Tear duct stenosis
definition
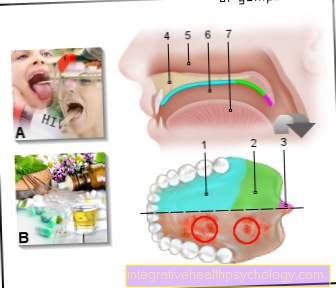
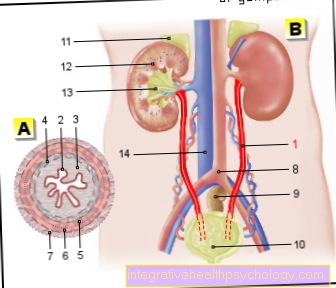
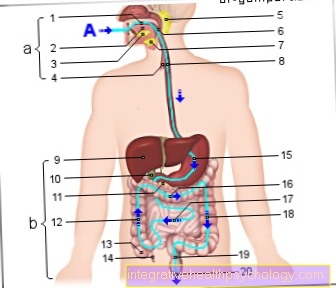
In the case of tear duct stenosis, the tear duct becomes blocked for various reasons, which hinders the outflow of tear fluid. The tear fluid is formed in the lacrimal gland, which is located at the top outside of the eye.
From here the tear fluid reaches the surface of the eye, where it protects the eye from dehydration and the penetration of pathogens. With the help of the blink of an eye, the tear fluid is transported over the entire surface of the eye to the inner corner of the eyelid.
Then the tear fluid is usually drained through the lacrimal dots, tubules, the tear sac and finally through the tear and nasal duct into the nose. With tear duct stenosis, this drainage is disturbed and tear fluid collects in the eye, causing the eye to water constantly. On the one hand, this can be perceived as very annoying, on the other hand, the build-up of the tear fluid can cause infections of the eye with bacteria, which is why a persistent tear duct stenosis should always be treated.

How common is lacrimal stenosis?
Lacrimal stenosis is a common condition. Congenital lacrimal stenosis affects around 30 percent of newborns. In the majority of the affected newborns, however, this regresses quickly. The frequency of acquired tear duct stenosis increases with age and affects every third person from the age of 90.
Recognizing tear duct stenosis
What are the symptoms of lacrimal stenosis?
With tear duct stenosis, there is a disruption in the tear fluid drainage system. This leads to constant tears and the formation of a lake of tears in the affected eye.
If too much tear fluid accumulates, tear fluid overflows over the edge of the eyelid, which is referred to as "teardrop" or "epiphora".
Since the tear fluid also comes to a standstill in the tear sack because it cannot flow out through the tear duct and the nasal passage, the tear sack can become infected with bacteria. Symptoms such as the discharge of purulent secretions when pressure is applied to the inner corner of the eyelid, as well as reddening and swelling of the inner corner of the eyelid, are common.
Purulent crusts can also form on the corner of the eyelid. As a complication, the inflammation can spread to the surrounding soft tissues, which is then known as phlegmon.
How is lacrimal stenosis diagnosed?
Typical symptoms of patients with lacrimal duct stenosis are tears (Epiphora) and constant tearing of the affected eye. However, these symptoms can also occur with other diseases of the eye, which must be ruled out before a lacrimal stenosis is diagnosed.
In order to diagnose lacrimal stenosis, it is important to carefully question the patient about his or her symptoms (anamnese), as well as an ophthalmological examination of the eye, which includes a close look at the lids, teardrop points and conjunctiva of the affected eye.
In some cases, for example for the precise localization of the lacrimal duct stenosis, imaging methods such as ultrasound, X-rays, computed tomography (CT) or magnetic resonance imaging (MRI) used to depict the draining tear ducts.
In the case of acquired tear duct stenosis, an additional examination by the ear, nose and throat doctor may be necessary if the cause of the tear duct stenosis is suspected to be polyps, tumors or a misalignment of the nasal septum. This is usually done as part of an endoscopy, in which the structures in the nose that may hinder the drainage of the tear fluid can be shown very well.
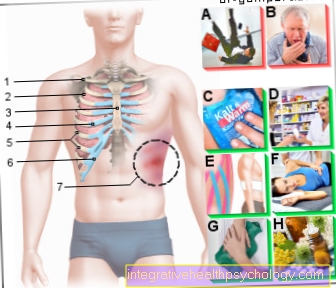
Treat tear duct stenosis
How is lacrimal stenosis treated?
Various measures can be considered for the treatment of tear duct stenosis.
In the case of congenital lacrimal stenosis, the Hasner membrane often regresses spontaneously within the first year of life and thus improves the outflow of tear fluid, which is why a wait-and-see approach is justified.
The opening of the tear and nasal duct can be encouraged by daily massages of the tear and nasal duct with the index finger. The use of decongestant eye drops and nasal drops can also improve the outflow of tears. Antibiotic eye drops are used to treat infections of the eye. It should be noted that the use of eye drops and nasal drops is by no means suitable for long-term therapy.
Instead, if there is no improvement in the symptoms after the sixth month of life, other procedures such as positive pressure irrigation or probing of the draining tear ducts should be carried out.
If the nasal tear duct cannot be opened in this way, various surgical measures are available to enable the proper drainage of tear fluid. If complaints such as tears or infections increase in frequency, the measures mentioned such as pressurized irrigation, probing and surgery are recommended before the age of six months.
In the case of acquired tear duct stenosis, different treatment options can also be used, depending on the cause. These include, among other things, the removal of nasal polyps and tumors or a correction of a misalignment of the nasal septum.
Prevent tear duct stenosis
What are the causes of lacrimal stenosis?
Lacrimal stenosis can be congenital or acquired. Congenital lacrimal stenosis is a disorder of the regression of tissue at the junction of the lacrimal duct and the nose. Normally, the tissue present here regresses before the child is born, but in some cases this regression does not take place, or not properly.
This tissue, which is a barrier for the tear fluid, is called Hasner's membrane.
Due to the presence of a Hasner membrane, the tear fluid cannot drain and the affected newborns become conspicuous with constant eye tears. However, tear duct stenosis can only occur at an advanced age.
Reasons for an acquired, i.e. not congenital, tear duct stenosis are, for example, injuries in the area of the draining lacrimal ducts, such as the lacrimal tubules or the tear duct, which impair the drainage of the tear fluid. This can include bite wounds or cuts.
Previous inflammation of the draining tear ducts can also be the cause of acquired tear duct stenosis. But not only diseases of the tear duct itself, but also diseases of the nose such as polyps, tumors, a misalignment of the nasal septum or swelling of the nasal mucosa caused by runny nose can obstruct the tear-nasal duct and thus also cause an impaired drainage of tear fluid.
How can you prevent tear duct stenosis?
In many cases, tear duct stenosis cannot be prevented.
Acquired tear duct stenosis can be prevented by avoiding injuries and frequent inflammation of the tear ducts or, if necessary, by removing polyps and tumors in the nose. In the case of congenital lacrimal stenosis, on the other hand, rapid treatment is particularly important in order to prevent complications such as infections of the eye.
Course of tear duct stenosis
What is the prognosis for lacrimal stenosis?
With congenital lacrimal stenosis, the prognosis is good.
A healing through the spontaneous regression of the Hasner membrane within the first year of life is common. The healing process can be promoted by various measures, such as massages or probing the tear duct. The prognosis of acquired lacrimal stenosis depends on the cause of the obstruction.
Further questions about tear duct stenosis
How do you recognize lacrimal stenosis in newborns?
Symptoms / complaints
The closure of the tear and nasal duct not only builds up mucus but also the tear fluid, which normally flows from the eye through the tear and nasal duct into the nose. This leads to the symptoms typical of lacrimal duct stenosis, such as constant tearing of the eye and the tear fluid overflowing over the edge of the eyelid, which is referred to as tears or epiphora.
diagnosis
The diagnosis of lacrimal duct stenosis in newborns is usually made on the basis of typical clinical complaints, such as constant tears and tears in the affected eye. In some cases, additional examinations with imaging methods such as ultrasound, X-rays, computed tomography (CT) or magnetic resonance imaging (MRI) are necessary to diagnose the tear duct stenosis.
therapy
If the irrigation and the probing of the tear ducts are also unsuccessful, various surgical measures are available to establish the proper drainage of tear fluid.
How do you recognize lacrimal stenosis in adults?
A narrowing of the tear ducts, a tear duct stenosis can also occur in adulthood. However, lacrimal duct stenosis in adults has different causes than lacrimal duct stenosis in the newborn.
root cause
Injuries or previous inflammations in the area of the lacrimal ducts are often the cause of lacrimal duct stenosis in adulthood. But diseases of the nose such as polyps, tumors, a misalignment of the nasal septum or swelling of the nasal mucous membrane caused by a cold can obstruct the tear-nasal duct and thus hinder the drainage of the tear fluid.
Symptoms
In the case of tear duct stenosis, there is an impairment of the drainage of the tear fluid, which leads to constant tears in the affected eye and to tear fluid overflowing over the edge of the eyelid (tears or epiphora). Tears can also come to a standstill in the eye sac due to the obstructed drainage, which can lead to an infection of the eye sac with bacteria. In the context of an inflammation of the tear ducts, symptoms such as discharge of purulent secretion when pressure is applied to the inner corner of the eyelid, as well as reddening and swelling of the inner corner of the eyelid, are added.
diagnosis
The diagnosis is made on the basis of the typical symptoms. If necessary, examinations with imaging methods such as ultrasound, X-ray, computed tomography (CT), magnetic resonance tomography (MRT) or an endoscopy of the nose are necessary to diagnose lacrimal duct stenosis or its causes.
therapy
For the treatment of lacrimal duct stenosis in adults, as with lacrimal duct stenosis in newborns, irrigation and probing of the lacrimal ducts as well as various surgical measures can be considered. In addition, depending on the cause of the tear duct stenosis, it may be necessary to remove nasal polyps and tumors or to correct a misalignment of the nasal septum.















.jpg)