Diving disease
Synonyms
Diving sickness, decompression sickness or decompression sickness, caisson sickness (caisson)
introduction

Decompression sickness occurs most often in diving accidents and is therefore also referred to as diving disease. The real problem with decompression sickness is that If the surface is too rapid, gas bubbles form inside the body and these then trigger the typical symptoms. Decompression sickness is classified according to the severity of the symptoms three types assigned.
Definition
There are some inconsistencies in terms of terminology. In English, decompression sickness is known as decompression sickness (DCS) or as decompression illness designated. In German there is no difference between "sickness" and "illness". Many diving doctors don't accept this difference either. Another problem with the naming, to make the confusion completely, is that the decompression sickness also started with DCI (decompression incident) is abbreviated.
Under the umbrella term decompression sickness, two different approaches to the formation of gas bubbles inside the body are summarized. On the one hand, gas bubbles can form too much nitrogen in the blood or in tissue (DCS). It can also be another gas, like Helium or hydrogen. On the other hand, it can be too high if the pressure is too high Tears in the central pulmonary vessels come and thereby lead to the formation of Air bubbles in the blood vessels (arterial gas bubble embolism, AEG).
root cause
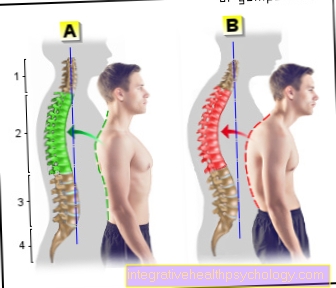
The solubility of a gas in a liquid depends on the Ambient pressure (Henry Law). For example if you click 30m depth dives, then the partial pressure of the gas increases and thus more gas dissolves in the blood. Say it is more dissolved nitrogen in the blood. The blood now transports the nitrogen to the tissue, where more nitrogen is now also accumulating due to the shifted pressure conditions (Saturation of the tissue). The different tissues take up nitrogen at different rates, depending on the blood flow rate. The more blood is supplied to a tissue (e.g. brain), the faster it takes up the nitrogen, i.e. H. the saturation of the tissue occurs more quickly than, for example, in cartilage or bones with little blood supply. The Desaturation on ascent, d. H. the tissue releases the nitrogen back into the blood and it is exhaled through the lungs, also different from tissue to tissue. While the brain desaturates quickly, the bones or cartilage take a long time. So when climbing you have to do the Observe decompression rulesOtherwise, if the ascent is too rapid, the external pressure drops faster than the tissues can desaturate. The previously dissolved nitrogen and other gases no longer remain in solution and form in the blood and tissue fluid Gas bubbles out. This process can be compared to the frothing of a soda bottle the first time it is opened. The gas bubbles that have now formed can now close in the tissue mechanical injuries lead and Clog blood vessels similar to a thrombus (Gas embolism).
The The risk of decompression sickness increases at high altitudes (Mountain lake diving), as the atmospheric pressure is already lower here and the gases remain in solution even worse.
The Caisson disease is after the Caissons which were used to make foundations for bridge piers. In contrast to the diving bells previously used, the caissons made it possible to work longer. With the introduction of caissons, the number of decompression sickness also increased.
Astronauts are also at increased risk to suffer decompression sickness while exiting space. In order to minimize the risk, the astronauts have to spend the night before the space exit in a chamber where the pressure is significantly lower so that they can get used to the low pressure conditions.
First aid
If there is a suspicion of a diving accident, the following measures must be taken, as these can save lives:
In the first place comes the Alerting the rescue workers. If there is a chance, it should be given to the patient give pure oxygen. When unconscious the patient in a Shock positioning (as you know from the driver's license course) and check your breathing and pulse. If you stop breathing or your pulse stops, perform cardiopulmonary resuscitation. During the whole procedure make sure that the Patient is kept warm with blankets. If the patient is conscious, do not perform a shock position as this will cause the Intracranial pressure can increase, but stable side position or prefer to lie on your back. The rescue workers should initiate infusion therapy with 500ml - 1000ml liquid and a pressure chamber treatment with hyperbaric oxygen.
Type I decompression sickness
With decompression sickness type I (DCS I) are mainly tissues that have less blood flow are affected, such as skin, muscles, bones and joints. The symptoms show up in 70% of the cases in the first hour after the dive. However, cases have also been described in which the symptoms of DCS I still occurred after 24 hours. Show on the skin blue-red discoloration with a swelling and strong Itching (diving fleas) caused by the blockage of small blood and lymph vessels. In the muscles, the bubbles cause one pulling pain and a Pressure sensitivity. This lasts for a few hours and then turns into symptoms of sore muscles. In the bones, joints and ligaments, pain and restricted mobility come to the fore. The knee joint is most commonly affected. The pain in the joints is called "bends " designated. This comes from caisson workers who suffered from the occupational disease caisson disease and had a stooped posture (English "to bend" = "to bend").
With the DCS I one is enough pure oxygen treatment to make the symptoms go away. Since the DCS I is often the forerunner of the dangerous DCS II, it should still be treated in the pressure chamber.
Type II decompression sickness
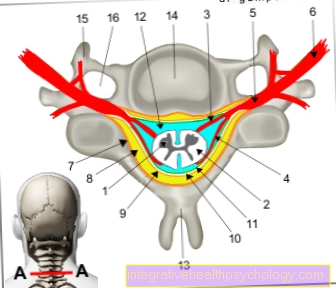
DCS II affects the brain, spinal cord, and inner ear. Here, the direct gas bubble formation in the tissue itself is less the cause of the damage than the cause Gas embolismwhich lead to occlusions of the small vessels. The damage to the brain can cause very different symptoms depending on where the occlusion occurs. It can too Clouding of consciousness up to Unconsciousness with respiratory paralysis come. It can too Paralysis of the arms or legs come or completely to hemiplegia. Bilateral paralysis occurs in the spinal cord, Sensory disturbances or Urinary and rectal disorders. The occlusions in the spinal cord appear a little later than those in the brain. The symptoms can also worsen over time (initially only a discomfort in the big toe, leading to paralysis). If embolism disturbs the blood circulation in the inner ear, it leads to nausea with vomiting, dizziness and Ringing in the ears.
Type III decompression sickness
Under the DCS III, the Long-term damage classified.The recognized occupational diseases of divers include aseptic bone necrosis (AON, a tissue destruction of the bone that was not caused by an infection), Hearing impairment, Retinal damage and neurological failures after an unresolved DCS II.
Pulmonary overpressure accident AGE (arterial gas embolism)
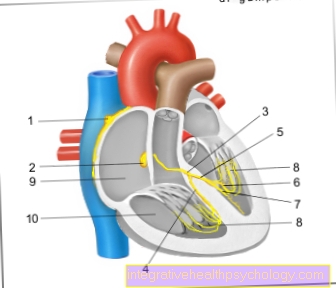
If the pressure is too high, the alveoli tear and the air gains connection to the blood vessel, causing the alveoli to form in the blood vessels and clog the arteries like a thrombus. The symptoms are similar to DCS II. In addition, a heart attack can occur here due to the occlusion of the coronary arteries.
You might also be interested in this topic: Air embolism
Prevention and Risk Factors
For each dive the appropriate Ascent rates and the Decompression rules be respected. This will minimize the risk of decompression sickness. With certain risk factors, however, despite adhering to the decompression rules, a decompression sickness can occur.
People who have the following risk factors are particularly at risk.
High age
Upper respiratory tract infection
High blood pressure (hypertension)
fever
diabetes
People who are almost dehydrated (dehydrated) due to insufficient fluid intake or excessive fluid loss (severe diarrhea)
alcohol
Heavy smokers
Obesity
stress
fatigue
aching
history
Of the Relationship between pressure and the solubility of gases in liquids was established in 1670 by Robert Boyle. However, it was not until 1857 that the theory of gas embolism as the cause of decompression sickness was established by Felix Hoppe-Seyler. There were then further investigations into diving depth and diving time. However, it wasn't until 1878 that Paul Bert's first textbook for divers came out and the recommendation that a decompression time of 20 minutes should be observed for each bar of pressure relief. This recommendation was valid for the next 30 years. Through experiments on sheep, John Scott-Haldane discovered that there are different tissues that saturate and desaturate at different rates. He was the first to bring out decompression tables for the different tissue classes. However, his tables only went to a depth of 58m. These tables formed the basis for research for the next 25 years. Haldane had taken a very simple model as the basis for his tables. He assumed that the degree of saturation or desaturation only depends on the blood flow. In the following years, research was carried out to refine the whole and calculate it for greater depths. In 1958 the most popular tables were those of the US Navy. They were based on 6 tissue classes and variable supersaturation factors.
The dive tables were finally replaced by dive computers, which could record the processes during diving in a much more complex way. But even computers cannot rule out all risks, as they cannot capture all of the complex processes in the body. Studies are still ongoing to better control microbubble formation.