Breastfeeding- All You Need To Know
What is the breastfeeding period?
The period when the child drinks breast milk from the mother's breast is called breastfeeding. Breastfeeding begins right after birth. The children are placed on the mother's breast as early as possible. On the one hand, this supports the connection to mother and child immediately after birth, and on the other hand, the mechanical stimulus of sucking on the breast is extremely important for the mother's milk production. Especially at the beginning, it is often unusual for the mother to lay it against the breast and it requires patience. Over time, however, mother and child get used to it more and more. If you have any questions, you can always contact your midwife.

How long should you ideally breastfeed?
Breast milk is the best food for your child. How long the child should optimally be breastfed is still controversial.There is no generally applicable recommendation in Germany. It is believed that exclusive breastfeeding in the first six months is good nutrition for healthy, mature babies. Depending on how the child develops, it may be necessary to give the child complementary food before the age of 6 months. However, this should not be done before the 4th month. If the child develops normally, it should be fed no later than the 7th month of life. It is important that complementary food does not mean immediate weaning, but that breastfeeding is also carried out. It has been proven that feeding exclusively with breast milk in the first 4-6 months of life reduces the risk of an allergy in the child (disease of the atopic group of forms).
Here you can find the main page: Breastfeeding
nutrition
What diet should you watch out for while breastfeeding?
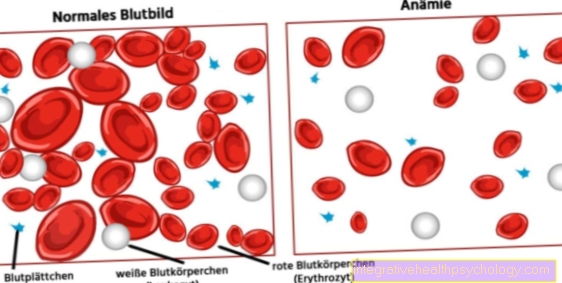
There is actually no need for a special diet during breastfeeding. As in any situation in life, one should eat a balanced and conscious diet. These include whole grain products, fresh fruits and vegetables, and foods rich in calcium and iron, such as milk and legumes. Due to the milk production and the passing on of nutrients to the child, the mother still needs additional calories. Only with the slow weaning of the child does the calorie requirement also decrease. In the first four months, the mother needs between 400 and 500 kcal in addition to her normal consumption. After that, any complementary food decides on further requirements. This means that the need for more calories is even greater than during pregnancy. If you eat according to your appetite and in a balanced way, additional fat reserves from pregnancy will be used up and your body weight will decrease. An additional, strict diet is not recommended, as insufficient calorie intake can reduce the amount of milk. You should also drink enough.
Read more on the topic: Diet while breastfeeding
Can you drink alcohol while breastfeeding?
Alcohol consumed by a nursing mother passes into the child's body through milk and can cause harm. Therefore, the best recommendation is not to drink alcohol while breastfeeding. 30-60 minutes after consuming alcohol, it can be found in breast milk. You should avoid alcohol, especially in the first month after the birth of the child. If you still want to drink one or two glasses of alcohol every now and then, there are a few things to watch out for. You should breastfeed your child shortly before drinking alcohol so that the time until the next breastfeeding is as long as possible. As in the mother's blood, the alcohol content in breast milk has decreased over time since consumption. The rule of thumb is that 10 g of alcohol are broken down by the body in two hours (1 bottle of beer = 12.7 g; 1 glass of wine = 8.8 g of alcohol). However, every body breaks down alcohol at different rates. Eat before you have any alcoholic drink. If you are unsure whether the alcohol has already broken down, it is advisable to have expressed milk beforehand so that you can give it to the child when he or she is hungry again. Overall, it is possible to drink alcohol occasionally while breastfeeding, but this should be done responsibly and thoughtfully.
More information on this topic: Alcohol while breastfeeding
Is alcohol-free beer allowed?
By definition, an alcohol-free beer has an alcohol content of less than 0.5% vol. It is not completely alcohol-free, but the amount is so small that it has no physiological effects on the body. This means that you can drink a non-alcoholic beer every now and then while breastfeeding. Due to the natural fermentation process, fruit juices also have a minimal alcohol content. Studies have shown that consuming 1.5 liters of alcohol-free beer within an hour increases the blood alcohol concentration to 0.0024 per mille. However, this small amount had already been reduced again within the next half hour. Some experts even say that alcohol-free beer boosts milk production and they recommend consumption in moderation.
Can you drink coffee while breastfeeding?
Caffeine should be consumed with caution during breastfeeding as it passes into breast milk. The child's body cannot process caffeine as quickly as an adult. It takes him about three days to do this. In an infant, this can cause abdominal cramps, restlessness, and gas. For this reason, breastfeeding mothers are advised to consume moderate amounts of caffeine as soon as possible after breastfeeding. In total, no more than 300mg of caffeine should be consumed per day. In comparison, an espresso has around 50mg of caffeine, a cup of filter coffee (125ml) around 80-120mg and 200ml of cola has around 20-50 mg of caffeine. Herbal and black tea should also be enjoyed with caution, as the caffeine content varies depending on the steeping time.
You can find more information at: Coffee during breastfeeding- what you need to consider!
Can you smoke while breastfeeding?
The nicotine of the cigarette and other toxins pass directly into the breast milk. Nicotine has a concentration three times higher in breast milk than in the mother's blood. Children of smoking mothers are more likely to show restlessness, lower pumping speed, colic and vomiting. In addition, heavy smoking can inhibit the mother's milk production. Therefore, the best recommendation is not to smoke at all while breastfeeding. If the mother fails to do this, the question often arises whether it is better to stop breastfeeding or to continue breastfeeding despite smoking. In general it can be said that the child should still be breastfed, as the benefits of breast milk outweigh the above. A few things should be observed here so that the burden on the child is as low as possible. Smoke immediately after breastfeeding, as the highest nicotine concentration is found in breast milk shortly after the cigarette and the time until the next breastfeeding is then greatest. After about 95 minutes, only half of the nicotine concentration can be measured. It is best to stop smoking two hours before breastfeeding. Do not smoke in the home or around the child and wash your hands afterwards. Overall, try to limit your smoking as much as possible.
Read more on the subject at: Smoking while breastfeeding- how dangerous is it?
Can you lose weight while breastfeeding?
The mother's body consumes 400-500 kcal in addition to the normal calorie consumption through milk production. A certain decrease in the mother's fat reservoir is even provided by nature. The composition and fat content of breast milk are always approximately the same, regardless of what the mother has ingested. Therefore, the child is usually adequately nourished. However, if there is very severe weight loss, this can negatively affect the amount of milk produced. If the mother loses weight, attention should therefore always be paid to the growth of the child. In total, the mother should not lose more than 500g per week. If you combine the increased calorie requirement with a healthy and balanced diet, the body often manages to shed excess kilos on its own. However, this is different for everyone. Avoid sweets and very fatty foods and watch your body and your child.
Read more about this: Lose weight while breastfeeding
Can you eat chocolate while breastfeeding?
Of course, when you are breastfeeding you can give in to any cravings and reach for chocolate. Like almost everything, this should always be done in moderation, as chocolate can have a few negative effects. On the one hand, sweets naturally settle on the hips quite quickly and can lead to weight gain. On the other hand, chocolate also contains caffeine, the consumption of which should be limited to 300mg during pregnancy. A 100g bar of dark chocolate contains 90mg of caffeine and a whole milk chocolate bar contains 15mg. With an additional daily coffee or the like, for example, the 300mg can be reached quickly and can lead to restlessness in the infant. Also, chocolate is considered to be a flatulent food that can cause stomach pain in your child.
Is raw meat allowed during breastfeeding?
During pregnancy, raw meat and raw milk cheese are prohibited because of the risk of toxoplasmosis and listeriosis. After the birth of the child, they can be eaten whole again while breastfeeding. The risk of the above diseases being passed on to the child through breast milk is unfounded. Tartar and raw ham are now back on the menu.
Is cinnamon allowed?
The spice cinnamon contains the substance coumarin, which is considered to be harmful to the liver. There are two different types of cinnamon. Ceylon cinnamon only contains low levels of coumarin, so it is considered harmless. The cheaper cassia cinnamon, however, has a higher, more questionable concentration of coumarin. The consumer cannot distinguish between the two types. You shouldn't consume more than 0.1 mg of coumarin per kilogram of body weight per day. Since this is difficult to control, caution is advised with cinnamon. You should therefore limit your cinnamon consumption while breastfeeding. You should therefore avoid the cinnamon stars, especially in the run-up to Christmas.
Is licorice allowed?
Liquorice should only be consumed in small amounts during pregnancy, as the ingredient glycyrrhizic acid is suspected of raising blood pressure and, if taken during pregnancy, of lasting disruption to the child's physical and mental development. No scientific knowledge is available for breastfeeding. It is therefore recommended, as in pregnancy, to limit the consumption of licorice to 100g per day. Liquorice can also change the taste of breast milk and is suspected of causing gas in an infant.
What are the consequences of eating citrus fruits while breastfeeding?
There is also a wide variety of experience reports with citrus fruits. A sore bottom in the child has been reported more frequently after the mother has consumed orange juice or lemons, for example. Here, too, try out whether your child is sensitive and how much citrus fruit is still okay.
Can you eat spicy while breastfeeding?
One often hears that spicy food can lead to skin irritations and a sore bottom in breastfed children. However, this has not been scientifically proven, but is based on experience reports from breastfeeding mothers. This shows that you can eat whatever you and your child can eat. However, if your child is more restless after a spicy meal or if the skin changes, then leave out spicy food and see how the abnormalities change. So the motto is: try it out and then adjust your eating habits.
Flatulence while breastfeeding
In principle, while breastfeeding you can eat anything that you and your child can tolerate. The general statement that children cannot tolerate certain foods when they are consumed by their mother and that they should therefore be avoided is unfounded. However, there are very sensitive children who react to certain foods with gas, abdominal pain or sore skin. It often takes a few tests and a little trying out what is tolerated and how well. Flatulent foods, such as some types of cabbage, can lead to intolerance not only in the mother but also in the infant. These include, for example, savoy cabbage, sauerkraut, onions or legumes. Broccoli or kohlrabi are considered milder and are therefore good starting points. If these are well tolerated, other types of cabbage can be tried. In children, gas is often caused by swallowing air and it is difficult to distinguish it from food intolerance. The swallowed air is caused, for example, by an unfavorable breastfeeding method. The so-called "peasant" can help after breastfeeding.
More information on this topic: Flatulence while breastfeeding
What are the consequences of eating too much onions while breastfeeding?
Onions are suspected of causing gas in infants. But, as almost always, it is said that the dose plays an important role. Not every child reacts in the same way and some children do not mind onions at all, while others are very sensitive. Therefore, it is said that onions should simply be tested and the changes observed. Abdominal pain in children can have many reasons, but if there is a link to onions, it is better to avoid them.
Medication
What medications should I not take while breastfeeding?
The use of medication while breastfeeding should only be justified if the active ingredient either does not pass into breast milk or if it does not cause harm to the infant. In principle, however, many drugs are no reason to wean. You should always discuss with your doctor or pharmacist which drugs cause potential damage and should therefore be avoided. You may only need to take a break from breastfeeding. A website of the Federal Ministry of Health www.embryotox.de gives a good overview. In the case of mild complaints, you should consider whether a medicine is really needed or whether harmless home remedies might be sufficient. In the case of chronic illnesses and related drug intake, you should discuss the procedure with your doctor. In principle, you should always take medication a few hours before the next breastfeeding meal, so that the mother's body can convert part of the active ingredient. Each drug must be checked individually and critically questioned in order to ensure the best possible protection for the child.
continue reading: Medication during breastfeeding
Ibuprofen while breastfeeding
Ibuprofen belongs to the group of non-steroidal anti-inflammatory drugs (NSAIDs). It is a pain reliever, anti-inflammatory and antipyretic drug and is often given for headaches or rheumatoid arthritis, for example. Ibuprofen is considered the pain reliever of choice when breastfeeding. No damage was found in breastfed children.
Read more about this: Ibuprofen while breastfeeding
Paracetamol while breastfeeding
Paracetamol is a pain reliever and antipyretic drug. It is not anti-inflammatory and is mainly used for mild to moderate pain. The use of paracetamol while breastfeeding is considered safe. So far, no negative effects or intolerance have been found in a breastfed child. Therefore, paracetamol is considered to be the pain reliever of choice for breastfeeding alongside ibuprofen.
Aspirin while breastfeeding
The active ingredient acetylsalicylic acid in aspirin is considered an analgesic for mild to moderately severe pain. It has an antipyretic, anti-inflammatory effect and is used to inhibit coagulation. Aspirin is not prohibited per se during breastfeeding. An occasional intake of 1.5 g as a pain reliever appears to be justifiable. However, ibuprofen and paracetamol are preferred as pain relievers. The use in an anti-rheumatic dose of 4g per day is not recommended. With a dosage of 100-300mg per day, aspirin may be taken regularly.
Which antibiotics can you take while breastfeeding?
Infections during breastfeeding are often caused by bacteria and therefore require antibiotic therapy. Symptoms from the drug are not very common in breastfed children. The infant occasionally experiences diarrhea. Most treatments during pregnancy and breastfeeding are based on beta-lactam antibiotics. These include penicillins, carbapenems, cephalosporins, and monobactams, with penicillins and cephalosporins being best studied during pregnancy and breastfeeding. A combination with beta-lactamase inhibitors such as clavulanic acid is possible. Together they are considered the first choice for breastfeeding. Macrolides are also available for people with allergies. Discuss any antibiotic use with your doctor. They can select the best antibiotic for you and your child.
Chest pain while breastfeeding
Chest and nipple pain are a common symptom while breastfeeding. Especially shortly after the birth, breastfeeding often hurts despite the correct breastfeeding position, as the nipple is still particularly sensitive and has to get used to sucking the child.An incorrect breastfeeding position can also lead to immediate breastfeeding pain. In order for the child to drink effectively, they must also put a large portion of the areola in their mouth. If this does not happen, the nipple will be pushed too hard and hurt. It can also injure the nipple. Therefore, you should practice the correct positioning of the child with an experienced person.
As a result of the milk penetration, the mammary gland can swell significantly. Some women find the increased pressure painful. Furthermore, the milk is transported towards the nipple with the help of the smallest muscle contractions. This can be perceived as painful. The causes of pain mentioned so far are usually limited in time and are directly related to the breastfeeding of the child. Persistent and recurring chest pain should be clarified and the mother should be advised by the midwife or doctor. Sometimes there is an anatomical cause. For example, a particular shape of nipple can prevent effective drinking. Here, for example, nipple shields can help. A child's tongue that is too short can also cause problems when breastfeeding. Breast congestion can also cause chest pain. Regular emptying of the chest is advisable. Bacterial or viral inflammation in the breast is common. In so-called "mastitis", bacteria get into the breast. Redness, swelling and pain occur locally. You may also experience a fever, chills, and body aches. Mastitis should be examined by a doctor and treated with antibiotics and regular breast empties.
You might also be interested in this topic: Milk congestion such as Painful breastfeeding
Do I have to use contraception while breastfeeding?
In non-breastfeeding mothers, the period starts again six to eight weeks after the birth. During lactation, ovulation is inhibited by the release of prolactin, so that bleeding can stop for several months. During this time, you are theoretically protected against a new pregnancy. However, it is important to remember that the first ovulation and thus the possibility of pregnancy takes place before the first menstrual period. In order for the so-called “lactation amenorrhea method” (LAM) to work safely, three important points must be observed.
First, the mother must not have had any menstrual bleeding (bleeding from the vagina from the 56th day after birth). Second, the child must have been fully breastfed without interruption since birth, including at night (at least six times a day with a maximum of six hours' break). Third, the infant cannot be older than six months. If all these points are considered, there is a protection against pregnancy of 98-99% and is therefore quite safe. If not every point can be answered in the affirmative, further contraception methods should be considered. This includes, for example, barrier protection such as condoms or a diaphragm or the insertion of a coil by the doctor. Not all contraceptive pill preparations may be taken during breastfeeding. It is best to discuss the next steps with your gynecologist before the birth or during your first follow-up examination.
Do you get your period while breastfeeding?
Regular breastfeeding releases prolactin through sucking on the breast. On the one hand, this is responsible for milk production; on the other hand, it inhibits the hormones FSH and LH. These are essential for ovulation. If they are suppressed, there will be no ovulation and thus no menstrual period. Therefore, breastfeeding can stop your period. If a mother is exclusively breastfeeding her infant, there is a high likelihood that ovulation, and therefore menstruation, will not occur for several months. However, this requires very regular application to the chest. If you fully breastfeed your child day and night, it can be up to a year before their period starts again. For example, if the child sleeps through quite early and the intervals between breastfeeding are longer, you will probably have your menstrual period earlier - on average, usually between three and eight months.
Will the child with the Bottle nourishes, your period can return as early as six weeks after the birth. Sometimes it takes two to three months. The first period after the birth can be very heavy and painful or sometimes it is hardly distinguishable from the remaining weekly flow. Thus the strength and regularity after the birth is very variable and it takes time for the body to return to its old rhythm.
Can I tint my hair while breastfeeding?
When you dye your hair, the body can absorb tiny amounts of the dye through the scalp. However, the manufacturers of the dye products already take into account during product development that all ingredients can be used safely by pregnant and breastfeeding women. Only products approved by the European Union's Scientific Cosmetics Committee may be used. The Federal Institute for Risk Assessment (BfR) says that there is no evidence of health risks from hair dyes during pregnancy and breastfeeding.
Find out more about the topic here: Coloring hair while breastfeeding.
Can you apply nail polish while breastfeeding?
Nail polish and nail polish remover contain solvents and plasticizers. However, these have a very low concentration and the area to be applied on the nails is comparatively very small. If possible, a formaldehyde-free product should be used. In principle, you can also use nail polish while breastfeeding. Make sure that the child is not in the room when applying the nail polish and ventilate thoroughly afterwards due to the smell.
Cystitis while breastfeeding- what to do?
A bladder infection or, more accurately, a urinary tract infection is common in women. A woman can also get it while breastfeeding. There is pain when urinating and an increased need to urinate. It is particularly important to drink a lot and to empty your bladder frequently. Urinary and bladder teas may help. Keep warm to prevent hypothermia. It is often necessary to treat the bacterial infection with an antibiotic. To do this, consult your doctor, who will prescribe an antibiotic that is approved for breastfeeding. Penicillins in particular are considered the antibiotic of choice for breastfeeding. If the pain increases and turns into flank pain, kidney disease is suspected and you should be treated immediately.