Staph infection
What is staph infection?
A staphylococcal infection describes the penetration of the staphylococcus bacteria into the organism with a settlement and subsequent increase in the number of bacteria. The bacteria can infect the organism via different access routes.
Often an infection occurs through wounds.
Infection is also possible, for example by means of an indwelling venous cannula or central venous catheter (CVC), which are often used in hospitals to draw blood from the patient or to administer medication.
Infection with bacteria of the genus Staphylococcus can occur through different species or subspecies such as Staphylococcus aureus or Staphylococcus epidermidis.

These are the symptoms you can tell if you have a staph infection
Because staph can cause a wide range of diseases, there is a great variety in symptoms as well.
It must also be remembered that not every symptom is specific to a staph infection, but can also have other causes. Reliable detection of staphylococci can only be achieved through microbiological cultivation.
If pus forms as part of a staphylococcal infection such as a boil, carbuncle or abscess, for example, pain and possibly also paresthesia often occur. Depending on the location, there may be additional, secondary symptoms that are caused by the affected tissue.
A wound infection usually shows the typical signs of overheating, swelling, pain, reddening and dysfunction.
If sepsis with phlegmon develops, the symptoms can also be palpitations, increased breathing rate, fever and chills.
Possible urinary tract infections show symptoms of burning sensation when urinating and a frequent need to urinate.
Endocarditis often has many different symptoms. These include fever, chills, palpitations, decreased performance, night sweats, anemia and, in extreme cases, decreased consciousness and involvement of the kidneys.
Staphylococcal Scalded Skin Syndrome (SSSS) first shows a high fever with an accompanying rash, a skin rash. Then an otitis media and pharyngitis (inflammation of the throat) appear. This then leads to the formation of blisters all over the skin with the exception of the mucous membranes, which burst very easily.
How contagious is staph infection?
Transmission is relatively common, especially when there is close contact with an infected person. However, if precautionary measures such as maintaining a certain safety distance or wearing protective clothing are taken, further infections are very rare. Nevertheless, staphylococci pose a high risk of infection because, depending on the resistance, they are very difficult to kill.
Staphylococci are largely transmitted through direct contact as part of smear infections. More rarely, staphylococci can also cause further infections through the air.
What diseases are caused by staphylococci?
The diseases that can be caused by staphylococci are diverse. These diseases are also caused by the species or the subspecies.
A wide variety of diseases can result from infection with Staphylococcus aureus. Symptoms typically occur that are related to the formation of pus.
Boils, carbuncles and abscesses can form in the skin.
A purulent brain abscess can also develop.
In addition, endocarditis, an inflammation of the inner lining of the heart, which corresponds to a special form of pus formation, often occurs.
Furthermore, pneumonia, or pneumonia, can develop.
Staphylococcus aureus infection of wounds is also common. In the case of pus formation or wound infections, there is a risk that the bacterium will develop in the blood in the entire body, which can lead to life-threatening multi-organ failure, known as sepsis.
Rarer diseases are the "Staphylococcal Scalded Skin Syndrome" (SSSS), the "Toxic Shock Syndrome" (TSS) or food poisoning with the toxin of the bacterium.
When infected with the bacterium Staphylococcus epidermidis with simultaneous immunosuppression, which is a normal skin germ, sepsis is very common. This route of infection is the most common route of hospital-acquired infections.
Other Staphylococcus species such as Staphylococcus saprophyticus can also often be the cause of urinary tract infections.
Tonsillitis caused by staphylococci
In addition to a wide range of causes, tonsillitis can also be caused by an infection with staphylococci. This infection can occur after minor injury to the mouth and throat such as an injury to the mucous membrane by a sharp object.
Often the affected person also suffers from inflammation of the nasal and sinus lining as well as inflammation of the upper respiratory tract such as the bronchi.
symptoms of tonsillitis are
- Swelling and redness of the tonsils
- Sore throat
- difficulties swallowing
- Body aches
- possibly fever
- Loss of appetite.
The tonsillitis is treated with symptomatic therapy such as lowering the fever and, in severe cases, with the administration of an antibiotic.
Learn more about the causes, symptoms and treatment options for a Tonsillitis.
Abscess formation due to staph infection
Abscess formation by staphylococci only occurs in infections with Staphylococcus aureus.
The reason for this is that, in comparison to other species or subspecies, some enzymes are present in this species, which are the prerequisite for abscess formation.
These enzymes include those that can actively decompose the tissue of the affected organism and thus penetrate far into the tissue. Examples of these enzymes are a collagenase, a lipase and hyaluronidases. These enzymes mainly degrade the connective tissue, creating an area in which necrotic, i.e. dead, cells predominate.
In connection with the initiated immune response, which is strongly dependent on granulocytes, pus develops.
A wall of fibrin is formed around this purulent area, which protects the bacteria and thus enables a massive increase in the number of bacteria. At the same time, the bacterium has an enzyme, fibrinolysin, which can open the fibrin wall. This enables the bacterium to penetrate massively into the surrounding, intact tissue and the bloodstream after it has multiplied. This can lead to life-threatening sepsis, which is why a doctor should usually be seen in the event of an abscess.
Have you a Abscess? Find out what you can do about it.
Staphylococci as a cause of pimples
A pimple represents an inflammatory change in the skin. This change occurs when a skin pore becomes blocked, which can be caused by various substances.
Among other things, sweat or sebum can cause a blockage, creating good conditions for colonization by pathogenic bacteria such as staphylococci.
A pimple is one of the skin changes of the primary efflorescences, which always have a disease value. As a rule, there are no complications when a pimple appears.
In extreme cases, however, the pimple can spread to a boil, carbuncle or abscess with the risk of developing sepsis.
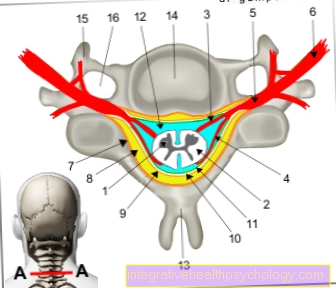
Staphylococcal sepsis
Staphylococcal sepsis occurs when there is a massive increase in the number of bacteria in the blood, which triggers a strong immune response, but also carries the risk of fatal multiple organ failure.
The entry portal of the staphylococci can be localized in different ways.
On the one hand, after the formation of an abscess, the staphylococci can infiltrate the supplying blood vessels by infiltrating the surrounding, intact tissue.
On the other hand, skin wounds have good conditions for the bacteria to also infiltrate the vessels.
Furthermore, indwelling venous cannulas and central venous catheters (CVC) pose a particular risk for the development of staphylococcal sepsis.
The specialty of the staphylococci genus is the formation of a biofilm that protects them, in which they can multiply and enable the bacteria to migrate along the indwelling cannulas and CVCs into the blood vessels.
Various species can be held responsible for the development of staphylococcal sepsis. ly the species Staphylococcus aureus and Staphylococcus epidermidis come into consideration for this.
These species can produce a superantigen, a product of the bacteria, which causes a massive response from the immune system. This usually leads to multiple organ failure with potentially fatal consequences.
Staphylococcal sepsis occurs more frequently in women who use tampons during menstruation, as these create good conditions for the bacteria to multiply. From here, it is not the bacterium but the superantigen that gets into the bloodstream and unfolds its effect.
Skin infections caused by staphylococci
Not every detection of bacteria of the genus staphylococci on the skin is of disease value.
Many species of staphylococci such as Staphylococcus epidermidis are part of the normal skin flora.
In addition, infection of the skin by staphylococci is usually not a problem in immunocompetent individuals, as the immune system is able to fight the infection effectively when it enters the body.
In the case of immunodeficiency, however, these bacteria sometimes pose a health risk, as, for example, there is a risk of infection if a wound is suffered.
In addition to unproblematic species of staphylococci, some people also have pathogenic staphylococcal species that pose a threat to the environment. These can serve as a source of infection for other people or, if they enter the bloodstream, cause considerable damage to the person's health.
This is particularly problematic in hospitals, where special staphylococcus species are a frequent cause of hospital infections with fatal consequences.
Staph infection of the bone
A staph infection can also affect the bone. This condition is called osteomyelitis. Osteomyelitis affects both the bone substance and the bone marrow.
There are many causes of osteomyelitis, but bacteria often play an important role. In particular, multi-resistant hospital germs such as staphylococci can cause an infection postoperatively.
Osteomyelitis is noticeable through the typical signs of inflammation such as swelling and reddening. In addition, pain and pus can occur.
The treatment of osteomyelitis usually consists of a surgical procedure in which the respective focus of inflammation and pus is removed, or an intravenous administration of antibiotics. In the case of anaerobic bacteria, it is also possible to work with the introduction of oxygen. In extreme cases, an amputation of the affected part of the body is necessary.
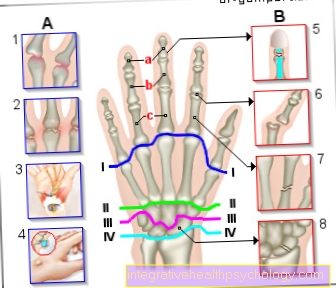
Staph infection in the knee
A staph infection can also affect joints such as the knee. This infestation is called pyarthrosis (purulent knee joint effusion).
Typical signs of a staph infection in the knee are the classic signs of inflammation redness, swelling, pain, overheating and functional impairment.
The finding can only be confirmed by a joint puncture.
A confirmed infection of joints such as the knee is always an indication for emergency orthopedic surgery, whereby the inflamed tissue is removed. In the case of advanced damage, the use of a knee prosthesis may be necessary.
Staph infection of the eye
Staphylococci can also infect the eye or the tissues associated with the eye.
This includes, among other things, the tear sac.
The basis of dacryocystitis, an inflammation of the tear sacs, is the reduction in the outflow of tear fluid from the tear sac. This creates conditions that are good for fungi or bacteria such as staphylococci to colonize.
Typical signs are the one-sided appearance, increased secretion of tear fluid, redness, swelling and pain.
Therapy is usually complicated and depends on several factors, which is why a doctor should be consulted.
Another eye disease caused by staphylococci is the formation of stye.
After the closure of a sebum or sweat gland on the inside of the eyelid, an infection with bacteria occurs.
This leads to redness, swelling, pain, and the secretion of pus.
Therapy consists of using warmth and, if necessary, giving eye ointments or eye drops that contain antibiotics.
What is MRSA?
MRSA originally stands for methicillin-resistant Staphylococcus aureus and means bacteria of the species Staphylococcus aureus, which have developed a variety of resistances to methicillin and later other antibiotics.
Nowadays the term MRSA is usually translated as multi-resistant Staphylococcus aureus, which is incorrect, but is often used because these bacterial strains have a large number of resistances to antibiotics.
MRSA is referred to as a typical hospital germ, as it occurs more frequently here and is responsible for a large number of hospital infections, including fatal ones.
On the one hand, the germ occurs on many surfaces that are not properly cleaned. On the other hand, the germ colonizes a large number of patients and hospital employees, who can also be a source of infection.
Since infection with MRSA poses a high health risk, risk groups are screened before hospitalization and infected patients are isolated in hospital. MRSA infection is treated with special antibiotics such as vancomycin or linezolid. For the rehabilitation of MRSA carriers who are not sick, full-body disinfecting baths are recommended.
Would you like to learn more about MRSA? Read our articles on MRSA and Multi-Resistant Hospital Germs.
Therapy of a staph infection
A staphylococcal infection is not necessarily treated if it is suspected and after it has been proven.
Since some staphylococcal species belong to the normal skin flora, further differentiation has to be made.
Even the species Staphylococcus aureus, which can cause considerable damage in the body, is not necessarily treated if it is detected on the skin.
However, if it is detected in the context of a blood culture or if symptoms are found that are compatible with an infection by staphylococci, antibiotic therapy is used. Different active ingredients are used for this, depending on the species and the resistance of the bacteria to some antibiotics.
As gram-positive bacteria, staphylococci are generally sensitive to beta-lactam antibiotics such as penicillin.
However, because of resistance or allergies, other antibiotics such as clindamycin, erythromycin or rifampicin are often used.
Methicillin-resistant Staphylococcus aureus (MRSA), in which vancomycin or teicoplanin is used as a reserve antibiotic, is a special case.
Learn more about Treatment with antibiotics and the Side effects of antibiotics