Atrial flutter
introduction
Atrial flutter is when the atria of the heart contract significantly faster than the ventricles for a limited time or permanently.
Normally, the atria and the ventricles form a coordinated unit. Blood travels from the circulatory system and from the lungs to the atria of the heart. The atrial cells contract after electrical excitation by the sinus node and pump the blood into the chambers. The electrical excitation is conducted from the sinus node via the atria to the AV node. This passes the excitation on to the heart cells of the chambers via paths of a transmission system. As a result of the electrical activation, the blood-filled chambers contract and pump it into the body's circulation. At the same time the atria are filling up with new blood and the electrical wave has activated the last heart cell. The heart is now ready for a new cycle that begins again with a new excitement and the filled atria.

The electrical activation of the heart cells is controlled via both the sinus node and the AV node, with the AV node passing on the rhythm of the sinus node as the first priority. If the sinus node fails, the AV node can set its own clock. This system should create and guarantee a regular rhythm that can be adapted to external requirements.
The normal rhythm of this process generates a pulse rate of 60 - 80 beats / minute at rest.
With atrial flutter, the atrial cells are activated by themselves, which is no longer caused by the sinus node. This process can be triggered by a so-called reentry mechanism. The excitation does not arise centrally at the sinus node, but in another area of the atria. This activation is also passed on to all cells of the atria. This can lead to an acceleration of the rhythm, so that the pulse rate increases to 200-350 beats / minute. In this case one speaks of a "flutter" of the atria.
Due to the nature of the AV node, this rapid frequency is in most cases not transmitted 1: 1 to the ventricles, but only every 2nd or 3rd beat. This also increases the heart rate, but not as much as in the atria. Atrial flutter is often caused by organic diseases of the heart.
What is the difference to atrial fibrillation?
Both atrial flutter and atrial fibrillation lead to a disturbed spread of excitation within the atria. Circling excitation within the atria leads to an increased contraction of the atria and, as a rule, the ventricles as well.
In contrast to atrial fibrillation, with atrial flutter, the excitation is usually transmitted regularly from the atria to the ventricles. For example, every second or third excitation is transmitted to the chambers. In atrial fibrillation, this transmission of excitation is irregular. In addition, with atrial flutter there is a clearly defined spread of the excitation, whereby the atria are excited in an orderly manner. In addition, atrial flutter shows a mostly typical ECG finding. This shows a characteristic “sawtooth pattern” instead of a straight isoelectric line.
While catheter ablation has a higher probability of success in typical atrial flutter, atrial fibrillation often shows a better response to medication.
A transition between atrial flutter and atrial fibrillation is possible.
Read more about this under
- Atrial fibrillation
- Atrial flutter and atrial fibrillation
causes
The exact origin of atrial flutter is not yet fully understood.
Atrial flutter is favored by organic heart diseases (coronary heart disease, heart valve diseases, heart muscle diseases, and many more), which lead to damage and scarring of the heart tissue. Other triggering factors can be emotional stress and excessive alcohol or nicotine abuse. In rare cases, atrial flutter occurs even in patients with healthy heart. However, older people are particularly affected.
With regard to the development of atrial flutter, a distinction is made between a typical and an atypical form. The typical (85%) is much more common than the atypical form (15%).
With typical atrial flutter, there is a delayed spread of excitation from the sinus node (located in the right atrium) via the muscles of the atria to the AV node (located at the transition between atria and ventricles). This delay occurs primarily due to scarred heart muscle tissue as a result of organic heart disease. As a result, the atria become unevenly aroused. While individual areas were already excited and can be excited again, other muscle cells have not yet been excited. This creates the risk of permanent circling excitation within the atria. This often forms around the tricuspid valve (valve between the right atrium and right ventricle). As a result, only every second or third excitation originating from the sinus node is transmitted to the chambers.
In atypical atrial flutter, the circular excitations are not located in the area of the tricuspid valve, but can be localized in the entire atrial tissue. As a result, the atypical atrial flutter is much more difficult to localize and treat.
Atypical atrial flutter
The typical atrial flutter often arises in preferred locations in the right atrium, for example in the area of scarring. In atypical atrial flutter, it can arise in both the right and left atrium. Anatomical structures or scars are preferred as the place of origin.
Concomitant symptoms
Atrial flutter is often noticeable through a rapid and possibly irregular pulse. This can also have a direct impact on the heart, as the heartbeat is perceived as fast, strenuous or irregular. In addition, circulatory weakness or restricted resilience, shortness of breath or a feeling of pressure in the chest can occur. Atrial flutter cannot be distinguished from the more familiar atrial fibrillation only on the basis of the symptoms. There is a chance that the flutter could turn into atrial fibrillation.
Read more on this topic: Symptoms of atrial flutter
Irregular heartbeat
Atrial flutter often shows a course without the appearance of any symptoms. The diagnosis is therefore made by chance in the ECG.
The most common symptom of atrial flutter is an irregular heartbeat. Patients report a fluttering sensation in the chest, so-called Palpitations. This feeling can spread to the neck area, giving the patient the feeling that “the heart is beating up to the neck”. In addition, due to the irregular and sometimes rapid heartbeat, the patient can also notice a racing heart.
Typically, these symptoms appear suddenly in atrial flutter. They can wear off again after a while. Accompanying symptoms are often caused by the uncomfortable feeling of a fast and irregular heartbeat for the patient.
Shortness of breath
Another symptom of atrial flutter, which occurs especially with a very fast and irregular heartbeat, is shortness of breath. Due to the irregular beat, not enough blood can get into the circulatory system. The heart chamber already pumps the blood into the circulation before the chamber is completely filled with blood. The result is a backlog of blood (including in the lungs), which can cause shortness of breath. The patient is often concomitant with shortness of breath. In addition, pressure can also be felt on the chest.
Read more about this under Causes of shortness of breath
dizziness
In addition, many patients with atrial flutter report increasing dizziness. The inadequate pumping function of the heart results in an insufficient supply of blood to the brain. As a result, short-term clouding of consciousness with the risk of collapse can occur. A short-term, reversible loss of consciousness is also called syncope designated.
Due to the insufficient supply of blood to the brain, other accompanying symptoms can occur in addition to dizziness (paleness, nausea, sweating, etc.).
Read more about this under Causes of dizziness
sweat
The uncomfortable feeling of a fast and irregular heartbeat can cause accompanying vegetative symptoms. In many patients, the autonomic nervous system is activated (Sympathetic). As a result, there is increased perspiration in the body's sweat glands.
fear
In addition, the patient may experience anxiety from the sudden onset of a rapid and irregular heartbeat. By activating the autonomic nervous system, the heartbeat is additionally accelerated and the atrial flutter and its symptoms can be further intensified.
Diagnosis
First, the flutter will be examined in more detail, in order to Select suitable therapy method to be able to. It is important to know if this is a typical or atypical atrial flutter acts and whether maybe already thrombi in the atria educated to have. To do this, a EKG derivedin order to be able to localize the place of origin better. Both of them can here too Forms of flutter differed from each other become. In addition, a Ultrasound of the heart carried out to rule out that thrombi have already formed in the atria.
EKG

The electrical excitation can be measured by an EKG (electrocardiogram) can be visualized and recorded. Electrodes are attached to the chest according to a certain pattern, which can measure the excitation of the heart cells as a change in voltage. This process is also known as derivation. This takes place between two electrodes, each pair of electrodes can be assigned a lead. The result is the characteristic image of a heartbeat, in which both the electrical activation of the atria and the ventricles and the recovery of the heart's excitation can be read. In addition, the frequency and regularity of the heart's action can be mapped using the existing sequence of beats. It is also possible to determine the position of the heart by combining the individual leads.
This examination procedure is painless, non-invasive, and can provide a wide range of information. For example, cardiac arrhythmias, disorders of the conduction and spread of excitation, a heart attack or an inflammation of the myocardium make themselves noticeable in an EKG. Atrial flutter can also be shown in an ECG and is the main diagnostic method.
treatment
Since there is existing atrial flutter to Strokes to Thrombus formation in the left atrium or cause the ventricles to contract too quickly therapy quite quickly be sought. The target is here that End atrial flutter and the heart to a normal beat rhythm to return.
The procedure of Cardioversion applied. This can on the one hand over antiarrhythmic drugs take place, i.e. drugs that restore the normal rhythm. On the other hand, this effect can also be achieved by a Electric shock at the heart, which equates the activity of all heart cells, can be brought about.
With the latter method, the success rate is slightly higher, but it can be with one pre-existing thrombus in the forecourt to Loosen this thrombus lead and for example one Trigger a stroke. Both types of cardioversion can cause other abnormal heart rhythms.
Another option for treatment lies in the Catheter ablation. It can be used both as the method of first choice and after the failure of drug therapy. The prerequisite is that you have the Knows the origin of the self-activated excitation in the atrium. This is done through the so-called Mapping, in which the atria can be represented three-dimensionally using a specialized process. Of the Place of origin is then done using a catheter visited and tries that with an electrical impulse To desolate tissue at precisely this pointto break the excitement. If this project succeeds, the sinus node takes over the sole rhythm specification again.
Another procedure is the atrial overstimulation to disposal. Here is the Heart rhythm by means of a Pacemaker set slightly higher than normal. Some models can record the actual frequency of the heart and then specify a slightly increased rhythm. It has been shown that this prevents renewed atrial flutter.
For each form of therapy, certain requirements must be met that contribute to the success of the therapy.
Anticoagulation
During an existing atrial flutter, it may be necessary to take blood clotting medication.
Due to the very rapid contraction of the atria, the normal amount of blood cannot be transported further into the chambers, there is a restricted pumping function. Some of the blood remains in the atrium and the blood flow slows down. This combination of circumstances can lead to the formation of blood clots in the atrium. Should this blood clot break loose, the bloodstream will carry it into the chamber and possibly to the lungs or brain. There it could trigger a pulmonary embolism or a stroke, depending on the location. This risk can be reduced by taking anticoagulants, but a therapy that eliminates atrial flutter is always sought with as little loss of time as possible. If you take anticoagulant medication for a certain time, the general risk of bleeding increases during this time, even with harmless injuries.
Read more about this under
- Signs of a stroke
- How can you recognize a pulmonary embolism?
ablation
Drug therapy for atrial flutter proves to be very difficult. For this reason, the Catheter ablation ("targeted sclerosing") the therapy of choice for atrial flutter. In addition, ablation is a therapy option in which the patient can be completely cured of atrial flutter (curative method).
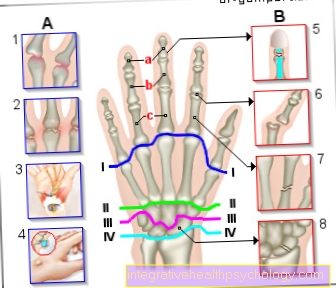
During catheter ablation, a catheter is pushed through a vessel in the groin area or the hand into the right atrium. With typical atrial flutter in the area of the tricuspid valve, the surrounding heart muscle tissue can be scarred with the help of the catheter, which suppresses the transmission of impulses. In the case of atypical atrial flutter, the circular excitation must first be precisely localized with the help of the ECG findings before an ablation takes place.
Catheter ablation is mainly used for recurring atrial flutter or chronic atrial flutter. This shows a very high probability of success (over 95%). The duration of the treatment is usually around 2 hours. General anesthesia is not required for therapy.
Electric cardioversion
Another therapy option for atrial flutter is electrical cardioversion. With the help of electrical surges, one tries to convert the disturbed heart rhythm back into the sinus rhythm and to maintain it. Correction of the heart rhythm takes place depending on the EKG (difference to acute defibrillation). The current surge is EKG-triggered at the time of the R-wave in the EKG.
The cardioversion takes place under continuous ECG monitoring and an intravenous short anesthetic. Therefore cardioversion is painless for the patient. It is an alternative to catheter ablation, especially in the case of very pronounced symptoms of atrial flutter or an acutely life-threatening disorder of the heart pump function.
Pacemaker
The implantation of a pacemaker in the case of atrial flutter is the therapy option of the last choice. An implantation is necessary if the above-mentioned therapeutic approaches do not lead to an improvement in the symptoms or if the heart rate cannot be slowed down with the help of medication.
As a rule, a pacemaker is implanted with simultaneous catheter ablation of the AV node. This enables the pacemaker to function as an electrical clock generator for the heart.
Read more about this on our main page Pacemaker
How dangerous can atrial flutter be?
Similar to atrial fibrillation, complications with atrial flutter can occur due to the irregular heartbeat. The most common and at the same time most dangerous complication is a thromboembolism. This is the formation of a blood clot within the atria that can spread through the ventricles into the arterial vessels of the body. It is particularly common for the blood clots to spread into the arteries that supply the brain, which obstructs the arteries and causes a stroke. In rare cases, a kidney or splenic infarction can occur due to the blood clot that has leaked.
Score
The CHA2DS2VASc score can be used to estimate the thromboembolism risk. This is usually calculated for patients with atrial fibrillation. As a rule, patients with atrial flutter have a slightly lower risk of thromboembolism than patients with atrial fibrillation.
The following parameters are taken into account by the CHA2DS2VASc score and each rated with one point: Chronic heart failure, arterial hypertension, diabetes mellitus, vascular diseases (CHD, PAD), age between 65 and 74 years, female gender. In addition, thromboembolism (or stroke) that has already occurred and an age over 75 years are rated with two points.
Depending on gender and point value, blood thinning therapy (Anticoagulation) required. Both vitamin K antagonists (Marcumar®), direct oral anticoagulants (Dabigatran, Apixaban, Edoxaban, Rivaroxaban) or Heparin be used.
Read more about this under
- blood thinner
- Effect of Marcumar®
How high is the risk of a stroke?
The CHA2DS2VASc score can be used to determine the risk of a stroke without blood-thinning therapy (Anticoagulation) estimate. The annual risk of a stroke with a CHA2DS2VASc score of 1 is approximately 1%. With a score of 4, the risk of suffering a stroke is already 4%. With a score of at least 6 points, the risk is already over 10%.
What other risks are there?
In addition to the risk of thromboembolism, other complications can arise from chronic atrial flutter. The clinical picture of heart failure can develop due to the permanently restricted cardiac output as a result of the irregular heartbeat. This leads to a backlog of blood in the body's circulation (including the formation of edema and ascites) and in the lungs (risk of pulmonary edema). This primarily affects patients with previously impaired cardiac pump function.
In addition, a long-term, fast and irregular heartbeat can damage the heart muscle tissue (Tachycardiomyopathy). This tissue remodeling also promotes the development of heart failure.
Read more about this on our main page Heart failure
How does atrial flutter affect my life expectancy?
Numerous studies and investigations in recent years have shown no influence of atrial flutter on life expectancy. However, a prerequisite for normal life expectancy is treatment of the disease and drug prevention of possible complications and risks.
In particular, patients under 65 years of age with previously healthy heart show a similar life expectancy to patients without cardiac arrhythmias. In patients who also suffer from heart disease (coronary heart disease, heart valve disease, heart muscle disease, heart failure), a few years or decades ago, a lower life expectancy was found due to atrial flutter. Due to newly developed, improved treatment options, however, the life expectancy of these patient groups nowadays hardly differs at all.