Inflammation of the gums
Synonyms
med. Gingivitis, ultis
engl. gingivitis, gum infection
introduction
Under the term "gingivitis" (Gingivitis) one understands an inflammation of the gums (lat. Gingiva). It can be divided into different degrees of severity and can be chronic or acute.

If left untreated, it often leads to inflammation of the periodontal structures, the periodontal disease.
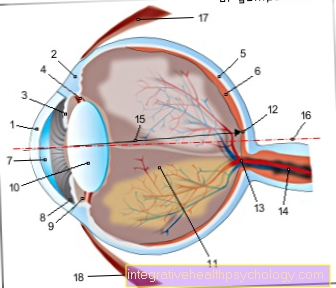
Illustration of a gingivitis

Inflammation of the gums
- Tooth enamel -
Enamelum - Gums -
Gingiva - Division point
of the tooth roots
(Fork) - Bifurcation - Alveolar bone
(tooth-bearing part of the
Jawbone) -
Pars alveolaris
(Alveolar process) - Cement -
Cementum - Root skin - Periodontium
- Nerve fibers and blood vessels
- Dental plaque
- Tartar (calculus)
- Inflamed gums -
Gingivitis - Pus - Pus
You can find an overview of all Dr-Gumpert images at: medical illustrations
Causes - an overview
Gum inflammation can be triggered by the following causes:
- Poor oral hygiene (dental plaque sticks to the teeth)
- Tartar
- Incorrect toothbrushing technique (too much pressure)
- Wrong toothbrush (bristles too hard)
- Tobacco use
- increased mouth breathing
- untreated carious teeth
- Life partner with inflammatory processes within the oral cavity
- hormonal changes during pregnancy
- general immune deficiency (immunodeficiency)
- Diabetes
- Genetic factors
Read more on the topic: Causes of inflammation of the gums
Causes in detail
The causes of gingivitis can be varied. In most cases, however, it is caused by plaque caused by bacteria (Plaque), which remains on the tooth surface for a long time, is triggered. Inadequate or simply incorrectly performed oral hygiene is the main cause. Plaque is a tough bio-film that consists of both food residues and waste products of bacterial metabolism and bacteria. The formation of a harmful bacterial flora can also be promoted by unhealthy breathing techniques such as mouth breathing.
Since the tooth surface is not completely flat even with healthy enamel, plaque can easily stick. If the plaque deposits are removed irregularly, they can even penetrate below the gumline. Over time, these deposits settle deeply around the tooth root and cause deep gum pockets over a relatively short period of time.
As a rule, the result is the development of severe inflammatory processes that cause enormous damage to the gums. Most patients notice small bleeding in the gum area at an early stage of the disease
Read more on the topic: bleeding gums
However, it has long been established that a number of other factors can also be responsible for the development of inflammatory processes in the area of the gums and the gums. These risk factors include:
It is estimated that every third patient from the age of around 40 suffers from inflammatory processes in the area of the gums. Most of those affected, however, do not have gingivitis (general inflammation of the gums) spread over the entire gums. In the majority of the observed cases, only isolated areas are affected. Areas that are difficult to access during dental care are particularly at risk (bridges, crowns, interdental spaces, nesting of teeth).
Inflammation of the gums due to stress
The Inflammation of the gums is so widespread in Europe in particular that one can assume that every second person will have at least one Inflammation of the gums developed.
In addition to the reasons already given, one seems to be long-lasting Stressfulness of the organism to promote the development of inflammatory processes in the gums. For many of those affected, this not only develops gum inflammation but also inflammation of the periodontium with involvement of the jawbone (Periodontal disease).
For a long time the connection between stress, a psychological phenomenon, and tooth decay or inflammation of the gums was not proven. However, modern studies indicate that people with a lot of stress are much more likely to be affected by these diseases. Causes for this can for example be through Lack of time represent neglected oral hygiene. It also helps with stress Messenger substances poured out which that Attack the immune system. Since not enough antibodies are then available, diseases can spread faster.
For further information see also: Bleeding gums due to stress?
Inflammation of the gums in pregnancy
The risk of gingivitis is significantly increased during pregnancy. The reason for this is the hormonal change with increased estrogen levels in the first 12 weeks of pregnancy. In addition to bleeding gums, gum growths also develop. These can mainly be found in the area of the toothed jaw, i.e. where there are still teeth. These lumps can be easily injured by, for example, crumbly foods and then become inflamed, causing severe pain.
Furthermore, these growths form pockets to the adjacent teeth. These are so-called "pseudo-pockets" because they disappear again after the disease has subsided.
However, with this type of bag there is a risk that deposits will accumulate there and caries will develop. Oral hygiene therefore plays a major role in pregnant women. To avoid bad breath and tooth decay, teeth should be cleaned properly every day. If the pain is too severe, a doctor must be consulted to combat the disease.
Although this is a special form of gingivitis, a disease of the periodontium (periodontitis) can follow without treatment.
As a rule, the gums calm down again after pregnancy with the normalizing hormonal balance.
You might also be interested in: Bleeding gums during pregnancy
Inflammation of the gums from smoking
Studies have shown that Smoke the risk of developing periodontal disease increases. In addition, smoking suppresses important warning signals. Constant contact with nicotine-containing smoke constricts blood vessels in the gums. The symptom of the Bleeding gums, which often occurs with gingivitis, is thereby suppressed. The actually sick smoker is apparently healthy, since an important symptom is eliminated.
The smoke becomes the Wound healing disturbedso that the immune system's regeneration reactions are greatly slowed down. Besides, the risk is one malignant tumor of the oral mucosa to get, greatly increased in smokers.
Smokers should therefore practice good oral hygiene and take regular preventive examinations in order to detect gingivitis or periodontal disease in good time.
You might also be interested in: Smoking diseases
Inflammation of the gums due to vitamin D deficiency
Several studies have shown that a vitamin D deficiency increases the risk of developing periodontal disease.
Vitamin D is a vitamin that is formed in the body with the help of solar radiation, so it is only available in sufficient quantities if you spend a certain time in sunlight or take it in from outside (via tablets or the like).
It is responsible for strengthening the bones and regulating cell growth. A lack of vitamin D can lead to gingivitis, which is particularly associated with bleeding gums. Without treatment, pocket formation occurs quickly. Bacteria can settle here and in the sore spots and then start to attack the bone. Periodontitis develops, which without treatment leads to tooth loss.
Read more on the topic: Vitamin D deficiency
Treatment options for gingivitis
Many home remedies and drugs available over the counter from pharmacies do not help very quickly in most cases. It often takes time for the inflammation to heal. However, if there is acute pain, one always hopes for quick help.The dentist can do this. In the practice, special ointments are available, which often bring relief with a single application.
Read more on the topic: What helps with inflammation of the gums? or betaisodona oral antiseptic
What can be done about the pain of inflammation of the gums?
Cooling the cheek helps against the pain associated with gingivitis. This will make the pain go away and the swelling will go down. You can still help with medication.
Local preparations, which are given directly to the inflamed area, can be purchased in the pharmacy. Dynexan®-Gel is applied several times a day with a cotton swab and relieves the pain. This gel contains lidocaine, an active ingredient that is also injected during dental procedures to numb the teeth.
Kamistad® also works on the same basis. However, it still contains chamomile flowers, which also have an anti-inflammatory effect.
Finally, you can also use tablets to achieve freedom from pain. Ibuprophen® or Paracetamol® are suitable here.
Read more on the topic: Ointments for gingivitis and lidocaine gel
Which drugs work best?
Above all, the drug Dontisolon® works very quickly. The active ingredient is prednisolone, a glucocorticoid. This prevents further inflammatory cells from penetrating the tissue and thus has an anti-inflammatory effect.
If the gums are bleeding profusely, the wound can be dabbed off with a medicine containing hydrogen peroxide. This is used for disinfection and can stop bleeding quickly and effectively.
The most important factor, however, is regular oral hygiene. Regular prophylaxis (brushing your teeth twice a day!) Often helps to reduce inflammation very quickly and prevent it in the long term.
Read more on this topic at: Medicines for gum inflammation
Ointment for gingivitis
One possible ointment is Solcoseryl® acute. The best thing to do is to get detailed advice on which product is best for you. Many are enriched with extracts from nature, the effects of which have been known for many years. Ointments with sage, rhubarb root, chamomile or myrrh are often found. Sage and chamomile have long been known to have a calming effect on inflammation in the mouth, relieve pain and combat inflammation.
Read more about this in the main topic: Dynexan® oral gel
You can help yourself with home remedies for gum inflammation. The mouth is often rinsed with sage or chamomile tea, as this also has a positive effect on inflamed areas, such as after a wisdom tooth removal. Its greatest benefit is in relieving pain, as this is the first thing one hopes for in therapy.
Some ointments also contain surface anesthetics, such as lidocaine hydrochloride, which reduces the capacity, external influences and stimuli that occur in the oral mucus during an inflammatory process. The sensation is quasi temporarily suppressed.
The ointments are used after the teeth have been thoroughly cleaned, which may also include a mouthwash, in order to additionally fight bacteria that are present in the presence of inflammation. The ointment is applied to the affected areas and gently massaged in.
It is not advisable to rinse your mouth or have a drink immediately after applying the ointment, as the ointment takes time to penetrate the tissue and would otherwise be washed away directly.
A visit to a dentist is urgently recommended, as only he can adequately treat the gingivitis. Ointments are usually not sufficient as the sole therapeutic agent.
Read more on the topic: Ointment for inflammation of the gums
Which mouthwashes help?
In the case of acute gingivitis, good oral hygiene should be observed. In addition to brushing your teeth twice a day for 3 minutes, this also includes the use of interdental brushes or dental floss as well as rinsing with a mouthwash. However, it should only be used in combination with these other aids. Simply using a rinse does not remove the bacterial film on the teeth.
There are different variants here with and without alcohol, With natural ingredients and / or with disinfectant propertieswhich can be purchased in drugstores. Fluoride-containing Rinsing solutions are also recommended.
In the pharmacy are preparations with CHX (Chlorhexidine) available. These have disinfecting properties and can kill all bacteria in the mouth. The disadvantage here is a brownish color Discoloration of teeth when the irrigation is over one used for a long time becomes. You should therefore just click Dentist's recommendation used and in no case longer than necessary.
If you don't like all artificially produced conditioners, you can also use a homemade conditioner made from strong chamomile tea, as chamomile has anti-inflammatory properties.
Home remedies for gingivitis
There are many home remedies for gingivitis. However, not all of them help equally. The following is a small list of useful resources:
- Chamomile is widely used and has a very good effect. As a tincture, compress or conditioner, it unfolds its disinfecting effect.
- Lavender can be drizzled on the sore area as an oil and has an anti-inflammatory effect.
- The same applies to garlic. A toe is chewed or a disc is placed on the inflammation. This allows the full effect to be developed.
- Cloves even have a pain-relieving effect. For this effect, chew a clove or add clove oil to the inflammation.
- Furthermore, there are many agents that have proven themselves as a rinse. Salt water, for example, kills germs and can stimulate saliva production. This should be used to rinse about 3 times a day.
- Pain can be relieved well by cooling. The blood vessels contract in the cold and the swelling also decreases.
- The most important thing about gum inflammation, however, is proper dental hygiene. Only those who take proper care of their teeth and gums can fight and sustainably prevent gingivitis.
Read more on the topic: Home remedies for gum inflammation
Tea tree oil for gingivitis
Tea tree oil is a well-known home remedy that is not only used in the oral cavity. Besides his anti-inflammatory effects, it disinfects wounds at the same time. This can effectively protect it from further spread. Even small inflammations should be treated with it at an early stage in order to alleviate worse processes. Farther promotes it the Healing process.
Just something for that Mix tea tree oil with lukewarm water and several times a day with this solution do the washing up. Intensive treatment is also possible by doing the Oil directly applied to the site of the inflammation with a cotton swab.
Chamomile for gingivitis
Chamomile is a medicinal plant. It contains essential oils, which have different effects. Especially those are in the mouth anti-inflammatory and the antibacterial effect not to be despised. With inflammation of the gums, bacteria can be killed at the same time and the inflammation can be positively influenced. You have to get one for that strong tea and then as a Flushing use.
It is also used as an active ingredient in various medicines, such as the Kamistad ointment. This is applied directly to the inflammation with a cotton swab.
Homeopathy for gingivitis
Homeopathic remedies should only be tried at the onset of gum disease. The remedy is used for bleeding gums and inflammation Mercurius solubilis applied. It can also be used in pregnant women and babies. However, this must be discussed beforehand with a naturopath, pharmacist or doctor.
Do these funds not help or exist inflammation already about one longer period, is a Visit to the dentist strongly advised. The risk would be too great if an underlying disease was left untreated for too long.
When do i need an antibiotic?
Antibiotics are very rarely used for gingivitis. There are many other remedies, such as ointments and home remedies, that can be beneficial for healing. However, if nothing helps and the inflammation persists for the time being despite all the identifiable causes, the dentist must consider taking antibiotics after a few weeks. However, it should really only be used in an emergency. As with an "ANUG" (acute necrotizing ulcerative gingivitis).
Find out more at: Antibiotics for gingivitis
Which antibiotic is best for gum inflammation?
Generally in dentistry the active ingredient has Amoxicillin proven. This is due to the penicillins and attacks the cell wall of the bacteria. It is given in tablet form, mostly one tablet in the morning and one in the evening.
This active ingredient can be administered in conjunction with clavulanic acid, a substance that is harmful to bacteria, in order to achieve an even more extensive effect. Then, for example, the drug Amoxicomp® is prescribed.
Should be a Penicillin allergy another drug must be used. It is essential to inform the attending physician of this, otherwise serious side effects will occur. It can affect the active ingredient Clindamycin can be used, which is also administered via tablets.
prophylaxis
Targeted prevention of gingivitis can basically be done by any resident dentist and trained specialist (Prophylactic aid; Dental assistant).
A special specialist in periodontics is recommended for patients who wish to prevent the recurrence of gingivitis as part of prophylaxis or for whom inflammatory processes have already penetrated other structures of the periodontium at an earlier point in time (Periodontists) to visit.
During the prophylaxis session, the patient is shown which areas of oral hygiene need to be optimized by coloring the plaque with a special dye. This is followed by specific instructions on a suitable toothbrushing technique, which is adapted to the special conditions within the oral cavity of the individual patient.
So-called professional teeth cleaning, which is carried out at regular intervals, should not be missing in any prophylaxis plan. In the course of this tooth cleaning, every single tooth is freed from plaque and tartar deposits on all sides with special instruments. The curettes or ultrasonic scalers can remove both soft and hard deposits from the tooth surface due to their individual cut.
Read more on the topic: Professional teeth cleaning
Alternatively, teeth can be cleaned using a small sandblaster-like device during the prophylaxis of gingivitis. From a technical point of view, however, this method is more than questionable, as the small particles of the emitter roughen the tooth surface and thus create new dirt niches.
The costs of the prophylaxis are not completely covered by the statutory health insurance. As a rule, only one grant is granted or one meeting is carried per year. The patient must therefore pay at least part of the amount himself.
However, regular professional teeth cleaning is not enough to prevent gum inflammation in the long term. Above all, the patient's oral hygiene, which is carried out correctly and regularly, is essential in order to avoid gingivitis.
Home remedies can also be used prophylactically.
Is gingivitis contagious?
When it comes to the question of whether gingivitis is contagious, the cause must first be addressed. If it is just a matter of a mucosal injury that has become a little infected, you can answer this question in the negative. Injuries can be caused, for example, by crumbly, coarse-grained food.
However, the disease is through bacteria then this can be caused by Transfer kisses become. This direct fluid exchange is required for “plugging in”. However, it cannot be said for sure whether the disease will actually break out in the other person. This depends on other factors, for example a poor state of the immune system, etc.
Be careful with the ANUG required, as this variant is very aggressive and also transferable is.
Symptoms
Inflammation in the gum area can usually be recognized quite quickly. The gums quickly lose their rosy, light color in the affected areas and become increasingly darker.
Bleeding along the gumline is considered to be the first and most important sign of gingivitis. Even at this stage of the disease, the patient can feel pain when brushing their teeth. In addition, severe redness and dark discoloration of the gum line are typical symptoms of gingivitis.
Read more on the topic: Pain in the gums
In addition to these signs, which appear very early, severely inflamed gums often react after a while with water and secretion deposits within the tissue. The result is increasingly swollen gums.
Read more on the subject at: Symptoms of gingivitis
Purulent inflammation of the gums
If pus occurs with a gingivitis, it is essential to make an appointment with the dentist. There the cause must be found and treated. Pus can appear on the gums in the following forms, among others:
1.) As pus vesicles on the gums - this is often a tooth root inflammation.
2.) As a secretion that emerges from the gap between the tooth and gums - this can be an acute osteomyelitis. Osteomyelitis is inflammation of the bone caused by bacteria. The bacteria may have entered the bone through a fractured jaw, a tooth destroyed by deep caries, or surgery.
3.) As deposits on the inflamed gums - this is often an acute necrotizing gum inflammation (ANUG), which is accompanied by destruction of the gums.
All of these diseases can cause serious consequences. A quick clarification is therefore in the interests of the person concerned. Therapy is initiated individually depending on the underlying disease.
Read more on the subject. Purulent inflammation of the gums
Inflammation of the gums and swollen lymph nodes
In very rare cases also occurs in gingivitis Swelling of individual lymph nodes in the neck on. They usually only enlarge when illnesses already affect you longer period persist and the body tries harder to fight the disease. Therefore, in this case, they indicate chronic inflammation of the gums. However, since there can be many other diseases with which enlarged lymph nodes are associated much more often, one should Clarification at the dentist definitely be done.
What are the consequences of gingivitis?
Gingivitis can develop if it persists without treatment Periodontal disease trigger. Periodontitis is a disease of the teeth supporting structures. The tooth-holding apparatus is the “anchoring system” that connects the tooth with the jawbone. If it is affected, after a while this can lead to the Loosen teeth. If no treatment is initiated, this process will progress and over time even lead to Tooth loss.
The difference between these two diseases is that the Reversible gingivitis, so completely heals, the periodontitis is not. In the best case, a stabilization of the condition found can be achieved here. Destroyed tooth retaining tissue can, however no longer built become.
Another unsightly side effect of gingivitis is a unpleasant bad breath. However, this will subside when the inflammation has healed through good oral hygiene.
Risks to the heart with inflammation of the gums
A gingivitis alone does not pose a threat to the heart. Only when the Inflammation spreads and periodontitis (inflammation of the tooth support apparatus, which can be associated with tooth loss) develops, the heart is at risk.
The risk of suffering from heart disease is then increased by around 50%. The reason for this are the bacteria that are found in the oral cavity of periodontal disease. These are anaerobic bacteria that survive without oxygen. These can be via a Inflammation of the gums with bleeding gums in the blood circulation get and about to the heart hike.
Is gingivitis an indicator of HIV?
At HIV positive patients is this Weakened immune system. The risk that diseases break out faster than in healthy people is therefore increased. Especially necrotizing ulcerative gingivitis (NUG) occurs here frequently. This is an aggressive variant of gum inflammation, which is associated with the death and decay of the gums. In addition, there is a general feeling of illness and pain. With this condition one should see a doctor immediately.
The normal gingivitis heard however Not to the typical initial symptoms of HIV infection. Everyone has had gum inflammation at some point in their life, and this should not be overstated. One should then see a doctor if symptoms occur during a longer time occur. Especially when there are other typical HIV symptoms.
Read on under: Bleeding gums as a sign of HIV infection?
forecast
Inflammation of the gums is a serious condition. In addition to the fact that a short time after the onset of the disease, the patient suffers from pain while brushing the teeth and from bleeding gums, there is a risk of developing periodontitis if a suitable therapy is neglected. It can be assumed that almost every untreated inflammation of the gums turns into real periodontitis.
The rapid initiation of targeted treatment measures after the appearance of the typical symptoms is therefore essential for the prognosis of gingivitis. In those cases in which the affected patient visits a dentist early, adequate treatment is provided and the patient regularly takes part in the scheduled follow-up sessions, gingivitis can usually heal completely.
It only becomes problematic when parts of the jawbone are already affected by inflammatory processes, when the gums have receded or when the patient does not practice proper oral hygiene despite training.
Duration of a gingivitis
Every gingivitis is individual and depends on general causes; No information can therefore be given about a precise period of time.
An acute inflammation of the gums normally heals within a week. Of course there are cases that take a longer or shorter period of time to heal.
If there is a local cause, such as a single gum pocket or a wisdom tooth that has just erupted, the dentist can often help with the application of an ointment.
Read more on the topic: Gingival pocket
With a hormonal change, as is the case in pregnancy, inflammation can take a little longer.
Other systemic causes, i.e. underlying diseases or vitamin deficiencies, can also weaken the immune system and often take a little more time.
The general rule is: Gingivitis should not be trifled with. A clarification of all cases with an unclear cause, which exist for more than a week, should be presented to the dentist. Adequate therapy can be provided here and the cause can be found so that periodontosis cannot develop in the first place.
Read more on the topic: Duration of a gingivitis
diagnosis
Extensive screening must be carried out before treating any possible inflammation of the gums.
This screening includes both the survey of the current tooth status and the assessment of the tooth supporting structure. This means that, in addition to documenting the condition of the tooth substance, the appearance of the gums is also precisely assessed. For this purpose, the dentist measures the depth of possible gingival pockets.
The measurement can basically be done in two different ways:
- Periodontal screening index (PSI for short) is measured on each tooth and a classification is made into various degrees of severity using codes 0-4. To assess the depth of the gingival pockets, the treating dentist inserts a blunt probe between the tooth substance and the gums. This is usually painless for the patient and completely harmless to the function of the gums. If there is a suspicion of gingivitis at this point, a special microbial test can be carried out in the course of the preliminary examinations to precisely determine the germs.
- Gingival bleeding index (GBI) is an index that does not provide information about the gingival pockets, but the general condition of the gums. The dentist will run a blunt probe along the gumline and watch for any bleeding.
In addition, the preparation of an X-ray image (Orthopanthomogram; short: OPG) can be useful in patients with severe clinical pictures. The OPG completely depicts the teeth in the jaw as well as the jawbone and the joints. It serves the dentist as an aid in assessing the condition of the bone structures involved. Only with the help of the orthopantomogram can one deduce how far the inflammatory processes have spread and how much damage they have already caused.
Types of gingivitis
1. Gingivitis simplex
The simple inflammation of the gums is caused by the bacterial plaque. It shows itself in a superficial Redness and swelling the gum line and can bleed easily if touched, for example when brushing your teeth. There is no influence on bone loss and no tooth loosening. The inflammation is not painful and is therefore often misunderstood. Treatment consists of removing plaque and may be supported by rinsing with anti-inflammatory drugs.
After eliminating the causal factors, this form of gingivitis heals quickly. If left untreated, however, it can develop into a disease of the gums.
2. Gingivitis gravidarum
Gingivitis gravidarum is a type of gingivitis that can occur during pregnancy. This form is not caused by bacterial plaque, it is hormonal. In contrast to "normal"Removing plaque does not improve gingivitis.
The reddened and swollen gums are more prone to bleeding than simple ones Gingivitis. The swelling leads to pseudo-pockets in which plaque can easily accumulate. After the child is born, this gingivitis also disappears again due to the change in the hormonal balance.
3. Desquamative gingivitis
This form of gingivitis can also be hormonal. It can occur in women during menopause / Menopause occur. Most of the time, however, it is the manifestation of another disease. That is why it is necessary to work with doctors from other fields, especially dermatologists.
In this form of gingivitis, the connective tissue of the gums is changed and the surface can easily be peeled off. The gums are very red, smooth and shiny, they are painful and bleed easily. The entire gum is not changed, but can only be limited to a few areas. Dental treatment consists of treating pain and avoiding additional infection through careful oral hygiene. It is important to identify the underlying physical disease and treat it.
4. Ulcerative gingivitis
This is an inflammation of the gums that is accompanied by ulcers. It begins at the gingival papilla in the interdental space and then extends to the gum line. The result are defects in the tissue. The ulcers can also spread to the lining of the mouth. Treated with antibiotics in good time, healing can take place, otherwise defects in the interdental space and an infestation of the tooth support system remain.
5. Hemorrhagic gingivitis
The predominant symptom with this type of gingivitis is bleeding from the connective tissue of the gums. It starts in the interdental space and then continues to the rest of the gums. As the gums deteriorate, the teeth loosen up and eventually lose them.
This clinical picture is observed in scurvy, i.e. the lack of vitamin C, and is therefore extremely rare today, as a vitamin C deficiency practically no longer occurs with today's diet.
6. Neoplastic gingivitis
This is an overgrowth of the papillae in the interdental space, which can cover the entire tooth, mainly in the anterior region. It is not a product of inflammation, but rather a natural condition. The growths are benign and can be surgically removed. However, there is a high probability that it will occur again. Similar growths are possible with chronic use of anti-epileptic drugs. Therapy consists of stopping the drug or, if that is not possible, surgical removal.
7. Toxic gingivitis
Toxic gingivitis / gingivitis is based on heavy metal poisoning with lead or mercury. A bluish to black border forms along the gums. It is believed that these are sulfur compounds. The concentration of mercury that may be released from amalgam fillings is nowhere near enough to lead to this clinical picture. Rather, the dangers lie with workers who deal with the mining or processing of heavy metals.
Read more on the subject at: Mercury poisoning
8. Gingivitis in diseases of the blood
In leukemia (cancer that affects the blood-forming system), swelling and inflammation of the gums can occur. The treatment depends of course on the underlying disease.
Summary
Inflammation of the gums can vary greatly in terms of severity, cause, tendency to bleed and treatment options. The therapy ranges from careful oral hygiene, see also: professional teeth cleaning. to surgical treatment. Any change in the normal pink color should be a reason to visit the dentist to clarify the cause.