The temporomandibular joint
med .: Articulatio temperomandibularis
introduction
The joints ensure the mobility of the human body. They connect one or more bones together. Depending on your tasks, we differentiate between:
- Ball joints
- Hinge joints
- Socket joints
- Sliding joints
- Swivel joints
The temporomandibular joint (Articulatio temperomandibularis) is a swivel and sliding joint. The joints have a complicated structure and make high demands on diagnostics and therapy.

Structure and function of the temporomandibular joint
The socket of the temporomandibular joint is located close to the ear canal and is firmly connected to the temporal bone. The counterpart is the jaw head, a bone process of the lower jaw. Like the other joints, the joint surfaces are covered with cartilage. The entire joint is enclosed in a joint capsule. A thick synovial fluid ensures better gliding ability. Between the two joint surfaces there is a cartilage disc that divides the joint into an upper and a lower half. When moving the jaw, you can feel the joint in front of the ear.
The two jaw joints connect the upper and lower jaw with each other. In the case of rows of teeth lying on top of one another with the mouth closed, the joint heads should lie centrally in the joint socket. Any deviation from this position is registered by the joint and tries to compensate for it. This leads to a one-sided exposure to TMJ pain. The causes must be eliminated. The temporomandibular joints ensure that the oral cavity opens and closes. Because they can be rotated, they allow food to be ground. They are also involved in speaking and swallowing.
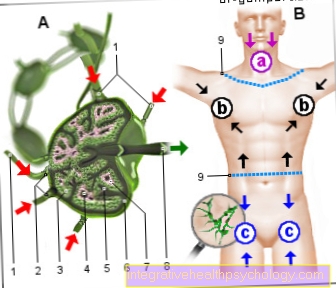
TMJ anatomy
The anatomy of the jaw in the human body is such that optimal food intake is possible. Components are the upper jaw and lower jaw, which can hardly be compared with one another because they are structured so differently.
- The upper jaw bone has a loose, honeycomb structure while the lower jaw bone is much more dense. Both jaws are used to attach the rows of teeth. In the upper jaw, the roots of the teeth are close to or even partially in the two maxillary sinuses. The upper jaw is firmly fused with the bony palate plate, the maxillary sinuses, the nasal bone and the cheekbone.
- In the lower jaw there is a canal that contains blood vessels and nerves that innervate and supply all of the lower teeth with nutrients. The lower jaw is movable and connected to the skull via the temporomandibular joint, while the upper jaw is an integral part of the skull bone and cannot be moved.
Figure upper jaw

- Upper jaw -
Maxilla - Zygomatic bone -
Os zygomaticum - Nasal bone -
Nasal bone - Tearbone -
Lacrimal bone - Frontal bone -
Frontal bone - Lower jaw -
Mandible - Eye socket -
Orbit - Nasal cavity -
Cavitas nasi - Upper jaw, alveolar process -
Alveolar process - Maxillary artery -
Maxillary artery - Under eye cavity hole -
Infraorbital foramen - Ploughshare - Vomer
You can find an overview of all Dr-Gumpert images at: medical illustrations
Figure lower jaw

- Lower jaw - Mandible
- Crown process -
Coronoid process - Lower jaw rest -
Ramus mandibulae - Mandible angle -
Angulus mandibulae - Upper jaw - Maxilla
- Zygomatic bone - Os zygomaticum
- Zygomatic arch -
Arcus zygomaticus - Temporomandibular joint -
Articulatio temporomandibularis - External ear canal -
Meatus acousticus externus - Temporal bone - Temporal bone
- Frontal bone - Frontal bone
- Chin hole - Mental foramen
- Eye socket - Orbit
- Upper jaw, alveolar process -
Alveolar process
You can find an overview of all Dr-Gumpert images at: medical illustrations
Jaw muscles
The jaw muscles or masticatory muscles are a group of muscles that enable all movements and functions of the jaw and the joint. The masseter muscles include four different muscles that all have different functions and are present once on both sides of the jaw.
The only one of them that is responsible for opening the mouth is that Lateral pterygoid muscle. When this muscle is simultaneously tensed on both sides, the jaw is moved forward, which initiates the opening of the mouth. In contrast, all three other muscles are responsible for closing the jaw. Of the Masseter muscle, of the Medial pterygoid muscle, as well as the Temporalis muscle.
With the help of these muscles, the jaw can exert insane forces, and it is not uncommon for forces of over 100kg / cubic centimeter to arise.
Read more under: jaw muscles
What complaints can occur in the temporomandibular joint?
Three symptoms dominate the symptoms of TMJ disorders:
- Pain
- Temporomandibular joint cracking and
- Restrictions on movement.
In the case of TMJ and osteoarthritis, the pain determines the picture. The pain can not only be limited to the temporomandibular joint, but can also radiate. The jaw clamp and the jaw lock are noticeable in the inability to open or close the mouth. Most often, a cracking of the temporomandibular joint is noticeable, which, if there is no cover bite, requires further diagnostic measures.
Diseases of the jaw
- Cranio-mandibular dysfunction (CMD)
- Jaw misalignments
- Tumors of the jawbone
- Articular cartilage tumors
- Ankylosis of the temporomandibular joint
- Arthrosis of the temporomandibular joint
- Condylar hyperplasia of the lower jaw
- Pine necroses
- Jaw cysts
- Broken jaws
TMJ inflammation
Inflammation in the joints is called arthritis. The cause of this can be traced back to many factors. One of the most common is the development of an inflammation due to a permanent improper load, such as the nocturnal crunch. The temporomandibular joint does not have enough time to recover and is permanently heavily stressed.
The joint can also catch fire if the teeth are incorrectly connected.This can be due to gaps in the dentition or an inadequately adapted prosthetic restoration such as crowns, bridges or prostheses. If a crown is made too high, one side of the joint will make contact earlier than the other and the joint will be put under incorrect stress. This can also be a trigger for crunching. With the many movements that we perform with it during the day, inflammation is a normal consequence. Inflammation is also possible if there is traumatic damage to the teeth, such as after an accident or an operation.
The symptoms of a temporomandibular joint inflammation range from pain, to cracking, to ear pain and headache. The pain can become so severe that it is difficult to eat. The tissues, like bone, begin to wear off and thicken. There is also fluid build-up. The temporomandibular joint is being destroyed more and more.
The treatment measures depend on the respective condition of the joint. But you want to be as invasive as possible, so that medication is prescribed, a splint is made and physiotherapeutic treatment is initiated.
Read more on the topic: TMJ inflammation
Temporomandibular joint cracking
The jaw joint cracking is one of the most common abnormalities in the oral cavity. Usually it is accompanied by temporomandibular joint pain, ear pain, headache and tension. The cracking is a symptom that indicates that something is wrong with the temporomandibular joint. The causes of the jaw joint cracking can be very diverse.
It can be caused by crunching at night or by misalignments in the teeth and consequent incorrect stress on the joint. The eruption of the wisdom teeth can lead to constriction in the teeth, so that the existing teeth shift. As a result, normal occlusion is no longer given and the temporomandibular joint can be incorrectly loaded. But a gap in the dentition or an incorrect prosthetic fitting are also possible triggers.
Uneven tooth positions or excessive elevation of individual teeth / tooth can lead to one-sided overload and pain in the joint. Arthritic inflammation or osteoarthritis can also affect the temporomandibular joint, as with other joints. It is not uncommon for patients to come and report that the temporomandibular joint cracks when opening and closing. The cause is usually a cover bite in which the upper front teeth are too steep and deep above the lower teeth. As a result, the lower jaw has little freedom of movement and the jaw joint cracks.
The Craniomandibular dysfunction usually manifests itself in the jaw joint cracking, just like a temporomandibular joint inflammation. If the causes mentioned above lead to an incorrect load, the one wears out Articular discso that it is no longer correctly fixed. If you now make movements, it does not physiologically follow the head of the temporomandibular joint, but jumps in front of or on top of it. This jumping is perceived by us as a crack. In addition to these factors, bacterial or viral infections can also affect the temporomandibular joint.
A displacement of the inter-cartilage disc can also cause the jaw to crack. If the head of the jaw slips out of the socket, the jaw locks, i.e. the patient can no longer close his mouth. This is usually the result of opening the mouth excessively when yawning. The opposite occurs if, for example, the mouth can no longer be opened due to inflammation or swelling in the back of the teeth. This is a jaw clamp. This can be the result of a difficult eruption of the wisdom tooth, or of inflammatory swellings after surgical removal of the wisdom tooth.
Splints are usually used for therapy, which prevent crunching at night or enable a correct bite, which prevents incorrect loading. Physiotherapy is also carried out if there are major problems. However, an individual diagnosis and tailored treatment are necessary for each patient.
TMJ osteoarthritis
In general, an osteoarthritis of the TMJ is a wear and tear that is comparable to osteoarthritis of the knee or hip. All of these diseases occur at an advanced age (from the age of 60) and the cause is wear and tear on the joints. The cartilage that cushions the joint becomes thinner over the years and contains less water, which makes it crack.
In addition, TMJ osteoarthritis is a breakdown of bone caused by wear and tear and abnormal movements. This wear and tear can lead to restricted mobility and severe discomfort with any movement.
In contrast to hip and knee joint problems, the replacement of the joint in the temporomandibular joint is far from being as established. This is because the temporomandibular joint is much more complex, since it is not a pure swivel or sliding joint, but both at the same time. The individually manufactured replacement joints cannot yet fully reproduce all functions, which is why TMJ osteoarthritis is often only treated conservatively. Attempts are made to flush the temporomandibular joint with minimally invasive surgical techniques and thus relieve tension. Therapeutic approaches with botox are also becoming more and more popular to alleviate the symptoms.
Broken jaw
The jaw fracture represents an injury to a jaw (upper or lower jaw), which is comparable to bone fractures on other skeletal bones. These fractures can result from an accident, but also after a surgical tooth extraction or a disease such as a tumor or a cyst.
Due to its anatomical structure, the lower jaw bone has some places that can break quickly and where mostly jaw fractures occur. This includes the ascending branch to the temporomandibular joint head, which is a weak point. The region under the respective canine tooth is also such a point, because the length of the canine tooth root means that the bone thickness is much thinner here than in other places. In a wisdom tooth operation, this often has to be milled out of the bone compartment, which leaves a thin layer of bone.
If the patient eats very hard foods too soon, the jaw can give way and break. Tumors or cysts can also weaken the bone so that it can break there. If the fracture is displaced or broken, it must be surgically fixed with small plates and screws (osteosynthesis plates). These titanium devices prevent the fragments from rotating and keep them rigid so that the bone can regenerate. Healing is usually achieved after six to eight weeks.
Dislocated jaw
With extreme movements of the jaw, the joint head can get caught in front of the joint cusp and thus be dislocated. In the case of a complete dislocation, one speaks of a dislocation or, in the case of a partial dislocation, of a subluxation. These excessive movements include, for example, opening your mouth when you yawn or vomit.
Patients can no longer close their mouths with a complete dislocation. The lower jaw must first be adjusted so that the jaw lock is guaranteed again. The doctor performs this treatment with the so-called Hippocrates handle. When setting, the lower jaw must first be pressed downwards and then combined backwards in order to bring the joint head of the temporomandibular joint under the articular cusp by which it is hooked and to restore the physiological position of the head in the joint pit. The treatment of straightening is an act of a few seconds that can be painful for a short time. Usually, however, no anesthesia is used for this procedure.
After the adjustment, all functions of the TMJ are usually restored and any movement can be exercised again. If severe symptoms persist after the straightening, an injury to the ligaments and muscles or the cartilage may be the cause. If the pain persists even after several weeks, it is advisable to visit the dentist who will prepare a DVT to find out the cause of the TMJ problem and then to treat it accordingly.
Read more on the topic: Dislocated jaw
Jaw misalignment
A jaw misalignment is part of the term Dysgnathias, which means that the normal position of the jaw and teeth has changed. A subdivision is made as to whether the misalignment has a skeletal, i.e. bony, or a dental origin, which affects the teeth. Skeletal dysgnathias include, for example, an upper or lower jaw that is too small or too large.
An example case is a protruding lower jaw that prevents the upper jaw from growing.
A cleft lip and palate also belongs to this group. The misalignments that affect the teeth usually represent poor interlocking, which makes the person affected bite and chew disadvantageously. These include, for example, open bites or cross bites. Both groups of misalignments are treated by the orthodontist or in combination with the oral and maxillofacial surgeon.
What is a jaw cyst?
By definition, a cyst is a cavity lined with epithelial cells that have a tendency to spread. In this cavity there is liquid which, due to the osmotic pressure, attracts more and more liquid from the surrounding tissue. A jaw cyst usually occurs in the lower jaw and can take various forms.
One speaks of a radicular cyst when it arises around the root, which is probably the most common type of cyst. Furthermore, cysts tend to develop around displaced wisdom teeth. In general, cysts usually spread without symptoms, unless they press on nerve tissue, so that the patient feels painful or numb. If a cyst is diagnosed, it must be surgically removed.
The two surgical methods are the cystectomy and the cystostomy. With a cystostomy, the fluid is let out of the cavity through an access; with a cystectomy, the entire "cyst sac" is also removed. After the surgical treatment of the cyst, there is always a certain risk for the patient that a cyst will form again in the same place.
Jaw clamp
The jaw clamp is a symptom with many different potential causes. It has the effect that the affected person can no longer open their mouth.
- One reason for this can be cramping of the masticatory muscles. In this case one speaks of a trism.
- Furthermore, a scar, a change in the temporomandibular joint or the salivary glands can cause a jaw clamp.
- A fracture of the bony structures of the skull such as the zygomatic bone can trigger a clamp and prevent the mouth from opening.
- If one is anesthetized during dental treatment, the needle can also injure the muscle and form a bruise. This "Hematoma“Can also trigger a jaw clamp.
The jaw clamp can occur on one side or both.
Muscle-relaxing drugs that relieve tension in the muscles are often prescribed therapeutically. Physiotherapy and self-massaging exercises can also relieve symptoms.
In the event of fractures or other causes, the jaw clamp disappears when the actual cause is treated, for example with surgical fixation of the cheekbone fracture.
Lock jaw
The lock is the complete opposite of the clamp. When locking the jaw, the jaw closure is impaired and restricted and the patient's mouth is open. Possible causes for this can be broken jaws that impede the functions of the jaw. If these are surgically fixed and tightened with plates and screws, the symptoms also disappear.
Furthermore, the jaw head jumping out of the socket is also a reason for an open mouth. With this jaw dislocation, the symptoms disappear when the temporomandibular joint is dislocated. After a short rest, all functions of the jaw are restored.
Inflammation of the temporomandibular joint or wear and tear such as TMJ osteoarthritis are also possible causes of a locked jaw. After the inflammation has healed and the osteoarthritis has been treated, the symptoms usually disappear completely in these cases too and the jaw can be closed again.
See also under: Lock jaw
Temporomandibular joint pain

In addition to the teeth or gums, it is often the temporomandibular joint that can cause pain. Due to the many movements that it makes during the day, a pain in the jaw joint can limit everyday life. Chewing, speaking or just swallowing can be torture. The causes of this pain can be traced back to many possibilities.
The patient should pay attention to when they occur, for example in the morning or after eating. Is the pain only present in phases or is it permanent? Brusixmus can be a possible cause. This is a clenching or grinding of the teeth, which usually happens unnoticed and at night. It is triggered either by incorrectly fitting dentures or by mental suffering and a high level of stress. After getting up, the jaw appears tense and pain occurs. The muscles are also overloaded and feel rigid and tense.
Bacteria are often responsible for oral pain. These can also trigger pain in the temporomandibular joint. Bacteria continue to work their way through the tissue, attack the jawbone and can thus also spread to the joint. It should also be noted that the systematic destruction leads to incorrect loads within the chewing organ, for example due to the absence of a tooth, which causes the other teeth to begin to migrate.
This also shows another cause of pain in the temporomandibular joint, namely incorrect loading. This can either be caused naturally, through migration and tilting of teeth or through the eruption of the wisdom teeth. Prosthetic restorations that are not well-fitting can also be to blame, such as a crown that is too high / too deep, incorrect bridges or incorrectly fitting prostheses. The temporomandibular joint is permanently incorrectly stressed and manifests itself as pain.
This often leads to what is known as craniomandibular dysfunction. This is the malfunction of all parts of the jaw, such as muscles, bones and tissues. As in any other joint, permanent incorrect or incorrect loading can lead to arthritis in the temporomandibular joint, which can also cause very unpleasant pain. If left untreated, arthritis can develop into osteoarthritis and cause permanent damage.
The cause of the temporomandibular joint pain can also be general tension, especially in the spine, or a permanent incorrect load and incorrect posture. Cold-related pain in the face area can radiate into the joint. Side effects of TMJ problems are usually headache, neck pain and ear pain.
Read more on the topic: Temporomandibular joint pain and Pain in jaw and ear.
Therapy against temporomandibular joint pain
The simplest therapy is heat treatment. But it is often not enough. If the load is uneven due to differences in height of individual teeth, the teeth must be ground in. A bite splint can help with stress-related crunching that has led to an overload of the temporomandibular joint and the masticatory muscles. If there is cartilage damage, an operation is necessary. In most cases, it is sufficient to remove the disturbing cartilage particles or to smooth the frayed cartilage by means of arthroscopy, a minimally invasive procedure. The jaw clamp disappears as the temporomandibular joint inflammation subsides. The lock is removed by repositioning the jaw head that has jumped out.
How can I relax the jaw?
Most of the therapies aim to relax the jaw joint, teeth and muscles. Since the complex of the jaw works closely with the surrounding soft tissues, it is not possible to immediately categorize where the problem lies. A plastic splint is usually made for the night to prevent contact of the teeth and the clenching of the jaw. This allows the jaw, the masticatory muscles and the joint to relax.
External massage movements can also release tension and knots in the muscles and soft tissues, which also relax the jaw. Furthermore, targeted exercises can also provide relaxation.
One exercise involves opening the lower jaw against light pressure from the hands, holding this tension for 15 seconds and then releasing it. This targeted mouth opening should be repeated 10 times and trains the soft tissue with regular exercise. This can trigger a lasting relaxation of the jaw.
Exercises to relax the TMJ

Various exercises can be performed to relax the jaw joint a little.The muscles are particularly often very rigid and firm and can be loosened up a little with simple stretching and relaxation exercises. This also requires a watchful eye on the part of the patient, who controls himself and notices that the temporomandibular joint is very tense at the moment and that an exercise can help, such as after a stressful day in the office or an exam.
For most of the exercises, it is important to sit upright and straight and close your eyes to relax and concentrate fully on the exercises. You concentrate on the tension and on the movements, inhale deeply and forcefully. Massaging the muscles in the jaw area from the outside can be a starting point.
You begin by opening your mouth slowly and evenly, inhaling calmly and deeply and, in the open position, moving your lower jaw slightly to the right or left until the tension begins to loosen. One observes how smooth the movements are, whether a lot of force has to be used and whether it begins to move more fluently again. If things are a bit clumsy at the beginning, keep the mouth movements small, let them work and gradually open your mouth a little more. Next, you can easily stick your tongue out when opening it. Furthermore, it is possible to place the index and middle finger on the temporomandibular joint, tilt the head slightly, keep the shoulders lowered, keep the fingers in the same position and optionally massage briefly. The important thing is not so much the massage, but the feeling of relaxation. The lower jaw remains very loose. Then you rattle your teeth very gently and gently and let the relaxation flow through your whole head. Once the relaxation has spread to the head, it helps to gently massage the temples while breathing calmly and to gently circle the head in the next step.
In addition to relaxation exercises, there are also exercises that strengthen the muscles, and stimulate the oxygen supply and blood circulation. This includes an exercise in which you place your thumb from below on the outside of the center of your chin, open your mouth, but gently press against it with your thumb and hold it in the open position for 3-6 seconds. This can be repeated 2-5 times. For relaxation and stretching, an exercise can be used in which one hand presses the thumb against the upper incisors and with the other hand places the index and middle fingers on the lower front teeth. Now you open your mouth and press gently with your fingers. But it should be comfortable and painless. With it you stretch the muscles and enjoy the relaxation effect.
Diagnostic measures for the temporomandibular joint
Since temporomandibular joint pain can have many causes, a comprehensive examination is necessary. The patient's statements about the type, duration and intensity of the complaints provide initial indications of the cause. This is followed by an inspection of the oral cavity to determine any irregularities in the position of the teeth. An x-ray can reveal damage within the joint.
Summary
The Temporomandibular joint is a sliding and swivel joint that connects the upper and lower jaw. TMJ diseases can have very different causes. Therefore diagnosis is often difficult. The therapy depends on the causes and can therefore be very different. It ranges from heat therapy to surgical interventions.