Vasculitis
introduction
Vasculitis is the inflammation of blood vessels. This can affect all blood vessels in the body. Arteries, veins and the very small capillaries.
The term vasculitis is a generic term and includes various diseases that can take different courses, but all belong to the autoimmune diseases. In the case of an autoimmune disease, the body itself forms antibodies against the body's own structures and thus destroys them.
There are two forms of vasculitis, primary and secondary.
Primary vasculitis is an independent disease that can be traced back to autoimmunological processes. Secondary vasculitis is caused by the use of medication, infections, or certain autoimmune diseases.
causes
A Vasculitis can through various causes be evoked. However, every vascular inflammation is one Immune system reaction.
The primary vasculitis is independent Autoimmune diseasewhich is inflammatory-rheumatic. However, the exact causes for this are unclear.
The secondary vasculitis are triggered by other factors. Underlying autoimmune diseases can lead to vascular inflammation. These include, for example Rheumatoid arthritis, Crohn's disease and systemic Lupus erythematosus.
Also Infections in the body Viruses or bacteria can be the cause of vasculitis. Streptococcal infections, hepatitis, HIV or borreliosis are possible triggers.
Malignant tumors can also cause vasculitis.
In addition, the Taking certain medications have inflammation of the vessels as a possible side effect. This can be for example Antibiotics, Cytostatics and so-called ACE inhibitors be the case.
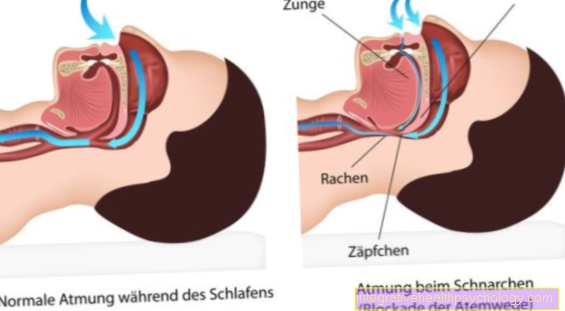
Body's own antibodies can be along with drugs, viruses or bacteria Complexes build up in the walls of the blood vessels. This leads to damage to the vessel walls and, as a result, inflammation. As an inflammatory reaction, the walls swell and narrow the blood vessels. This obstructs the blood flow.
Symptoms
The inflammation of the blood vessel walls and the resulting narrowing lead to impaired blood flow in the body. Usually it is arterial vessels that are affected by vasculitis. The organs that lie behind the affected vessels are then poorly supplied with blood. This means that the oxygen and nutrient supply is also reduced. The symptoms vary depending on which vessels are affected.
In most cases, however, vasculitis is initially noticeable through general symptoms such as fatigue, fever, weight loss and often night sweats. Many patients also report joint pain.
The further symptoms depend on which organs are damaged by the vascular inflammation. The skin is often affected, or at least also affected. This is noticeable through redness and sometimes also through open areas.
Eye involvement can show up as visual disturbances and redness. If the heart is insufficiently supplied, this manifests itself in chest pain and possibly in inflammation of the heart muscle or pericardium.
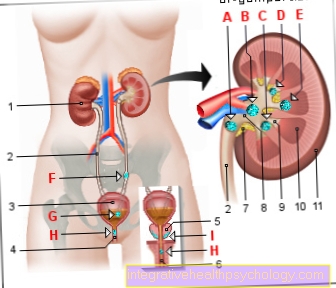
Difficulty breathing and coughing up blood indicate lung involvement, while high blood pressure and blood in the urine indicate kidney damage. If the nervous system is affected, seizures, strokes, headaches or paralysis can occur.
There are different forms of vasculitis and, depending on which form it is, certain organ systems are predominantly affected.
Find out more about the topic here: Symptoms of vasculitis
Skin vasculitis
Skin vasculitis (cutaneous vasculitis) is when the blood vessels in the skin become inflamed. In this case, the small blood vessels in particular show deposits in the vessel walls. In most cases, vasculitis of the skin vessels does not appear alone and as an independent disease, but is caused by other influences or diseases.
A common cause is the use of drugs that lead to vascular inflammation. This can be the case, for example, when taking antibiotics. Bacterial infections or vascular inflammation in other areas can also trigger cutaneous vasculitis.
The inflammation of the skin vessels is often noticeable through a rash, which can appear in various ways. Red spots, blisters, lumps or a flat rash are possible abnormalities. In addition, pain or itching may occur.
The diagnosis can be confirmed by removing tissue.
In addition, a blood test will show how far the inflammation has progressed in the body.
Depending on the underlying cause, skin vasculitis is treated in different ways. If bacterial pathogens are the cause, antibiotic therapy is initiated.
For other causes, therapy with anti-inflammatory drugs such as cortisone makes sense. In pronounced cases, immunosuppressive drugs are used.
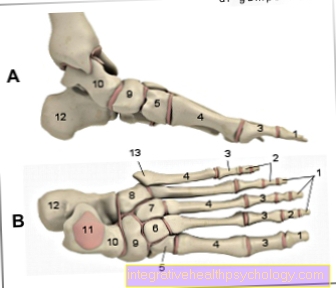
Vasculitis of the legs
Vasculitis often affects the larger and smaller vessels of the legs. The various vasculitis diseases can express themselves differently.
The purpura Schönlein Enoch is often expressed by small bleeding (petechiae) on the legs and feet. It mainly affects the small vessels. Joint problems in this area can also occur. Some patients also have edema (water retention) in the feet and legs.
Endangiitis obliterans affects the small and medium-sized vessels of the legs. Young men (under 40) are particularly affected. Heavy smokers are also more likely to be affected. The disease manifests itself primarily through pain and a feeling of coldness in the legs - especially when at rest.
Microscopic panarteritis also affects the legs. Small nodules and palpable bleeding under the skin are typical. The legs are particularly affected.
In cutaneous leukocytoclastic angiitis, the legs are also most commonly affected. Point-like redness can be observed, which does not disappear when pressed with the finger (purpura). Also, blood blisters and painful nodules may appear in the skin.
Vasculitis in the eye
If the vasculitis affects the eye, this is mainly noticeable as reddening of the affected eye. Visual disturbances can also occur. The eye is affected as part of various underlying diseases. The eye is often affected, especially when vasculitis affects smaller vessels in the body.
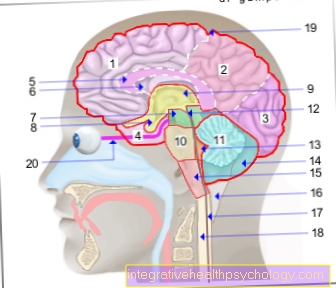
Vasculitis in the brain
If you have vasculitis in the brain, the vessels in the brain and spinal cord can become inflamed. In the brain, too, a distinction is made between primary and secondary vasculitis.
Symptomatic of vasculitis in the brain can be expressed by many different symptoms that affect the central nervous system (CNS). The common occurrence of central symptoms and other physical side effects is typical of this disease.
Often headaches, confusion or paralysis that occur on one side are included. Since a vascular inflammation, just like a stroke, leads to an insufficient supply of certain areas in the brain, the symptoms of the two diseases are similar.
The exact diagnosis of brain vasculitis is difficult because the symptoms are very unspecific. They can also resemble those of a brain tumor, meningitis, or damage to the spinal cord.
In order to make the diagnosis, brain fluid (liquor diagnostics) is usually taken. Here, increased inflammation values indicate the presence of a vascular inflammation and other diseases of the brain can be excluded.
Inflammation can be detected using MRI images of the head. To confirm the diagnosis, it may be necessary to take samples of the brain or meninges (biopsy) so that an infection by bacteria or viruses can be excluded.
Vasculitis of the brain is treated just like other inflammation of the blood vessels by the administration of anti-inflammatory or, in more severe cases, immunosuppressive drugs.
What is vasculitic polyneuropathy?
In the context of vasculitis, an inflammatory change in the vessels can damage the surrounding nerves. This can lead to discomfort, tingling and pain. The sensation of touch and temperature can also be changed. Existing vasculitic neuropathy often improves only moderately with therapy for vasculitis.
What is the classification?
The vasculitis are divided into primary and secondary vasculitis. The primary vasculitis often occurs spontaneously and has an unknown cause. They are further subdivided into vasculitis of the large, medium and small vessels.
There are also secondary vasculitis. They occur as part of another disease called autoimmune diseases, infections, or tumors. They can also be caused by certain medications.
Purpura Schönlein Enoch
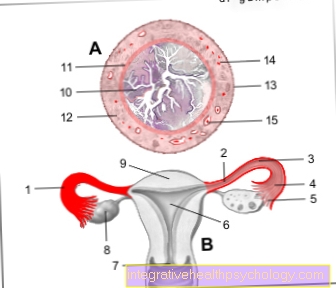
Henoch Schönlein purpura is one of the vasculitides. It is characterized by inflammation of the small vessels. This is mainly characterized by small bleeding into the skin and mucous membranes (so-called petechiae). In addition, there may be cramp-like (colicky) abdominal pain and painful swollen joints. If the kidneys and gastrointestinal tract are affected, blood may appear in the urine or stool. Antibodies (proteins that are formed by the body against foreign substances) are deposited on the vessel walls of the small vessels. The immune system then reacts with inflammation of the vascular wall. This destroys the vessel wall and the blood can escape into the surrounding connective tissue. This leads to the small bleeding (petechiae) in the skin.
The Purpura Schönlein Henoch occurs mainly in small children and school children. An accumulation in the winter months can also be observed. The exact cause is still unknown. An increased occurrence a few weeks after a viral or bacterial infection is noticeable. It can also be triggered by medication. The disease is not contagious and usually heals on its own. It mainly treats symptoms such as fever and pain. Physical exertion should be avoided. Cortisone can be administered to slow the inflammation. Overall, the disease can last four to six weeks.
Read more on the subject at: Purpura Schönlein Enoch
Behcet's disease
Behcet's disease is a very rare disease that belongs to the group of vasculitides. The disease occurs more frequently in the Mediterranean region and Asia. It also occurs in families and is associated with the antigen HLA-B51. The cause is still unknown. It is discussed that viral infections are possible triggers.
It is characterized by inflammation of the small vessels. The eyes, skin and mucous membranes are particularly affected. Characteristic symptoms are canker sores (defective areas of the mucous membrane) in the mouth and genital area as well as inflammation of the middle skin of the eye (uveitis). A high level of inflammation is often seen in blood tests. Above all, the general symptoms are treated. In addition, glucocorticoids (cortisone) and immunomodulators can be used, both of which have an immunosuppressive effect. This reduces the function of the immune system.
Read more on the subject at: Behcet's disease
Takayasu vasculitis
Takayasu vasculitis is a special type of vasculitis. It manifests as inflammation of the abdominal artery (aorta) and its main branches (for example the kidney arteries). There may also be general symptoms such as fever, night sweats, malaise or weight loss. The narrowing of the lumen of the abdominal artery can lead to a weakened pulse, a difference in blood pressure between the arms and legs, heart attacks and cerebral infarctions.
Takayasu vasculitis is a very rare disease. The cause is so far unknown. It occurs mainly in young women under 40 years of age. The disease is treated with drugs that reduce the function of the immune system, such as cortisone and aspirin.
What is the connection between vasculitis and collagenosis?
Collagenosis is a disease of the connective tissue, while vasculitis is primarily a disease of blood vessels. A collagenosis manifests itself mainly as a fever and a deterioration in the general condition. It can also lead to dryness of the eyes and mouth. Small bleeding into the skin (petechiae) is also possible. A collagenosis can therefore be very similar to a vasculitis or a vasculitis can also occur in the context of a collagenosis.
Diagnosis
If vasculitis is suspected, blood is drawn first. Increased levels of inflammation, how CRP or the white blood cells, are evidence of inflammation in the body. Some forms of vasculitis are specific antibody increased in blood.
But imaging tests can also be helpful in making the diagnosis. These include Ultrasound examinations or the special vascular presentation through the use of contrast media in the Computed Tomography (CT) or Magnetic resonance imaging (MRI). An X-ray examination with a contrast agent can also show the vessels.
To confirm the suspicion, a Tissue sample taken and examined (biopsy). This can be taken from various organs or vessels. Often, however, this is not possible due to the high risk.
What do you see in an MRI?
The advantage of an MRI (magnetic resonance tomography) is to be able to assess the vessel walls well. The inflammatory processes that occur in vasculitis can thicken the vessel walls. This can be shown well in the MRI.
therapy
There are various treatment options vasculitis. Which one is chosen depends on the type of vascular inflammation and which organs are affected to what extent.
Usually, drugs that have anti-inflammatory effects are used for vasculitis. This includes, for example Cortisone, which can be used as a cream for external use or as tablets for systemic therapy.
In some cases, especially if the kidneys are severely affected, it is necessary to suppress the body's immune system. For this purpose, special drugs, the so-called Immunosuppressants, applied.
Also one Combination of different active ingredients is possible. Often there is vasculitis not curable, through drug therapy, the Course however positive influenced and the symptoms can be reduced.
After having gone through and healed vasculitis, the risk of developing one again is quite high. It is therefore very important to pay attention to early signals from the body and to consult a doctor immediately if the feeling of weakness, fever, night sweats or weight loss persists.
Which doctor treats vasculitis?
If you suspect vasculitis or if you have been suffering from vasculitis for a long time, the first point of contact should be your family doctor. He can write a referral to a specialist. An emergency presentation can of course take place at any time in the hospital or with a medical on-call service.
Doctors in internal medicine (internists) and above all rheumatologists specialize in vasculitis. If vasculitis has been diagnosed, you should present yourself regularly in order to be able to optimally coordinate the therapy.
Can Vasculitis Be Cured?
There is often no cure for vasculitis. As a result of the advances in therapy options, vasculitis is now mostly very treatable. However, this often means that very aggressive immunotherapy with cortisone and immunosuppressants (which reduce the function of the immune system) must be carried out. If the therapy works well and the vasculitis improves, the therapy can often be reduced in consultation with the attending physician, so that high doses often only have to be taken for a short time.
What is the life expectancy with vasculitis?
The life expectancy with vasculitis is not significantly reduced by the innovations in therapy (immunomodulators) than with a healthy person. The immunomodulative therapy reduces the function of the immune system and reduces inflammatory reactions. Early detection of the disease and appropriate therapy are important. With early detection and promptly initiated therapy, serious consequential damage can also be reduced. It is also important to lead a healthy lifestyle. This includes sufficient exercise, a healthy diet and abstaining from nicotine.

.jpg)