Start and duration of thrombosis prophylaxis
Note
General information on the topic of thrombosis prophylaxis can be found on the start page on the topic: Thrombosis prophylaxis
Start of prophylaxis
Of the Start of thrombosis prophylaxis should be as early as possible on the situation causing the risk.
In the inpatient surgical departments, thrombosis prophylaxis is nowadays routinely routinely performed both peri- and post-operatively. carried out until discharge. If there is a need for discharge (e.g. a Hip prosthesis) prophylaxis must also be given after discharge.
Duration of thrombosis prophylaxis
The duration of the prophylaxis depends on the persistence of the risk factors.
There are currently no fixed rules as to how long exactly thrombosis prophylaxis should be carried out.
Several studies on the subject of thrombosis prophylaxis provide initial information for various risk profiles. So should patients
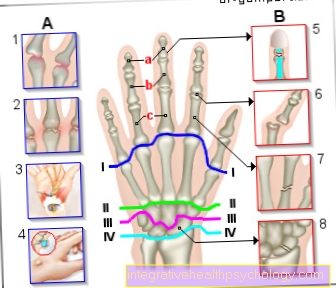
- With Hip prosthesis
- after hip fractures / Femoral neck fracture
or - after surgery one malignant tumor
receive postoperative drug thromboprophylaxis for about 4 - 5 weeks.
According to the guidelines of the German Society for Surgery 2003, the duration of prophylaxis after an operation should be determined by the additional dispositional risk factors, the operative trauma and the degree of immobilization.
For outpatient surgical interventions, thrombosis prophylaxis is recommended for the duration of the immobilization of the operated extremity.
Special feature during surgery
In operations with anesthesia procedures close to the spinal cord, drug thrombosis prophylaxis may only be carried out after removing the catheter at a safe time.
For some interventions (e.g. in the head and neck area), no drug prophylaxis is recommended unless there are additional risk factors.
Read more on the topic: Xarelto®
Classification
In the Thrombosis prophylaxis a distinction is made physical and drug measures.
To the physical measures count among others:
- Mobilization
- storage
- Stroking the veins
- Vein compressions
- Promotion of the return flow through gymnastics
A number of different drugs are available for drug intervention, which are intended to reduce the blood's ability to clot.
The points of attack are the various components of the coagulation system. The differentiated use and dosage of the Medication depend on the risk profile of the person concerned.
Blood clotting physiology
To better understand the various measures of thromboprophylaxis, it is helpful to know some basic facts about blood clotting.
The following are essentially responsible for blood clotting:
- the nucleated blood platelets (thrombocytes)
- the coagulation factors
- as well as some other factors
One shares them Blood clotting (also hemostasis) into a primary and secondary hemostasis. Furthermore, the speed of the blood flow, the composition or the viscosity of the blood and the willingness to clot are of decisive importance (Virchow triad).
The Coagulation factors IX, X, VII and II are in their function of Vitamin K dependent. Primary and secondary hemostasis, as well as the endogenous and exogenous pathway, neither take place alone nor one after the other, but rather in parallel.
Primary hemostasis and platelet function
goal of primary hemostasis is the hemostasis through the formation of a platelet clot (thrombus). Platelets, of course, as well as a number of different factors (e.g. von Willebrand factor) and receptors. Does it come e.g. If a blood vessel is injured, it contracts in the primary reaction (vasoconstriction) in order to minimize blood loss and slow down blood flow.
The components of the now exposed tissue as well as the inner layer of the vessels (Endothelium) now ensure that the platelets from the bloodstream can adhere exactly there.
The Platelets are further activated by clinging, emptying their content and changing their shape. With the formation of a plug (also called a white deposition thrombus), primary hemostasis is complete. It serves to "temporary waterproofing“.
Secondary hemostasis
For permanent closure, the plug must be replaced with a fibrin thrombus. This must be done in the inactive prepress in blood occurring Fibrinogen (or factor I of the blood coagulation cascade) can be converted to fibrin. This requires a relay-like activation of various coagulation factors in the blood.
This preceding blood coagulation cascade consists of an exogenous (or extrinsic) and an endogenous (or intrinsic) path, which represent different activation pathways and lead to a common end path.
To the endogenous way count the Factors XII, XI, IX, VIII such as Calcium as the most important components.
To the exogenous way count especially factors III and VII as well as likewise Calcium.
The common final section begins with the activation of factor X and the other factors V, II, XIII and I.
The fibrin, which is now activated at the end of the cascade, is cross-linked and glued and is ultimately called red thrombus referred to as the other components of the blood composition (e.g. the red blood cells) are caught in the fibrin network.
Laboratory chemical testing
Of the endogenous way can be done in the laboratory by the so-called Partial thromboplastin time PTT be measured.
Of the exogenous way is through the Quick value or. INR checked.
Both test methods also measure the common end route.