Chronic gastric mucosal inflammation
introduction
In general, one can say that an existing discrepancy between factors that damage the mucous membrane (e.g. stomach acid) and factors that protect the mucous membrane (mucous layer) lead to a chronic gastritis can lead.

Types of gastric mucosal inflammation
There are basically 3 different types of chronic Inflammation of the gastric mucosa:
- Type A gastritis
- Type B gastritis
- Type C gastritis
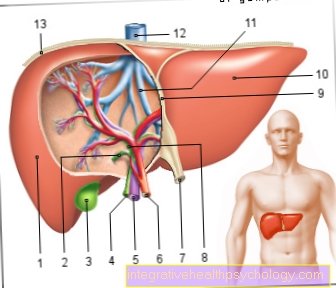
Gastritis anatomy

The detail shows the gastric mucosa enlarged.
The mucous membrane defects, which appear as red spots in the mucous membrane, as areas of locally increased blood flow and, in some cases, bleeding into the mucous membrane tissue of the stomach, are clearly visible.
As the disease progresses, stomach ulcers can also form, which can break through the stomach wall.
Particularly in the chronic form of gastric mucosal inflammation, there are visible changes to the gastric mucosa.
causes
Type A gastritis
This shape is a Autoimmune disease, in which the body's own antibodies against the parietal cells (which produce gastric acid) are caused by a dysregulation of the immune system Gastric mucosa straighten them and thereby destroy them. In some cases, the antibodies are also directed against those produced by the parietal cells Intrinsic factor. This substance is needed later to transport vitamin B-12 through the mucous membrane of the small intestine, so that a lack of intrinsic factor automatically becomes one lack of Vitamin B12 leads.
This gastric mucosal inflammation mainly affects the mucous membrane of the gastric corpus and is therefore also called "corpus gastritis" (see also stomach).
Overall, type A gastritis represents about 5% of all chronic gastritis and is excessively common with other autoimmune diseases such as Rheumatoid arthritis (Rheumatism) and systemic lupus erythematosus associated. In rheumatoid arthritis, autoantibodies form against the synovial membrane.
In type A gastric mucosal inflammation, the parietal cells are more and more destroyed in the course of the disease, so that at some point stomach acid can no longer be formed.
This state is then called Achylia gastrica or Achlorhydria (Absence of gastric juice).
Type B gastritis
90% of this form of gastritis is caused by the bacterium Helicobacter pylori caused. In the remaining cases, less common bacteria and viruses can lead to this chronic gastritis. The colonization of the gastric mucosa by the Helicobacter pylorus Bacteria (germ) are widespread and the number of colonized people increases steadily with age, so that it is assumed that almost 60% of those over 60 years of age have the germ in the gastric mucosa.
However, that does not mean that everyone suffers from inflammation of the gastric mucosa. The germ often goes undetected precisely because of the lack of symptoms. The bacterium has the enzyme (active protein) Ureasewhich can split urea into ammonia and carbon dioxide (CO2).
The alkaline ammonia obtained in this way neutralizes the hydrochloric acid and thus protects the bacterium from being decomposed by gastric acid and thus ensures its survival in the acidic environment. The inflammation mainly affects the gastric antrum (see also stomach) and will therefore "Antral gastritis" called. Type B - gastric mucosal inflammation, is the most common chronic gastritis with 85%.
Type C gastritis
The causes of type C gastritis are chemical-toxic factors. Pain medication like Acetylsalicylic acid (ASS, aspirin ®) and NSAIDs, such as. Voltaren or ibuprofen, which reduce the blood microcirculation in the gastric mucosa, often cause this type of gastric mucosal inflammation, especially in patients with chronic pain Medication are instructed daily. Longtime Alcohol and nicotine addiction (abuse) also often leads to this type of gastritis.
In some cases the Bile acid reflux from the Duodenum (Duodenum) represent the cause of the inflammation. At 10%, this form is the second most common cause of chronic gastritis and it particularly affects the gastric fundus (see also stomach).
Chronic inflammation of the stomach lining due to stress
A lot of stress is one of the main risk factors for chronic gastric mucosal inflammation, in this case from one Type-C-Gastritis is the topic. The body works at full speed under stress, and the adrenal glands release the "alarm messengers" adrenaline and noradrenaline as well as the stress hormone cortisol. Cortisol in turn has a stimulating effect on the gastric mucosa, so that specific cells (main cells) produce more stomach acid.
Excessive acid production can disturb the balance of gastric juice components that are aggressive to the mucous membrane (gastric acid) and protective mucous membrane (neutralizing protective mucus), so that aggressive factors predominate and permanently damage the gastric mucosa and cause inflammation.
Symptoms / complaints
As a complication of the chronic Inflammation of the stomach lining Type B and C can be a Gastric ulcer (Ulcer) occur, which accumulated to a acute gastric bleeding can lead. As already described for acute gastritis, gastric bleeding can appear differently. Indications can be hidden (occult) blood in the stool, tarry stool, as a coffee grounds-like mass or white blood in the vomit.
The persistent immune-controlled inflammation in type B gastric mucosal inflammation causes the mucous membrane to recede over time (atrophy). Due to its chronic irritation, it changes into a different type of tissue. The pathologist calls this process Metaplasia of the tissue.
This tissue is more likely to be malignant (malignant) to degenerate and can therefore to Stomach cancer (Gastric CA) lead.
Autoimmune gastritis (type A) also leads to severe atrophy of the mucous membrane and even to a three to six-fold increased risk of gastric cancer.
In type A gastric mucosal inflammation, the lack of gastric acid leads to an increased stimulus on the G cells, which then increase Gastrin pour out. This excess hormone stimulus can cause other tissues to become malignant, so that more hormone-producing tumors develop, so-called Carcinoids.
Read a lot more information on this topic at: Symptoms of inflammation of the stomach lining
diagnosis
Clear indications of the suspected diagnosis of gastritis can already be obtained in the patient interview (anamnesis) by asking about medication and consumption habits (alcohol, nicotine). In type A gastritis, the causative ones are often found Autoantibodies in the blood that are directed against parietal cells and the intrinsic factor. The lack of intrinsic factor can mean Schilling test be diagnosed.
A Anemia (pernicious anemia), which can be seen in the blood count, can also refer to type AInflammation of the stomach lining Clues. Usually only one brings Gastroscopy (gastroscopy) final clarity on the diagnosis and extent of the mucosal damage. The 13C-urea breath test can be used to diagnose Helicobacter pylori colonization. Otherwise the bacterium is detected in tissue samples from the stomach.
Schilling test
This test measures the absorption capacity of Vitamin B12 checked in the small intestine. First, the gastric patient is given vitamin B-12 and then checked how much of it is absorbed into the blood. The second step is to give both vitamin B-12 and Intrinsic factor and again looks at the concentration of the vitamin in the blood. If there is more vitamin B-12 in the blood on the second dose, it can be assumed that there is an intrinsic factor deficiency. However, if the blood shows little vitamin on the second try, the problem could most likely be am Small intestine and its mucous membrane itself.
Gastroscopy
The appearance and location of the inflammation alone provide the doctor with important information about the type and cause of the gastric mucosal inflammation. The gastroscopy initially shows stunting (atrophy) of the stomach lining. With the "mirroring" of the stomach, statements about existing Mucosal defects (erosions) or Ulcers (Ulcers) to be hit.
With the removal of a Tissue sample (biopsy) a better statement about the inflammation process can be made under the microscope. In the case of gastritis, the pathologist recognizes a surface reduction of the mucous membrane with flattening of the folds of the mucous membrane and the glands under the microscope.
In the event of an attack by the Helicobacter pylori bacterium, the inflamed inflammatory cells (inflammatory infiltrate) can be recognized, especially in the gastric antrum. In addition, a piece of tissue can be used to make a Urease test perform.
Urease test
In this test, the piece of tissue is placed in a medium for 3 hours. Due to the ammonia, which is formed by the bacteria's own enzyme urease, the medium changes color and the detection of the bacterium Helicobacter pylori is quick and cheap.
C13 urea breath test
During this test, the patient is given a C13 (or 13C) labeled urea (non-radioactive) administered through a drink. The patient must then exhale vigorously through a straw into a special glass tube. By splitting this urea into CO2 and ammonia, the labeled 13C can be measured in the exhaled CO2. With this not entirely cheap method, after antibiotic therapy, you can check whether the eradication of the Helicobacter pylori bacterium was successful.
The advantage of this examination is that it is non-invasive and non-stressful for the body.
Therapy for chronic gastric mucosal inflammation
As a general therapy for gastric mucosal inflammation, care should be taken to avoid substances irritating to the stomach such as coffee, alcohol, nicotine and spicy food is avoided.
Type A gastric mucosal inflammation:
In autoimmune gastritis, one does not treat the cause of the inflammation, only the symptoms and complications that arise. You have to give these patients what they lack for life Vitamin B12 Artificially replace it with an intramuscular syringe (injection). Because of the increased risk of gastric cancer and carcinoids, an endoscopic check-up must be performed annually to detect cancer (Stomach cancer) to identify and treat at an early stage.
Type B gastric mucosal inflammation:
The Helicobacter pylori bacterium must be associated with a Antibiotic therapy be treated (Eradication therapy). You use several for this Antibiotics at the same time (triple therapy) in order to be able to fight the bacterium effectively and to prevent the formation of resistant strains.
Two antibiotics such as amoxicillin and clatrithromycin are administered over 7-10 days (alternatively also Metronidazole) and a proton pump inhibitor (e.g. Omeprazole), which reduces gastric acid production. The success of the therapy can be checked about four weeks after the therapy using the 13C-urea breath test or an endoscopic examination with tissue removal (biopsy).
Type C gastric mucosal inflammation:
In this form of gastritis, the triggering chemical substance, often drugs such as NSAIDs, be dropped off; be discontinued; be deducted; be dismissed. If this is not possible, a stomach protection preparation (Proton pump inhibitors) to intercept the harmful effects of such drugs.
This often happens when NSAIDs (e.g. Voltaren) and similar substances are prescribed for the first time in order to prevent gastritis from developing in the first place if they are taken for a long time.
When consuming alcohol and nicotine, these pollutants (noxae) must of course be avoided.
With an existing bile acid reflux one can with the administration of certain drugs, the so-called Prokinetics how Metoclopramide (Paspertin) to provide relief.
Prokinetics accelerate the passage through the stomach, which means that harmful substances are removed from the stomach more quickly.
The drug Cholestyramine binds bile acids and thus improves bile reflux.
<- Back to the main topic gastric mucosal inflammation
Chronic gastric inflammation medication
The medication that can be taken for chronic gastric mucosal inflammation depends entirely on the type of inflammation or the underlying cause.
Is it a chronic one? Type-A-Gastritis, an autoimmune disease, is a lifelong delivery of Vitamin B12 necessary because the gastric mucous membrane cells can no longer produce this.
In the Type-B-Gastritis, which is usually based on a bacterial colonization with Helicobacter pylori, requires drug control, often in the form of a combination of three Acid blockers (e.g. omeprazole / pantoprazole) and two different antibiotics (Amoxicillin / clarithromycin or clarithromycin / metronidazole).
The chronic one Type-C-Gastritis benefits solely from the elimination of the harmful noxa, such as the withdrawal from medication, the reduction of stress, etc.
also read: Medicines for gastrointestinal diseases
Home remedies for chronic gastric mucosal inflammation
In the case of chronic inflammation of the gastric mucosa, care should be taken to reduce or even avoid irritating foods such as coffee, tea, cola, acidic juices and spices. Smoking, alcohol consumption and excessive consumption of meat products should also be stopped. The reduction of stress through e.g. Relaxation therapies can be useful. Under certain circumstances, it can even be limited to a few days Fast be conducive to healing, or at least a light, low-fat, low-carbohydrate meal.
Chamomile and fennel teas can have a calming effect on the stomach and alleviate the symptoms. Ginger tea can also have anti-inflammatory effects. Other foods with anti-inflammatory effects are cabbage juice and products containing mucus, such as porridge, raw potatoes or mallow leaves / blossoms.
also read: Home remedies for stomach cramps and Home remedies for stomach ache
Duration of chronic gastric mucosal inflammation
How long a chronic gastric mucosal inflammation lasts cannot be said in general terms, the healing process can vary greatly from person to person and depends on various factors. In contrast to acute gastric mucosal inflammation, which subsides without consequences after a few days, one speaks of chronic gastric mucosal inflammation when the symptoms are over Weeks to months last for. In the worst case, there is chronic inflammation of the gastric mucosa even for a lifetime and can therefore not be fully treated for recovery.
It is important, however, that those affected do not necessarily have to have permanent symptoms and complaints: a chronic gastric mucosal inflammation that lasts for months to years can flare up and flatten out again and again in its inflammatory activity, i.e. it can progress in spurts, whereby the inflammatory phases are usually triggered by various factors can.