs of this would be neurological failures, fever and reddening of the puncture site. However, infections during spinal anesthesia are a very rare complication.
Long-term consequences
Long-term effects that are directly related to the spinal anesthesia do not occur. As already described under Risks, undesirable side effects of local anesthetics disappear over time and usually do not cause permanent damage. Nerve injuries, such as those caused by needlestick injuries, are extremely rare. On the one hand, this is due to the fact that spinal anesthesia has now become a routine procedure that is often practiced in clinics and thus shows a high level of safety through experience. In addition, rounded needles are used for spinal anesthesia to minimize the risk of injury. If nerve damage occurs due to mechanical irritation, there can be long-term consequences. These primarily include loss of sensitivity of the skin in delimitable areas. Paralysis or even paraplegia are not to be expected if carried out properly. Bacterial infections can cause extensive permanent damage to the spinal canal or the central nervous system. Sterile work prevents such complications.
Read more about the long-term effects of spinal anesthesia
Contraindications
There are in the assessment, which of the existing anesthetic procedures is suitable for a specific procedure and patient, some contraindicationswho speak against the use of spinal anesthesia. Absolute contraindications, for which spinal anesthesia should not be performed under any circumstances, can be obtained from relative contraindications distinguish. Must here Advantages and disadvantages carefully weighed against each other.
One of the most common contraindications are various coagulation disorders. these can innate be or else deliberately brought about by medication become. In the latter case, the reduced coagulability of the blood can be attributed to the Stop taking medication undo, depending on the agent used, a few hours (Heparin) up to over a week before spinal anesthesia must be discontinued. However one is poor coagulation is an absolute contraindicationas there is bleeding around the spinal cord area and such Paralysis can come.
Spinal anesthesia is also absolutely contraindicated existing bacterial infection. These include the infections affecting the whole body as a sepsis, but also local infectious events occurring at the point of puncture. For example, a severe acne on the back be seen as a contraindication.
Another important contraindication for the use of spinal anesthesia is the presence of a allergy against the local anesthetics used, which you should definitely tell the anesthetist in the preparatory talk.
Likewise, recruits increased intracranial pressure a contraindication. If this is established, it comes very likely to have a severe headache after the anesthesia, so you should choose a different procedure here. In addition, a so-called one that has already occurred speaks also postspinal headache against spinal anesthesia.
As the last absolute contraindication is the Hypovolemia to call, so a Volume depletion with decreased circulating in the circuit Amount of blood.
In contrast to the previously mentioned contraindications, the use of spinal anesthesia is in the presence of relative contraindications possibly possibleafter weighing the risk and benefit in favor of the patient.
To the relative contraindications a spinal anesthesia chronic back pain or the ankylosing spondylitisin which the spine stiffens. Valvular heart disease, one narrowed aortic valve (Aortic valve stenosis) and a increased blood pressure in the pulmonary circulation can also be contraindications.