Varicella zoster virus (VZV)
definition
The varicella zoster virus (VZV), which also belongs to the herpes virus group, causes various neurological diseases. The following are to be mentioned here:
- chickenpox
- Herpes zoster encephalitis (inflammation of the brain)
- Herpes zoster myelitis (inflammation of the spinal cord)
- Zoster radiculitis / neuritis (inflammation of a nerve root / nerve, commonly known as shingles)
- Zoster vasculitis (inflammation of blood vessels)
Zoster encephalitis is rare and its clinical appearance can hardly be distinguished from herpes simplex encephalitis. The therapy is also high-dose with acyclovir, the prognosis is accordingly.
You may also be interested in this topic: Viral infection
.jpg)
What is the varicella zoster virus?
The varicella zoster virus is a primarily neurotropic virus that remains in the sensitive ganglia (accumulation of nerve cell bodies, "node" in the CNS) of the central nervous system for life after the initial infection, which manifests itself as chickenpox (varicella).
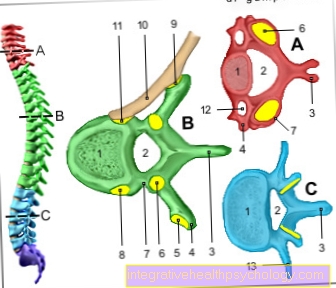
These are called the spinal ganglia on the torso, and the ganglia on the head have proper names.
Here the virus behaves quietly until it is under certain conditions reactivated becomes. A weakening of the immune system is the most important of these conditions, but stress, infectious diseases or surgical interventions (surgery) can also lead to it.
The reactivated virus then migrates from the sensitive ganglion along the nerve to which this “node” belongs, into the skin. Since this nerve is a sensitive nerve, that is, it is responsible for feelings in the skin, it normally conducts pain that is caused in the skin by damage to the brain.
If the varicella zoster virus now wanders along the nerves and the body's own cells try to fight it at the same time, the nerve is irritated. This results in (dull or pulling) pain and sensory disturbances in the supply area of this nerve, i.e. in a specific skin area without this being damaged.
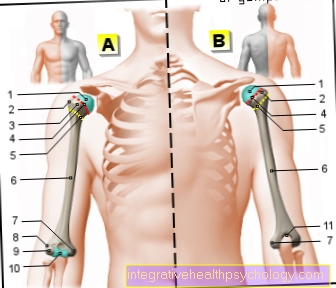
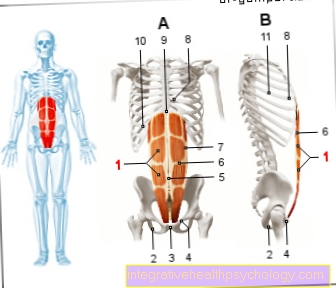
The affected skin area is called a segment or dermatome. The whole body is divided into such segments or dermatomes, symmetrically on both halves of the body. The varicella zoster virus (VZV) usually affects only one side and only one dermatome.
If several dermatomes are affected or both halves of the body (or halves of the face), the underlying condition may be more serious, e.g. AIDS or cancer.
You can find out more about this under our topics: AIDS, cancer
How does the varicella zoster virus express itself?
The most common zoster attacks:
- Segments in the chest / stomach area (thoracic segments) Here the disease is referred to as shingles; because the segments are arranged in a belt shape here
- Segments of the lower neck area (cervical segments); Pain in the shoulder and arm area
- The uppermost of three segments of the sensitive facial nerve (trigeminal nerve), zoster ophthalmicus (pain in the eye and forehead region) (Greek: ophthalm = eye). The nose and chin regions (2nd and 3rd trigeminal branches) are less affected.
- The segment that supplies the ear region Zoster oticus (pain in the ear, lateral face / neck)
On the 3rd - 5th day, vesicles arranged in groups appear in the affected skin area, which can be bloody, filled with secretion and virus and scabbed off after a few days. Like the vesicles in chickenpox, they can leave small scars.
In zoster ophthalmicus, the whole eye with the cornea and the optic nerve is affected, which can lead to permanent damage and even blindness.
In zoster oticus, the whole ear with the auricle and inner ear. Since the organ of equilibrium is also located in the inner ear, there can be impressive symptoms with ringing in the ears, vertigo and nausea.
The involvement of various cranial nerves is possible, especially the facial nerve, which supplies the facial motor muscles. In 60% of the cases, there is therefore unilateral facial paralysis (facial paralysis).
Read more on the topic:
- Shingles of the eye
- Facial palsy
Varicella zoster virus and shingles - what is the connection?
The causative agent of shingles is the varicella zoster virus (VZV). It belongs to the herpes virus family. It can be transmitted through the air (droplet infection), but also through contact with the virus-containing vesicle contents or crusts (smear infection).
When infected with the varicella zoster virus for the first time, the disease manifests itself as chickenpox. Chickenpox often occurs in childhood. This results in small, mostly raised, round-oval, red spots and blisters in the area of the trunk, face, arms and legs and accompanying headache and body aches and fever. After healing, a renewed outbreak (reactivation) of the virus and the clinical picture of shingles can occur many years later. This reactivation is favored by a weakened immune system (e.g. in the event of stress, infections, tumor diseases, immunosuppressive therapy). The viruses spread along the nerve fibers into the skin. There it comes to a striped rash with the formation of secretion-containing blisters. At the same time, the patient reports severe pain in the affected area.
Read more on the subject at: Shingles
diagnosis
In addition to the clinical appearance with the pioneering skin changes, a lumbar puncture with examination of the nerve fluid is also performed here to confirm the diagnosis, although this is often not necessary at all.
There are 20 - 70 cells (lymphocytes = white blood cells) and normal protein levels. Both increase when extensive inflammation of the meninges (zoster meningitis) develops with a high fever, clouding of consciousness and stiff neck.
The PCR test proves the VZV genetic material. The PCR can be used to detect DNA substance of the varicella zoster virus in the nerve water (CSF -> CSF diagnostics), which is evidence of an infection.
You can find further information on the examination of the nerve fluid (liquor diagnostics) under our topic: CSF diagnostics
Laboratory value "IgG"
Immunoglobulins G (IgG) are part of the specific immune system and are released by plasma cells (B lymphocytes). They are used to fight viruses and bacteria. In the case of an initial infection, IgG antibodies are only formed and released with a delay. They therefore often show that an infection has already subsided.
In the case of reinfection, however, they are released after 24 to 48 hours. For this reason, IgG antibodies play an important role in the diagnosis of shingles.
Laboratory value "IgM"
Immunoglobulins M (IgM) are also part of the specific immune system and are released by plasma cells (B lymphocytes). They are used to fight viruses and bacteria. They are formed and released directly during the initial infection and represent the first defense reaction to invading pathogens.
After the acute phase of an infection has subsided, the concentration of IgM antibodies in the blood decreases rapidly. For this reason, the IgM antibodies are primarily used to identify acute infections. If the varicella zoster virus reactivates in the course of shingles, an increase in IgM may not occur at all.
What does it mean when the antibodies (AK) are too high?
In the case of an infection with varicella-zoster viruses, the clinical picture of chickenpox occurs during the initial infection. After healing, the viruses remain in the human body and can be reactivated if the immune system is weakened. The appearance of shingles emerges as it spreads along the nerves.
The analysis of immunoglobulins (= antibodies) plays an important role, especially in diagnosing shingles. The immunoglobulins G in particular are assessed here. An increase in IgG antibodies suggests renewed infection with the varicella zoster virus and thus the presence of shingles. An eight to fourteen day follow-up of the IgG level is recommended in order to be able to assess the disease activity. IgM antibodies only play a subordinate role in the diagnosis of shingles.
The immunoglobulins M can be measured to diagnose chickenpox. These are particularly high in the acute phase of the infection. As the symptoms subside, increased IgG levels in the blood can occur. The analysis of immunoglobulins, however, only plays a subordinate role in chickenpox.
General information can be found at: antibody
therapy
Herpes zoster can be treated with antivirals. Virus statics are substances that can inhibit the replication of viruses. They are comparable to antibiotics, which prevent bacteria from multiplying.
The following are used, among others:
- Acyclovir (intravenous or tablets, 5x / day 800 mg)
- Valaciclovir (tablets 3x / day 1 g for 7 days),
- Famciclovir (tablets, 3x / day 250 mg) or
- Brivudine (Zostex® tablets 1x / day 125 mg)
As things stand, brivudine has proven to be the most effective drug.
Therapy should be started as early as possible (within the first 72 hours) to avoid complications.
Particular mention should be made here of the nerve pain that occurs more frequently with increasing age and that can manifest itself in the affected skin area after shingles (post-therapeutic zoster neuralgia).
Pain therapy initiated in good time also helps to prevent this postherpetic neuralgia.
The administration of corticosteroids (30-60 mg prednisone equivalent) has long been controversial because it additionally weakens the patient's own immune defense, but is also said to have a preventive effect against postherpetic neuralgia by suppressing the development of vascular inflammation.
With zoster ophthalmicus it makes sense to give acyclovir eye ointment to avoid permanent damage to the cornea (scar tissue).
If the vesicles on the skin become infected with bacteria (superinfection), they are treated with ointments containing antibiotics.
complication
Complications of a herpes zoster infection:
- Postherpetic zoster neuralgia (postherpetic neuralgia). In this case, there is the most severe burning, permanent pain (neuralgic pain) in the affected segment, although the infection has long been defeated. This is permanent damage to the nerve from the past infection.
Neuralgic pain is extremely difficult to get under control, since conventional painkillers are ineffective. You treat with a combination of painkillers, one tricyclic antidepressant and the anti-epileptic Carbamazepine (see also Trigeminal neuralgia) - Polyneuropathies
- Guillain-Barré Syndrome
Further information on this topic can be found at:
Guillain-Barré Syndrome - Incomplete resolution of paralysis, especially of the face (Facial palsy)
- Spread of the zoster over the whole body and internal organs (zoster generalisatus).
This serious clinical picture is life-threatening and is more likely to be found in patients with a weakened immune system (e.g. in AIDS, Cancer, immunosuppressive drugs such as corticoids (cortisone) or chemotherapy)
In younger patients, the herpes zoster usually heals without consequences.























.jpg)

