Synovitis in the knee
What is knee synovitis?
Synovitis in the knee is inflammation of the lining of the knee joint. The patients suffer from pain, swelling and overheating of the knee joint. The causes of synovitis are varied and range from traumatic injury to rheumatic disease.
In the following article you can learn more about the causes, symptoms and therapy of synovitis in the knee.

The reasons
There are many causes of synovitis in the knee. This inflammation of the synovial membrane is very often caused by excessive (incorrect) stress, e.g. in the context of sporting activities or kneeling work. Furthermore, traumatic injuries such as Bruises in the knee cause inflammation. Pathogens such as bacteria can also penetrate through wounds in the skin in the knee area and attack the synovial membrane.
Infectious diseases such as tuberculosis or the sexually transmitted disease gonorrhea (gonorrhea) can also make themselves felt as inflammations in the knee. Finally, autoimmune diseases such as rheumatoid arthritis or psoriasis should also be mentioned, which can also be the cause of synovitis of the knee. To be able to determine a clear cause of synovitis, you should consult an experienced doctor.
Find out more about the topic here: Synovitis.
Rheumatism as the cause
Rheumatism can also lead to synovitis of the knee. In rheumatic diseases, our immune system falsely attacks the body's own cells. The result is a painful inflammation of various joints. The knee joint can also be affected.
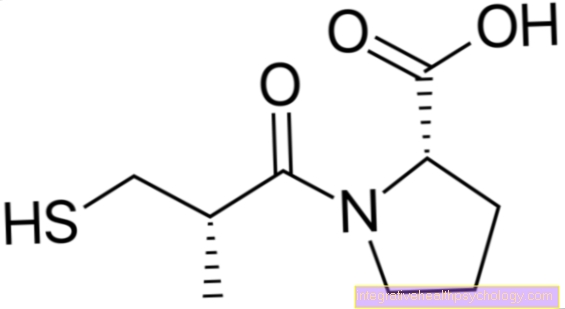
In the case of an acute rheumatic attack, anti-inflammatory painkillers (e.g. ibuprofen) and cortisone are usually used therapeutically. There should be a quick improvement below this. If rheumatic complaints occur frequently, long-term therapy, e.g. can be used with the active ingredient methotrexate. These curb the immune system and can lead to an improvement in the rheumatism in the long term.
For more information, read on: Rheumatism.
Knee TEP as the cause
A knee TEP is an artificial knee joint that can be used surgically, for example in the case of severe osteoarthritis (joint wear) of the knee joint. If this artificial joint becomes infected with pathogens, synovitis can occur. Quick action is required here in order not to have to remove the artificial knee joint again.
The therapy of choice is the treatment in antibiotics, which can also be given directly to the knee joint if necessary. If the inflammation cannot be contained in this way, the removal of the knee TEP may be necessary.
Read more about the topic here: Knee prosthesis
The accompanying symptoms
In addition to the typical symptoms of synovitis on the knee joint (pain, redness, swelling and overheating of the joint), there may be other accompanying symptoms. These include primarily a deterioration in the general condition. Patients feel weak and tired, with a fever and aching limbs. The mobility of the knee joint is painful and severely restricted
If the inflammation spreads, the surrounding muscles and skin can also be affected by redness, swelling and pain. Depending on the cause of the synovitis, other typical symptoms can occur: in rheumatoid arthritis, other joints are often affected by inflammation.
The swelling as a symptom
Synovitis of the knee joint leads to severe inflammation of the inner lining of the knee. A typical symptom is severe swelling of the knee joint. This is caused by the increased blood flow to the joint and the associated storage of water in the surrounding tissue. The swelling and the associated restriction of movement should recede early with the right therapy.
Also read the article: Inflammation of the synovial membrane.
The pain as a symptom
The main symptom of synovitis is severe pain in the knee. This can be expressed by pulsating pain at rest and usually intensify when the knee joint is moved. Shooting, stabbing pains are often described. Mobility is also mostly severely restricted due to pain.
Anti-inflammatory pain medication (e.g. ibuprofen) but also cooling and protection can help. With adequate therapy, the pain should also subside early.
The effusion as a symptom
With synovitis of the knee, it is not uncommon for a joint effusion to develop. This is an accumulation of fluid within the joint capsule. This can cause pain and swelling of the knee.
The joint effusion can be punctured externally by a doctor. This can be useful both to relieve the knee and to confirm the diagnosis, as the drained liquid in the laboratory, e.g. can be examined for pathogens. If the synovitis is treated appropriately, it can take some time for the joint effusion to subside.
The diagnosis
The diagnosis of synovitis of the knee can often be made through physical examination alone. Based on the typical symptoms such as pain, swelling, reddening and overheating of the joint, synovitis can often be safely concluded. Joint effusion can also be detected with the help of orthopedic physical exams. If bacterial inflammation of the knee is suspected, a joint puncture can provide information about the pathogen. In this way, the right antibiotic can be selected in a targeted manner.
If a traumatic injury is suspected, imaging tests such as an X-ray or an MRI can be helpful. An x-ray should also be taken if the artificial knee joint is suspected of being loosened. Should the patient have holistic symptoms such as If you show fever and fatigue, a blood test can be helpful for diagnosis.
What do you see of the knee in an MRI?
While the bony structures can be seen well with an X-ray of the knee, an MRI is used to assess the soft tissues. In the case of the knee, this includes e.g. the menisci, the various ligaments (cruciate ligaments, inner and outer ligament) but also cartilage, tendons and muscles. An MRI can detect inflammatory changes in these areas.
If a traumatic injury is suspected, an MRI may be necessary, as a tear in the meniscus or cruciate ligament can be detected. Possible joint wear and tear can also be identified as the cause of synovitis.
Read on here: MRI of the knee.
The treatment
The treatment for synovitis of the knee is highly dependent on the cause of the knee joint inflammation. Synovitis is most common when the joint is subjected to heavy loads, often in athletes or in patients who do a lot of work on their knees (e.g. when laying tiles). In the next few weeks, these patients should primarily protect their knee joint and refrain from the activity that caused it. Physiotherapy and anti-inflammatory pain relievers such as Ibuprofen contribute to faster healing.
If there is a traumatic injury to the knee joint, it should be treated appropriately. A competent orthopedic surgeon should be consulted here, who can determine the correct therapy. Is it a flare-up of an autoimmune disease such as Rheumatism, the use of cortisone may be necessary. Here, cortisone curbs the excessive body's own defense system and thus helps healing quickly. If the knee joint is infected with bacteria, antibiotics may be necessary.
If an artificial joint is inserted before the knee joint inflammation, you should consult a doctor in good time, as antibiotics must be treated here as early as possible. This can also be done, for example, by using drugs that contain antibiotics directly on the joint. If the inflammation cannot be contained, it may be necessary to remove the artificial joint.
When do you need an operation?
Surgery for synovitis of the knee joint is by no means typical. Most inflammations can be treated well with anti-inflammatory pain relievers or antibiotics while protecting the joint.
An operation can be performed especially in the case of an injury to the knee, e.g. become necessary after a sports accident. An operation can also be performed on a freshly inserted artificial knee joint that has become infected with pathogens. Even with severe signs of wear and tear on the knee, you can think about surgical treatment to prevent further synovitis. In the vast majority of cases, however, no surgery is required.
The radiosynoviorthesis
In the case of chronic inflammatory diseases of the knee joint, for example in the context of rheumatism or activated osteoarthritis, a radiosynoviorthesis can help relieve pain. Here radioactive substances are given into the knee joint, which lead to a change in the synovial membrane. This can often contain inflammation and significantly reduce pain in the knee joint.
You should discuss with your treating orthopedic surgeon or rheumatologist whether a radiosynoviorthesis is indicated.
Also read the article: activated osteoarthritis.
The duration
The duration of synovitis in the knee varies greatly depending on the cause. If there is an incorrect load, the symptoms should decrease quickly with pain therapy and physical rest. However, renewed inflammation when continuing heavy knee loading is common!
If there is a bacterial inflammation, there should be rapid improvement with appropriate antibiotic therapy. Please take the antibiotic exactly as instructed by your doctor and do not stop taking it early if the pain improves!
If there is an injury to the knee, the healing time can of course be extended. If an autoimmune disease such as rheumatism is the cause of the joint inflammation, there should be rapid improvement with appropriate therapy. However, relapses of the disease with new joint inflammation are typical.
Find out all about the topic here: Synovitis.
What is chronic synovitis in the knee?
Chronic synovitis in the knee is a long-term, recurring inflammation of the synovial membrane. It is typical in rheumatological diseases and in the case of incorrect workload on the knee. Due to the frequent inflammation, the individual structures of the knee change. This can lead to limited mobility and persistent pain due to wear and tear of the joint.
The treatment of chronic synovitis is difficult. Radiological therapy methods such as radiosynoviorthesis can be helpful here. If the joint is severely damaged, the use of an artificial joint may be necessary.
What is pigmented villonodular synovitis in the knee?
Pigmented villonodular synovitis is a rare disease that mainly affects patients between the ages of 30 and 40. It is a benign, excessive increase in the synovium and synovial fluid, the cause of which has not yet been clarified. The knee and hip joints are mainly affected. The disease manifests itself as severe swelling of the knee joint, which severely restricts mobility and can be very painful.
Pigmented villonodular synovitis also shows discoloration of the skin that resembles bruises. The diagnosis is usually made by an MRI of the knee joint. A joint puncture may also be necessary. The entire synovial membrane of the affected joint is removed therapeutically.
For more information, read on: Villonodular synovitis.